Abstract
Barium upper GI series performed by an interested and competent radiologist is still a very useful study to evaluate a variety of esophagogastric disorders. It usually provides information complementary to upper endoscopy and other foregut studies. Barium upper GI series is an important part of the diagnostic workup for gastroesophageal reflux disease, hiatal hernia, and esophageal motility disorders including achalasia. It is also an important part of the follow-up after operation for these common problems and after other operations such as resection or bariatric surgery. The GI radiologist should be an important member of the foregut surgery team.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
If a surgeon were limited to one and only one diagnostic study of the foregut, it would be barium upper gastrointestinal (GI) series. This study performed by an interested and competent radiologist can evaluate the esophagus, stomach, and duodenum for mucosal and submucosal lesions (tumors, polyps, ulcers, etc.), strictures (benign and malignant), leaks, diverticula, foreign bodies, obstruction, and motility disorders [1.] While admittedly it may not be the BEST study to evaluate the proximal alimentary tube for many of these problems, the noninvasiveness and ready availability of barium evaluation of the upper GI tract make this an essential diagnostic tool for surgeons [2.] Unfortunately it is often viewed as redundant to esophagogastroduodenoscopy. It is not redundant, but complementary to this and other diagnostic modalities useful in the management of patients with foregut symptoms (manometry, scintigraphy, pH studies, etc.).
Preoperative evaluation
While many patients present to the surgeons with a rather complete diagnostic workup, in the era of the internet patients with foregut symptoms often find their way to the surgeon without a diagnosis. Regardless of the differential diagnosis, barium upper GI series is an excellent study to start the diagnostic evaluation. Patients with foregut complaints and alarm features (weight loss, anemia or bleeding, dysphagia, odynophagia, palpable abdominal mass or lymphadenopathy, jaundice, strong family history) require upper endoscopy. But an initial barium study often yields the clinical diagnosis which can then be confirmed by additional focused testing and biopsy if indicated. In otherwise seemingly healthy patients with foregut symptoms, a barium study may provide inexpensive reassurance to both the patient and the surgeon. A healthy patient with recent heartburn may have only a sliding hiatal hernia with gastroesophageal reflux of barium on exam. If symptoms completely resolve with a short treatment course of proton pump inhibitor (PPI) and dietary modification, no additional testing is necessary. An elderly patient with longstanding mild dysphagia may demonstrate on barium esophagram cricopharyngeal dysfunction and a small Zenker’s diverticulum with an otherwise normal esophagus. Similarly, no additional testing is required.
Patients with already diagnosed esophagogastric or duodenal disease are often referred to a surgeon with a rather extensive workup that does not include barium upper GI series. But it is unusual for this study NOT to provide additional clinically useful information to the surgeon.
Dysphagia
Difficulty swallowing or the sensation of food sticking during deglutition can be caused by dysmotility or mechanical obstruction or both. Not uncommonly, patients referred to the surgeon have more than one problem that could cause dysphagia. For example, a patient referred for a large hiatal hernia diagnosed on esophagogastroduodenoscopy (EGD) and thought to be causing swallowing difficulty may have esophageal dysmotility or a small Zenker’s diverticulum on barium esophagram. Or a patient with a sliding hiatal hernia and Schatzki’s ring on EGD thought to be causing dysphagia may have evidence of oropharyngeal dysfunction on barium study. Or a patient with a small submucosal distal esophageal lesion on EGD, presumably a leiomyoma causing intermittent dysphagia, may have the picture of scleroderma esophagus on barium study. Nearly all patients with dysphagia who do not have cancer benefit from barium upper GI series [3,4,5,6,7].
Gastroesophageal reflux disease (GERD) and hiatal hernia
Barium upper GI series provides useful information to foregut surgeons contemplating operation for GERD and hiatal hernia. It is better than other diagnostic modalities for providing useful information about some issues [8,9,10]. Hernia type (sliding type 1 hiatal hernia vs. paraesophageal type 2–4 hiatal hernia) and hernia size are best delineated by barium study. The operation to repair a sliding hiatal hernia is fundamentally different from that required for a paraesophageal hernia. Large hiatal hernias, both sliding and paraesophageal, are associated with “short esophagus” and may require esophageal lengthening for durable repair [11]. The clinical significance of reflux stricture as well as location and dimensions are evaluable by barium esophagram too. While high-resolution esophageal manometry is the gold standard for evaluating esophageal motor disorders, oropharyngeal dysphagia and esophagotracheal aspiration are best evaluated with barium fluoroscopy [12, 13].
