Abstract
Purpose
To describe and validate a novel CT approach using volumetric analysis for renal stone surveillance.
Materials and methods
This prospective trial consisted of a standard low-dose non-contrast CT (SLD) of the abdomen and pelvis, immediately followed by an ultra-low-dose non-contrast CT (ULD) with reconstruction limited to the kidneys. A novel dedicated software tool was applied that automates stone volume, density, and maximum linear size. Manual linear stone size was measured by a radiology fellow and urology resident for comparison. CT dose and clinical charges were considered.
Results
Twenty-eight stones in 16 patients were analyzed. Mean effective dose of ULD CT was 0.57 mSv, an average 92% lower than the SLD CT dose. For SLD, mean size ± SD (range) (mm) was 7.9 ± 6.2 (2.6–30.5) for Reader 1, 7.3 ± 6 (2.4–30.7) for Reader 2, and 9.3 ± 6.4 (3.7–33.1) for the automated software. For ULD, mean size ± SD (range) (mm) was 7.3 ± 6 (2.5–30.5) for Reader 1, 7.2 ± 6.1 (2.1–30.7) for Reader 2, and 9.1 ± 6.4 (4.2–32.8) for the automated software. Automated stone diameters were larger than manual diameters for 27/28 stones (mean difference, 23%); difference was ≥ 2 mm in 30%. Average variability between manual measurements was 8.6% (SLD) and 7.8% (ULD), but was 0% for the automated technique. Our institutional charge for ULD renal CT is slightly less than renal US, and > 4× less than SLD CT. The Medicare global fee for the ULD renal CT is less than the SLD CT of the abdomen and pelvis.
Conclusions
This focused stone surveillance CT protocol is lower cost and lower dose compared to the standard CT approach. Automated assessment of stone burden provides improved reproducibility over manual linear measurement and offers the advantages of 3D measurements and volumetry. We now offer and perform this protocol in routine clinical practice for stone surveillance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Routine surveillance imaging plays an important role in the management of asymptomatic renal stones. Evaluating stone burden can identify patients at risk for future stone events and evaluate for treatment success [1,2,3]. Despite having lower sensitivity and specificity than CT, KUB and US are commonly used for stone surveillance, due in part to cost and availability [1, 4, 5]. Historically, higher radiation dose was a disadvantage of CT, but modern iterative reconstruction algorithms have allowed for dose reduction without sacrificing diagnostic confidence for detecting stones [6].
Renal stone burden is typically assessed by measuring stone diameter on the orthogonal views, but obtaining accurate and reproducible measurements can be challenging in stones with complex three-dimensional shapes. Prior studies have shown that volumetric automated analysis provides a more reproducible assessment of stones when compared to manual linear measurements [7, 8]. As a unique advantage to CT surveillance, volumetric assessment can also quantify total renal stone burden, which has been shown to be an independent predictor of future stone events [3].
The purpose of this article is to describe and validate an ultra-low-dose, limited coverage CT approach to renal stone surveillance (i.e., the limited renal CT) supplemented by volumetric analysis that provides a reproducible assessment of stones. Because coverage of this renal CT protocol is limited to the kidneys, this approach is best suited for the non-acute evaluation of renal stones.
Methods
We performed a HIPAA-compliant, IRB-approved prospective imaging study comparing concurrent standard low-dose and ultra-low-dose CT series. All subjects signed informed consent.
Patient population and CT protocol
The study group included outpatient adults with renal stones undergoing non-contrast CT evaluation. All CT scans were performed on a 64-detector-row Discover CT750 HD scanner (GE Healthcare) at 120 kV with variable tube current modulation (Smart mA). Immediately following the standard low-dose (SLD) non-contrast CT of the abdomen and pelvis, an ultra-low-dose series (ULD) was obtained with reconstruction limited to the level of the kidneys. Aggressive dose reduction of the ultra-low-dose series (target ~ 90%) was achieved by adjusting tube current range, slice thickness, and noise index (Table 1).
CT reconstruction and analysis
All images were reconstructed in 2.5 mm slice thickness at 1.25 mm intervals in the transverse (axial) and coronal planes. The SLD series was reconstructed using filtered-back-projection (FBP), and the ULD series was reconstructed using model-based iterative reconstruction (MBIR). The larger stones in each patient were selected as index stones for analysis.
