Abstract
This article presents methods to improve MR imaging approach of disorders of the renal sinus which are relatively uncommon and can be technically challenging. Multi-planar Single-shot T2-weighted (T2W) Fast Spin-Echo sequences are recommended to optimally assess anatomic relations of disease. Multi-planar 3D-T1W Gradient Recalled Echo imaging before and after Gadolinium administration depicts the presence and type of enhancement and relation to arterial, venous, and collecting system structures. To improve urographic phase MRI, concentrated Gadolinium in the collecting systems should be diluted. Diffusion-Weighted Imaging (DWI) should be performed before Gadolinium administration to minimize T2* effects. Renal sinus cysts are common but can occasionally be confused for dilated collecting system or calyceal diverticula, with the latter communicating with the collecting system and filling on urographic phase imaging. Vascular lesions (e.g., aneurysm, fistulas) may mimic cystic (or solid) lesions on non-enhanced MRI but can be suspected by noting similar signal intensity to the blood pool and diagnosis can be confirmed with MR angiogram/venogram. Multilocular cystic nephroma commonly extends to the renal sinus, however, to date are indistinguishable from cystic renal cell carcinoma (RCC). Solid hilar tumors are most commonly RCC and urothelial cell carcinoma (UCC). Hilar RCC are heterogeneous, hypervascular with epicenter in the renal cortex compared to UCC which are centered in the collecting system, homogeneously hypovascular, and show profound restricted diffusion. Diagnosis of renal sinus invasion in RCC is critically important as it is the most common imaging cause of pre-operative under-staging of disease. Fat is a normal component of the renal sinus; however, amount of sinus fat correlates with cardiovascular disease and is also seen in lipomatosis. Fat-containing hilar lesions include lipomas, angiomyolipomas, and less commonly other tumors which engulf sinus fat. Mesenchymal hilar tumors are rare. MR imaging diagnosis is generally not possible, although anatomic relations should be described to guide diagnosis by percutaneous biopsy or surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Disorders of the renal sinus represent a broad spectrum of diseases ranging from congenital to vascular to inflammatory and neoplastic conditions. Moreover, renal sinus disorders are much less frequently encountered on imaging studies when compared to their more common renal cortical counterparts [1]. A potential unfamiliarity with renal sinus diseases and a more varied differential diagnosis for renal sinus pathologies present a diagnostic challenge to interpreting radiologists. Magnetic resonance imaging (MRI) of the disorders of the renal sinus may further complicate interpretation due to technical pitfalls which may be encountered if MR imaging is not optimized. The purpose of this review article is to define the anatomy and normal structures encompassing the renal sinus, review a comprehensive MR imaging protocol which optimizes the imaging of renal sinus diseases, and present a contemporary illustration of the spectrum of renal sinus pathologies that may be encountered on MR imaging and an approach to facilitate imaging diagnoses. An emphasis on staging of renal cell carcinoma (RCC) and the importance of renal sinus invasion as well as discrimination between hilar RCC and urothelial cell carcinomas (UCC) are also presented as these are critically important concepts in urological oncology.
MR imaging and normal anatomy of the renal sinus
Normal anatomy of the renal sinus
The renal sinus is the medial compartment, consisting of the central cavity, of the kidneys. The sinus is formed by the extension of the perinephric space into the medial deep recess of the kidney. The entrance to the renal sinus is referred to as the renal hilum. The renal cortex lining the renal sinus does not have a well-defined capsule; however, there is a thick capsule which lines the pelvicalyceal structures and the renal pyramids. Contents of the renal sinus include the renal arteries, veins, major and minor calyces (as well as the renal pelvis and proximal ureter in most patients), nerves, lymphatics, and fibroadipose tissue (Fig. 1). Classically, the structures of the renal hilum are, from anterior to posterior, a single renal vein, a single renal artery, and the renal pelvis [2]. Due to the presence of major vascular and lymphatic drainage of kidneys, the renal sinus acts as a major route for metastatic dissemination in malignancies.