Achalasia
Esophageal dilation, tortuosity, and degree of obstruction and stasis are all readily evaluated by barium esophagram [14]. Although EGD and manometry are necessary for the complete evaluation of achalasia, operative planning can be facilitated by the barium study. The hugely dilated or tortuous serpentine esophagus is unlikely to respond to any operation except resection. Hiatal hernia may require repair concomitant with esophagomyotomy. Finally, it is generally recognized that comparison of preoperative and postoperative esophageal barium meniscus height is helpful in gauging the success of lower esophageal sphincter (LES) treatment in achalasia [15.]
Esophageal diverticulum
Proximal (Zenker’s) and distal (epiphrenic) diverticula are almost always solitary and associated with an underlying esophageal motor disorder [16]. Symptoms can be from the diverticulum (extrinsic pressure on the esophagus and stasis) or the dysmotility, but the relative contribution of either to the symptom complex is generally moot to the surgeon, since operation treats both (diverticulectomy is done concomitant with myotomy). However, the surgeon IS interested in the location, size, and degree of stasis associated with the diverticulum and all of these features can be defined on barium esophagram. A small wide mouthed Zenker’s diverticulum with only mild cricopharyngeal narrowing may not warrant operation, whereas a large chronically distended Zenker’s with extrinsic esophageal compression should respond well to operation. A large epiphrenic diverticulum just above the GE junction is easily approached with a laparoscopic transhiatal approach, but an epiphrenic diverticulum 10 cm above the GE junction would likely require a transthoracic approach.
Esophagogastric dysmotility
Esophageal motility disorders such as jackhammer esophagus (also referred to as nutcracker esophagus and diffuse esophageal spasm) or scleroderma esophagus have characteristic appearances on barium esophagram, and radiologic information thus obtained often complements data from high-resolution esophageal manometry [17]. Retained food in the stomach in the absence of gastric outlet narrowing may indicate gastroparesis which can cause or exacerbate an array of foregut symptoms.
Esophageal cancer
There are several features of esophageal cancer that are of interest to the surgeon and readily demonstrated on barium esophagram. The first is proximal and distal extent of the tumor. If the proximal extent of the tumor is near the carina, a transthoracic approach to resection is preferable to a transhiatal approach. If the tumor straddles the gastric cardia with a significant amount of tumor deformity in the stomach, standard transhiatal esophagogastrectomy with interposition of the residual gastric remnant may not be technically feasible since substantial or even total gastrectomy may be required. Significant angulation or change in the esophageal axis related to the esophageal cancer can be a sign of unresectability [18]. Finally, esophageal-airway fistulization is a sign of unresectability which is easily demonstrated with barium.
Gastric cancer
The extent of tumor involvement in the stomach is often best evaluated by barium fluoroscopy. Linnitus plastica suggests unresectability or the need for total gastrectomy. Encroachment on the duodenum by gastric tumor suggests that obtaining a negative duodenal margin may be difficult or impossible with standard radical gastrectomy. Similarly, proximal tumor encroachment on the esophagus may require extending the resection into the thoracic esophagus perhaps with the need for colon interposition. Thus, these findings may contraindicate operation in a high risk patient. Tumor perforation or fistulization indicates a T4 lesion.
Submucosal tumors
Most submucosal tumors of the esophagus, stomach, or duodenum are either gastrointestinal stromal tumors (GISTs) or leiomyoma’s, and the stomach is the most common location for both. GISTs should be removed if > 2 cm, while leiomyomas may be observed if not significantly symptomatic or rapidly enlarging. The ease and technical aspects of the operation depend upon the location of the tumor. In this regard, the information obtained from the barium upper GI series is always complementary to that obtained on EGD. Most submucosal tumors of the stomach can be wedged out, but large lesions or those in the juxtacardiac or antro-pyloric region may require formal segmental resection. Symptomatic esophageal leiomyomas are best enucleated with mucosal preservation. Operative planning is facilitated by localization on barium study [19].