On the SLD and ULD series, the diameter and density of the index stones were measured on soft tissue windows (window width/level: 400/50 HU) by an abdominal radiology fellow and a urology resident. The stone length was measured in the axial and coronal planes, and the larger of the two measurements was recorded as the maximum stone diameter. When measuring density, a region of interest was placed on the stone, and the maximum HU was recorded. For smaller stones, a single-point HU was recorded when the region of interest included tissue outside the stone. Images were presented in random order and were reviewed independently by the readers in separate sessions, blinded to the reconstruction technique and without simultaneous access to both series. A dedicated renal stone software tool (Ziosoft, Inc., Tokyo) was applied to each series and provided automated measurements of stone volume, maximum diameter, and density (clinical example in Fig. 1). This software tool uses a fixed attenuation threshold of 200 HU to automatically segment stones selected by the user.
Clinical example. Using a dedicated renal stone software tool (Ziosoft, Inc., Tokyo), the growth of a renal stone is quantified (table, left) and spatially demonstrated with 3D volume renderings (green, bottom right). The standard low-dose CT protocol was used for the exams in May 2016 and February 2017. When the stone diameter doubled (6.8 to 14.8 mm) on the February 2017 CT, stone volume increased by ~ 300% (49.6 to 200.3 mm3). The exam performed in December 2017 used the ultra-low-dose, limited coverage CT protocol and showed a 39% increase in linear size (14.8 to 20.7 mm) which corresponded to a 173% increase in volume (200.3 to 547.6 mm3)
Variability of measurements between reader 1 and reader 2 was assessed using the equation 100 × (|D1 – D2|)/Davg, where |D1 – D2| is the absolute difference in measurements and Davg is the average of D1 and D2. To assess the variability of the software tool, automated measurements were repeated for each stone and applied to the same equation. Variability of measurements between the SLD and ULD series was also calculated (100 X (|DSLD – DULD|)/Davg). Variability between the automated and manual measurements was calculated using the larger manual (LM) measurement between the two readers and the corresponding automated measurement (auto) (100 X (|DLM – Dauto|/Davg).
The volume CT dose index (CTDIvol,mGy) and dose-length product (DLP, mGy-cm) were recorded for the SLD and ULD series to demonstrate the level of dose reduction. Effective dose (mSv) was obtained from the dose-length product by use of the conversion factor of 0.015 mSv/(mGy × cm).
Institutional charges and Medicare reimbursement for non-contrast CT (limited abdominal and full abdominopelvic), renal US, and KUB were considered.
Results
Final cohort consisted of 28 renal calculi (mean size 7.7 mm; range 2.1–33.1 mm) in 16 patients (mean age 56.5 years; 8M/8F). The average effective dose of the ULD limited renal CT was 0.57 mSv, which is 92% lower than the SLD CT of the abdomen and pelvis (6.77 mSv) (Table 2).
Mean automated and manual stone diameter measurements are presented in Table 3. Variability of diameter measurements between the SLD and ULD series was higher for the manual technique (8.1% for Reader 1 and 8.2% for Reader 2, compared to 5.2% for the software tool). For the manual diameter measurements, variability between Reader 1 and Reader 2 was 8.6% on the SLD series and 7.8% on the ULD series. Variability was 0% for the automated software measurements on both series because repeated measurements of stones produced the same values.
Due to its 3D approach, the automated software diameter measurements were generally larger than the manual diameters. Figure 2 compares the larger manual diameter of the two readers and the automated diameter for each stone on the SLD and ULD series, demonstrating the size discrepancy between the two techniques (mean difference of 22.6% on SLD and 23.8% on ULD). Automated diameters were larger than manual diameters in 27/28 stones on both series with a difference of ≥ 2 mm in 8/28 stones on the SLD series and in 7/28 stones on the ULD series. Additionally, this comparison only accounts for the larger of the manual diameters obtained by the readers, so the size discrepancy is underestimated.