Peptic ulcer
Surely all patients with endoscopically diagnosed peptic ulcer do not require barium upper GI series. But in the small subset of peptic ulcer patients who require surgical consultation, many will benefit from this study. A small percentage of patients with perforated peptic ulcer can be managed nonoperatively if they are nontoxic AND if the contrast study demonstrates sealing of the perforation. In patients with chronic gastric outlet obstruction thought to be secondary to peptic ulcer scarring, barium study can be helpful in suggesting a benign etiology, as well as in defining the extent and location of the stricture. Finally, in the unusual patient in whom operation is contemplated for intractable gastric ulcer, if the barium study suggests significant duodenal scarring, consideration should be given to adding a vagotomy since type 2 gastric ulcer should be treated surgically like duodenal ulcer.
Duodenal tumor
Duodenal adenocarcinoma is best treated with pancreaticoduodenectomy. But for tumors amenable to local resection, location and size are the most important parameters for operative planning. Barium duodenography is an excellent technique for obtaining this information, probably better than EGD, and complementary to computerized tomography (CT) scan.
Bariatric surgery evaluation
Before gastric sleeve resection or Roux Y gastric bypass (RYGBP) for severe obesity, it is important to evaluate the esophagus and stomach for pathology. Upper endoscopy is the test of choice, but barium upper GI study can yield additional valuable information. Large hiatal hernia may require simultaneous repair during bariatric operation, and significant GE reflux is a relative contraindication to sleeve gastrectomy. Evidence of peptic ulcer disease is a relative contraindication to gastric bypass since it renders the distal stomach and duodenum inaccessible. Polyps should be biopsied or removed preoperatively, and gastric or esophageal cancer obviously contraindicates bariatric operation.
Early postoperative evaluation
Upper GI contrast study of the upper GI tract done within 2 weeks of operation is generally performed to rule out leak or obstruction. Unless the risk of pulmonary aspiration is unusually high, water soluble contrast is used first. If no leak is identified, barium is then administered. When a leak is seen, the surgeon is interested in the location, the size, communication with the drain, free extravasation, and any evidence of ischemia. While the clinical condition of the patient is the primary determinant of the need for reoperation, the parameters mentioned are also important. CT scan and barium upper GI series are best used together to evaluate patients with suspected perforation or leak after foregut operation [20,21,22,23.]
The significance of obstruction to the flow of barium in the early postoperative period depends upon the operation and the condition of the patient. Early complete obstruction after fundoplication or hiatal hernia repair is an indication for urgent reoperation to rule out tight wrap, acute hiatal herniation, and/or tight hiatus. A similar finding after achalasia surgery is unusual and is an indication for urgent EGD and possible reoperation to rule out incomplete myotomy or tight wrap. Failure of barium to pass through an esophageal, gastric, or duodenal anastomosis may be due to mechanical or more commonly functional obstruction. Depending on the clinical scenario, gentle endoscopy may be indicated to confirm patency [24, 25].
Intermediate postoperative evaluation
Barium upper GI series to evaluate the anatomic and/or functional result of foregut operation is best delayed until 3 months after the operation, allowing the postoperative swelling, induration, and dysmotility to resolve. This is an excellent time to obtain a baseline postoperative study against which future barium studies can be compared if indicated by new or recurrent symptoms. This is especially true for patients who have had operation for achalasia, GERD, and hiatal hernia. Following myotomy for achalasia, particular attention is paid to esophageal emptying (“timed barium swallow”) and distention [26,27,28]. The caliber of the GE junction is also noted. After operation for GERD and hiatal hernia, it is important to note any residual hiatal hernia as well as the position of the wrap and any associated obstruction to esophageal outflow or angulation of the GE junction. It must be recognized that “abnormalities” identified of postoperative barium esophagram are often not associated with clinically significant symptoms [29]. Examples include hiatal hernia, GE reflux, esophageal dysmotility, and gastric retention of food. The surgeon is usually the best person to put the barium findings into perspective with the patient. Injudicious comments by a well-meaning radiologist (“you have a lot of reflux”; “you don’t have any reflux”; “you still have a hiatal hernia”; “you have food in your stomach so you must have gastroparesis”; “the GE junction is tight”; “the GE junction is patulous”) can cause unnecessary anxiety for the patient who then may require time-consuming reassurance by the surgeon for clinically irrelevant or expected findings.
Long-term follow-up
During long-term follow-up of patients who have had foregut operation for benign disease, routine barium studies are generally not indicated and are reserved for the patient with bothersome persistent or recurrent symptoms. Obviously it helps if a baseline postoperative study is available for comparison. Similarly, routine barium upper GI series is not indicated for most patients who have had operation for cancer. But sometimes barium study can elucidate suspicious or abnormal findings seen on routine follow-up CT or EGD.
Hiatal hernia repair and fundoplication
Patients with recurrent or new foregut symptoms months or years after hiatal hernia repair or fundoplication should have a barium upper GI series to look for an obvious cause [30]. Recurrent hiatal hernia or wrap slippage is the most common anatomic problems resulting in postoperative symptoms. “Wrap slippage” is a term that encompasses a variety of anatomic abnormalities better displayed on upper GI series than on EGD, including wrap disruption, wrap herniation into the mediastinum, and low wrap with stomach above. Other possible causes of recurrent symptoms seen on upper GI series include recurrent GE reflux, peptic stricture, gastroparesis (suggested by debris in stomach), secondary achalasia, and hiatal stenosis (more common when perihiatal mesh has been used). Common clinical questions for which barium study can help provide answers include (1) has the wrap herniated and/or is there a paraesophageal hernia? (2) Is there a stricture or is the wrap too tight? Patients in whom the long-term follow-up upper GI series strongly resembles the early postoperative upper GI series are unlikely to benefit from surgical revision, but those with significant anatomic changes might. Additional testing, such as EGD, esophageal manometry, gastric scintigraphy, and pH impedance testing, along with GI consultation should be done prior to reoperation [31, 32].
Achalasia
Patients with recurrent achalasia symptoms after Heller myotomy may have incomplete myotomy, peptic stricture, hiatal hernia, tight wrap, cancer, and/or progression of disease. While EGD and manometry are very important in evaluating recurrent post-treatment achalasia symptoms, barium esophagram is a critical test to help sort out this important differential diagnosis. Obviously the presence of a mucosal lesion mandates EGD and biopsy, but this is a rare finding. The most common causes of recurrent symptoms after Heller myotomy are GE reflux, peptic stricture, incomplete myotomy, tight wrap, and disease progression. Patients who have a wide open LES on barium study are unlikely to benefit from another assault on the LES, but they may have reflux esophagitis or progressive esophageal dilation as a cause of symptoms. If a narrowing is seen on barium study, the location is key. A narrowing in the distal mediastinal esophagus is likely to be a peptic stricture or less commonly cancer, while a narrowing in the gastric cardia is more likely to be an incomplete myotomy or a tight wrap.
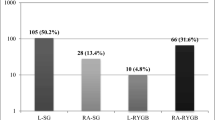
Bariatric surgery
Patients with upper GI symptoms months or years after obesity operation should be evaluated with barium upper GI. The likely cause of such symptoms obviously depends on the operation. After laparoscopic adjustable gastric band (LAGB), the most common cause of acute symptoms is band slippage or band erosion. The former may necessitate emergent operation because of the possibility of ischemic stomach. The most common cause of chronic symptoms after lap band is GE reflux or tight band.
Vertical banded gastroplasty (VBG) is rarely done nowadays, but there exists a cohort of patients who have had this operation. Chronic symptoms after this bariatric procedure are usually due to pouch dilation and angulation of the stoma resulting in solid food intolerance. This is readily demonstrated on barium study.
Patients with an acute abdomen months or years after RYGBP may have internal hernia or perforated marginal ulcer. CT scan is admittedly the test of choice in this situation and emergent operation can be life-saving [33, 34]. In patients with more chronic symptoms after gastric bypass, barium upper GI study is a very rational first test. Differential diagnosis includes marginal ulcer, gastro-gastric fistula (between the proximal gastric pouch and the bypassed stomach), GERD, hiatal hernia, strictured GJ anastomosis, Roux stasis or obstruction, strictured or obstructed jejunojejunostomy anastomosis, as well as chronic internal hernia. No single study comes close to barium fluoroscopy for evaluating all these important possibilities.