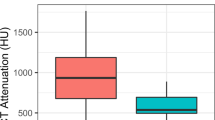
Mean ± SD (standard deviation) of manual density was 725 ± 636 HU (range 275–1175). Mean ± SD of automated density was 795 ± 580 HU (range 385–1204). Variability of density measurements between the SLD and ULD series was 18.1% for Reader 1, 16.9% for Reader 2, and 12.1% for the software tool. Both techniques produced the same density measurement on several stones (8/28 stones on SLD and 12/28 stones on ULD). Of the remaining stones, the automated density measurements were larger in roughly 50% (11/20 stones on SLD and 8/16 stones on ULD).
Mean ± SD of automated stone volume was 464.3 ± 1598 mm3 (range 7.2–8279 mm3) on the SLD series and 452.2 ± 1564 mm3 (range 5.6–8083) on the ULD series. Variability of the automated stone volumes between the SLD and ULD series was 11.9%.
According to the current Medicare Physician Fee Schedule, the global service fee for a limited CT or “Cat scan follow-up study” (CPT 76380) is $147.96 for our institution’s geographic location. This CPT code is used for our ultra-low-dose renal stone follow-up CT in clinical practice. The Medicare global service fee is $195.96 for unenhanced abdominopelvic CT (CPT 74176), $152.64 for unenhanced abdominal CT (CPT 74150), $116.28 for renal US (CPT 76770), and $27.72 for a single view KUB (CPT 74018) [9]. Our institutional charge for a limited, ultra-low-dose renal stone follow-up CT is slightly less than the charge for a renal US, about half of the charge for an unenhanced abdominal CT, and one-fourth of the charge for an unenhanced abdominopelvic CT.
Discussion
We demonstrate several advantages of using this limited CT protocol for renal stone surveillance, especially when automated volumetric evaluation is included. In our study, the manual linear measurements were less than the automated measurements of stone diameter for the vast majority of stones, and this discrepancy in size likely relates to the 3D capabilities of the software tool. While the manual technique is restricted to conventional CT planes, the software tool can measure stones in any spatial plane, providing greater accuracy, and is particularly beneficial when evaluating stones of complex shapes [7, 8]. The automated technique avoids the variability between readers because the software tool produces the same values when measurements are repeated on the same series. Integration of the automated technique into a surveillance program could potentially eliminate interobserver variability among radiologists and provide a more reproducible means for evaluating true interval change, the primary purpose of surveillance imaging.
Prior studies have described CT volumetry and the advantages of automated volumetric renal stone analysis [3, 7, 8, 10]. Volumetric analysis offers a more precise approach to complex stones, and longitudinal assessments of stone growth can now be reliably quantified. Using this technique, small incremental changes in linear size are more likely to be detected because changes in volume are comparatively amplified. The clinical example in Fig. 1 illustrates this concept where the doubling of stone size correlates with a volume increase of nearly 300%. Furthermore, stone volumetry may provide a metric with greater clinical implications than other radiographic measures. Selby et al. [3] found that automated total stone volume was more predictive of symptomatic stone events on multivariate analysis, independent of other imaging metrics, such as stone linear size and number. We include this analysis in our renal stone surveillance protocol, as it may be useful information when counseling patients with asymptomatic stones. Specifically, this information is useful in evaluating the success of medical management strategies [5].
Lowering CT dose is a priority in abdominal imaging, especially in stone patients who are often younger and will likely undergo serial exams. The lack of ionizing radiation is an advantage of US, but US does not provide the accuracy of CT [4] (Fig. 3). Our average effective dose for ultra-low-dose CT was 0.57 mSv, which is less than the reported average effective dose of a KUB (0.7 mSv) [11] and is 92% lower than the standard low-dose CT of the abdomen and pelvis. Good agreement between measurements on both series supports preserved diagnostic quality. It should be noted that because coverage is limited to the kidneys, this surveillance technique is meant for assessing renal stone burden in asymptomatic follow-up. This protocol would not be suitable for patients with acute flank pain when full coverage through the ureters and bladder is necessary.