Summary
Over the last 20 years, barium upper GI series has been used less frequently to evaluate esophagogastric symptoms and disease. This is unfortunate since as described above, the barium study nearly always yields information complementary to EGD and other foregut studies. Often this information is critical for optimal surgical management of the patient. But the decline is understandable. Many patients and most radiologists prefer CT scan to upper GI series because it requires less effort by both the examiner and the examinee. Also often physicians and patients believe, mistakenly, that “high tech” is always better than “low tech.” And many clinicians also are mistaken that barium upper GI series and EGD are redundant. Furthermore, barium upper GI series is operator dependent and younger radiologists may be less experienced with this potentially valuable study because recently they have done few barium upper GI series in training and/or practice. Additionally across the whole spectrum of health care facilities nationally, the quality control with EGD far exceeds that for barium upper GI series. Finally, patients with GI symptoms come to see the gastroenterologist not the radiologist. For all these reasons, it is not surprising that nationwide the number of barium UGI studies has declined. But foregut surgeons and gastroenterologists specializing in foregut disease understand the need for quality barium foregut studies. They can and should help hospital administrators and radiology chairs understand their value. Without high-quality barium esophagogastrography, optimal care of patients with foregut disease will be difficult.
References
Levine MS, Rubesin SE, Laufer I (2009) Barium studies in modern radiology: do they have a role? Radiology 250(1):18–22
Levine MS, Rubesin SE (2005) Diseases of the esophagus: diagnosis with esophagography. Radiology 237(2):414–427
Jaffer NM, Ng E, Au FW, Steele CM (2015) Fluoroscopic evaluation of oropharyngeal dysphagia: anatomic, technical, and common etiologic factors. Am J Roentgenol 204(1):49–58
Hoy M, Domer A, Plowman EK, et al. (2013) Causes of dysphagia in a tertiary-care swallowing center. Ann Otol Rhinol Laryngol 122(5):335–338
Gullung JL, Hill EG, Castell DO, Martin-Harris B (2012) Oropharyngeal and esophageal swallowing impairments: their association and the predictive value of the modified barium swallow impairment profile and combined multichannel intraluminal impedance-esophageal manometry. Ann Otol Rhinol Laryngol 121(11):738–745
Carucci LR, Turner MA, Yeatman CF (2015) Dysphagia secondary to anterior cervical fusion: radiologic evaluation and findings in 74 patients. Am J Roentgenol 204(4):768–775
Bleier BS, Levine MS, Mick R, et al. (2007) Dysphagia after chemoradiation: analysis by modified barium swallow. Ann Otol Rhinol Laryngol 116(11):837–841
Jobe BA, Richter JE, Hoppo T, et al. (2013) Preoperative diagnostic workup before antireflux surgery: an evidence and experience-based consensus of the esophageal diagnostic advisory panel. J Am Coll Surg 217(4):586–597
Lacy BE, Weiser K, Chertoff J, et al. (2010) The diagnosis of gastroesophageal reflux disease. Am J Med 123(7):583–592
Levine MS, Carucci LR, DiSantis DJ, et al. (2016) Consensus statement of society of abdominal radiology disease-focused panel on barium esophagography in gastroesophageal reflux disease. Am J Roentgenol 207(5):1009–1015
Mattioli S, Lugaresi ML, Costantini M, et al. (2008) The short esophagus: intraoperative assessment of esophageal length. J Thorac Cardiovasc Surg 136(4):834–841
Hunt EB, Ward C, Power S, et al. (2017) The potential role of aspiration in the asthmatic airway. Chest 151(6):1272–1278
D’Alessio MJ, Rakita S, Bloomston M, et al. (2005) Esophagography predicts favorable outcomes after laparoscopic Nissen fundoplication for patients with esophageal dysmotility. J Am Coll Surg 201(3):335–342
Rohof WO, Hirsch DP, Kessing BF, Boeckxstaens GE (2012) Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology 143(2):328–335