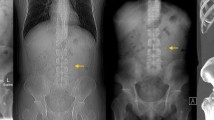
Clinical example. A A 55-year-old female underwent a standard CT of the abdomen and pelvis showing calculi in the right ureteropelvic junction and right lower pole which were subsequently treated with ureteroscopy and laser lithotripsy. DLP for this standard CT was 707 mGy-cm. Follow-up imaging was performed with B US and C KUB which demonstrated residual stones that were difficult to quantify by these modalities. D Eventually, the patient underwent a limited ultra-low-dose renal CT for follow-up which showed a decreased stone burden with smaller punctate right renal calculi. This limited protocol had a lower DLP of 88 mGy-cm
Both the Medicare global fee and our institutional charge for the limited renal CT are less than unenhanced abdominal CT and unenhanced CT of the abdomen and pelvis. The Medicare global fee for renal ultrasound is less than the limited renal CT, but our institutional charge for renal ultrasound is slightly more compared to the limited renal CT charge. In non-Medicare patients, the limited renal CT may be the less costly imaging test of the two.
We acknowledge several limitations. Our study lacks a true reference standard, as actual stone diameter and volume were not measured, and this study involves a small number of patients. The selected index stones were clearly visualized on both the SLD and ULD CT series, and the size and attenuation thresholds for automated software analysis in stones ≤ 2 mm were not assessed. It is possible that this ultra-low-dose protocol would not identify sub-2 mm stones at this aggressive level of dose reduction, which could lead to inaccuracies in reporting stone burden.
In summary, the limited renal stone CT protocol with automated analysis of stone burden that we describe provides a robust surveillance tool. This protocol maintains the benefits of CT evaluation but at a lower dose and lower cost compared with the standard CT approach. The addition of the automated volumetric analysis provides for a more reproducible stone assessment. For routine stone surveillance of asymptomatic individuals, we now offer and perform this CT protocol in clinical practice.
References
Fulgham PF, Assimos DG, Pearle MS, Preminger GM (2013) Clinical effectiveness protocols for imaging in the management of ureteral calculous disease: AUA technology assessment. J Urol. 189(4):1203–1213
Preminger GM, Tiselius HG, Assimos DG, et al. (2007) 2007 guideline for the management of ureteral calculi. J Urol. 178(6):2418–2434
Selby MG, Vrtiska TJ, Krambeck AE, et al. (2015) Quantification of asymptomatic kidney stone burden by computed tomography for predicting future symptomatic stone events. Urology. 85(1):45–50
Sternberg KM, Eisner B, Larson T, et al. (2016) Ultrasonography significantly overestimates stone size when compared to low-dose, noncontrast computed tomography. Urology. 95:67–71
Pearle MS, Goldfarb DS, Assimos DG, et al. (2014) Medical management of kidney stones: AUA guideline. J Urol. 192(2):316–324
Pooler BD, Lubner MG, Kim DH, et al. (2014) Prospective trial of the detection of urolithiasis on ultralow dose (sub mSv) noncontrast computerized tomography: direct comparison against routine low dose reference standard. J Urol. 192(5):1433–1439
Patel SR, Stanton P, Zelinski N, et al. (2011) Automated renal stone volume measurement by noncontrast computerized tomography is more reproducible than manual linear size measurement. J Urol. 186(6):2275–2279
Patel SR, Wells S, Ruma J, et al. (2012) Automated volumetric assessment by noncontrast computed tomography in the surveillance of nephrolithiasis. Urology. 80(1):27–31
Physician Fee Schedule Search (2018). https://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx. Accessed 7 May 2018
Demehri S, Kalra MK, Rybicki FJ, et al. (2011) Quantification of urinary stone volume: attenuation threshold-based CT method--a technical note. Radiology. 258(3):915–922
Mettler FA Jr, Huda W, Yoshizumi TT, Mahesh M (2008) Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 248(1):254–263
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by NIH grant R01 CA169331-01.
Conflict of interest
Pickhardt is co-founder of VirtuoCTC; consultant for Bracco and Check-Cap; and shareholder in Elucent, SHINE, and Cellectar. Lubner receives grant funding from Philips and Ethicon. Nakada is a consultant for Boston Scientific. Planz, Posielski, Li, and Chen declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Planz, V.B., Posielski, N.M., Lubner, M.G. et al. Ultra-low-dose limited renal CT for volumetric stone surveillance: advantages over standard unenhanced CT. Abdom Radiol 44, 227–233 (2019). https://doi.org/10.1007/s00261-018-1719-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1719-5