Park YM, Jeon HH, Park JJ, et al. (2015) Correlation between timed barium esophagogram and esophageal transit scintigraphy results in Achalasia. Dig Dis Sci 60(8):2390–2397
Varghese TK, Marshall B, Chang AC, et al. (2007) Surgical treatment of epiphrenic diverticula: a 30 year experience. Ann Thorac Surg 84:1801–1809
Prabhakar A, Levine MS, Rubesin S, Laufer I, Katzka D (2004) Relationship between diffuse esophageal spasm and lower esophageal sphincter dysfunction on barium studies and manometry in 14 patients. Am J Roentgenol 183(2):409–413
Mariette C, Finzi L, Fabre S, et al. (2003) Factors predictive of complete resection of operable esophageal cancer: a prospective study. Ann Thorac Surg 75(6):1720–1726
Winant AJ, Gollub MJ, Shia J, et al. (2014) Imaging and clinicopathologic features of esophageal gastrointestinal stromal tumors. Am J Roentgenol 203(2):306–314
Upponi S, Ganeshan A, D’Costa H, et al. (2008) Radiological detection of post-oesophagectomy anastomotic leak - a comparison between multidetector CT and fluoroscopy. Br J Radiol 81(967):545–548
Cooke DT, Lin GC, Lau CL, et al. (2009) Analysis of cervical esophagogastric anastomotic leaks after transhiatal esophagectomy: risk factors, presentation, and detection. Ann Thorac Surg 88(1):177–184
Swanson JO, Levine MS, Redfern RO, Rubesin SE (2003) Usefulness of high-density barium for detection of leaks after esophagogastrectomy, total gastrectomy, and total laryngectomy. Am J Roentgenol 181(2):415–420
Carucci LR, Turner MA, Conklin RC, et al. (2006) Roux-en-Y gastric bypass surgery for morbid obesity: evaluation of postoperative extraluminal leaks with upper gastrointestinal series. Radiology 238(1):119–127
Levy JL, Levine MS, Rubesin SE, et al. (2016) Findings of esophagography for 25 patients after peroral endoscopic myotomy for Achalasia. Am J Roentgenol 207(6):1185–1193
Sternbach JM, El Khoury R, Teitelbaum EN, et al. (2015) Early esophagram in per-oral endoscopic myotomy (POEM) for achalasia does not predict long-term outcomes. Surgery 158(4):1128–1135
Kostic SV, Rice TW, Baker ME, et al. (2000) Timed barium esophagogram: a simple physiologic assessment for achalasia. J Thorac Cardiovasc Surg 120(5):935–943
Vaezi MF, Baker ME, Achkar E, Richter JE (2002) Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut 50(6):765–770
Boeckxstaens GE, Annese V, des Varannes SB, (European Achalasia Trial Investigators, et al. (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364(19):1807–1816
Dallemagne B, Kohnen L, Perretta S, et al. (2011) Laparoscopic repair of paraesophageal hernia. Long-term follow-up reveals good clinical outcome despite high radiological recurrence rate. Ann Surg 253(2):291–296
Baker ME, Einstein DM, Herts BR, et al. (2007) Gastroesophageal reflux disease: integrating the barium esophagram before and after antireflux surgery. Radiology 243(2):329–339
Lidor AO, Kawaji Q, Stem M, et al. (2013) Defining recurrence after paraesophageal hernia repair: correlating symptoms and radiographic findings. Surgery 154(2):171–178
Wehrli NE, Levine MS, Rubesin SE, Katzka DA, Laufer I (2007) Secondary achalasia and other esophageal motility disorders after laparoscopic Nissen fundoplication for gastroesophageal reflux disease. Am J Roentgenol 189(6):1464–1468
Lockhart ME, Tessler FN, Canon Cl, et al. (2007) Internal hernia after gastric bypass: sensitivity and specificity of seven CT signs with surgical correlation and controls. Am J Roentgenol 188:745–750
Patel RY, Baer JW, Texeira J, et al. (2009) Internal hernia complications of gastric bypass surgery in the acute setting: spectrum of imaging findings. Emerg Radiol 16:283–289
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There was no external funding for this work.
Conflict of Interest
Dr. Dempsey declares that he has no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by the author.
Rights and permissions
About this article
Cite this article
Dempsey, D.T. Barium upper GI series in adults: a surgeon’s perspective. Abdom Radiol 43, 1323–1328 (2018). https://doi.org/10.1007/s00261-018-1618-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1618-9