A twenty-three-year-old male undergoing MRI for suspected sclerosing cholangitis. Axial T2-weighted (T2W) single-shot fast/turbo spin echo (ssFSE/HASTE) (A) shows a normal fluid-filled renal pelvis in the renal sinus (arrow) with a signal intensity similar to that of the surrounding renal sinus fat. Axial T2W fat-suppressed ssFSE/HASTE (B) better depicts the renal pelvis (arrow) after suppression of the surrounding fat. Axial 3-Dimensional T1W Gradient recalled echo (GRE) after administration of gadolinium during the corticomedullary (CM) (C) and equilibrium/nephrographic (NG) (D) phases of enhancement show the normal contents of the renal sinus, namely, normal renal artery (arrow in c.) and renal vein (arrow in d.) respectively. Axial 10 min delayed T1 W GRE obtained during the urographic (UG) phase (E) of enhancement shows the renal sinus is obscured by severe susceptibility artifacts (arrow). This is due to the T2* effects of concentrated gadolinium in the collecting system which renders assessment of the renal sinus non-diagnostic. Axial b1000 mm2/s echo-planar image (EPI) (F) which was acquired after gadolinium administration shows similar susceptibility artifacts and geometric distortions (arrow) which renders the assessment of the renal sinus impossible. These artifacts can be mitigated by using intravenous hydration, diuretic administration, half-dose gadolinium, and acquisition of diffusion sequences prior to contrast administration. The use of Gadoxetic acid has also been described to ameliorate UG phase imaging with MRI
Optimizing an MRI protocol to evaluate for renal sinus disorders
Among the imaging modalities, MRI is ideally suited to evaluate renal sinus disorders, due to: higher spatial resolution, non-ionizing nature of the examination, better localization of tumor to the correct anatomic compartment, better depiction of intratumoral lipid and fat as well as availability of functional information including diffusion-weighted imaging. MR evaluation of renal hilar disorders can generally be adequately obtained using existing up-to-date multi-parametric renal MRI protocols, the details of which have been described previously [3, 4]; however, a few important modifications are necessary to maintain image quality and enable accurate assessment of disease processes and their relation to normal structures within the renal sinus. At least two planes of T2-weighted (T2W) half-acquisition single-shot Turbo/Fast spin echo (HASTE/SSFSE) are required when assessing the renal sinus because it is critical to determine whether a disease process is truly originating within the sinus (e.g., epicenter of the disease is in the renal sinus) compared to being secondarily invaded or infiltrated by a process originating in the renal cortex, perinephric fat, or retroperitoneum (e.g., epicenter of the disease is not in the renal sinus). This distinction is important and often best obtained on multi-planar T2W HASTE/SSFSE imaging because of the optimal depiction of the relevant anatomy and because HASTE/SSFSE imaging is robust against motion artifacts even in patients who cannot adequately suspend respiration. In a minority of cases, obtaining true short- and long-axis views in oblique planes may provide additional information; however, the expected minimal incremental gain compared to standard 3-plane imaging must be balanced with potential image degradation due to prolonged examination times. Balanced steady-state free precession (bSSFP; True-FISP/FIESTA) imaging can be useful when imaging the renal sinus because of its inherent bright blood effects and higher signal-to-noise ratio and spatial resolution compared to HASTE/SSFSE [5]. Another advantage of bSSFP when imaging the renal sinus is that it can help differentiate flow-related artifacts due to mobile urine in the collecting system from renal calculi and other filling defects [6, 7]. 3-Dimension (3D) T1W gradient recalled echo (GRE) in-phase and opposed phase chemical shift MRI and fat-suppressed sequences with volume interpolation/acceleration (VIBE/LAVA) should be acquired before and after Gadolinium administration. T1W chemical shift MRI combined with fat-suppressed imaging ensures that renal sinus processes containing fat will be adequately characterized. Gadolinium-enhanced images should be acquired dynamically in the corticomedullary, nephrographic, and particularly when imaging the sinus in the urographic phase of enhancement. Like T2W-MRI, multi-planar acquisition of T1 W MRI is important to delineate anatomic relations and the different phases of enhancement enable evaluation of hilar arterial, venous, and collecting system structures and how they relate to the hilar disease. Acquisition of pre- and post-gadolinium images using 3-Dimensional GRE provide the added benefit that oblique imaging planes may be obtained by post-processing of source data if required. Obtaining adequate MR urographic phase imaging can be challenging and methods to improve image quality for MR Urography have been detailed elsewhere [8]. Briefly, to enable accurate depiction of the renal collecting system in the urographic phase of enhancement, the T2* effects of concentrated Gadolinium (as it accumulates in the collecting system) must be accounted for, especially on 3T, to prevent susceptibility artifacts or blooming from obscuring evaluation [9] (Fig. 1). The use of intravenous hydration, diuretic administration, and half-dose Gadolinium administration can all be used to mitigate these effects [4]. The use of Gadoxetate disodium has also been described to decrease susceptibility artifacts due to its lower renal excretion [10]. Alternatively, MR urography using heavily T2-weighted imaging may be alternatively considered or added as an adjunct to gadolinium-enhanced MRU; however, it is inferior to enhanced MRU for discrimination between the varied renal hilar conditions subsequently described in this article.
Diffusion-weighted imaging (DWI) has become an important adjunct in the imaging of renal masses and is considered a fundamental component of a multi-parametric MR renal protocol [3]. DWI can be particularly useful for differentiating between hilar renal cell carcinoma and urothelial cell carcinoma discussed later, a distinction which has profound clinical implications. Most clinical DWI in the abdomen is currently acquired using single-shot echo-planar imaging (EPI) techniques which are extremely sensitive to the susceptibility effects of concentrated gadolinium in the collecting system and which can produce severe geometric warping/distortion artifact in addition to severe blooming artifact (Fig. 1). For this reason, when imaging the renal sinus, DWI should be performed before Gadolinium is injected or at the minimum before it concentrates in the collecting system to reduce unwanted susceptibility artifact encountered on EPI. The optimal order of sequences for renal sinus MRI protocol and sample sequence parameters have been demonstrated in Tables 1 and 2.
Approach to the imaging diagnosis of renal sinus disorders
Determining the origin of disease (hilar primary origin vs cortical/extrarenal secondary invasion)
A broad spectrum of benign and malignant diseases may involve the renal sinus, either arising primarily from renal sinus structures themselves or secondarily extending into the sinus from the adjacent cortex or retroperitoneum [11]. Review of multi-planar sequences in at least two planes usually is sufficient to distinguish primary hilar pathologies from secondary involvement. Taking care to determine the epicenter of the lesion helps localize the tumor in the correct compartment [11]. The distinction can be critical as it will form the basis of an imaging differential diagnosis.
Fat-containing lesions: approach to fatty lesions of the renal sinus
There is a growing body of evidence pointing to the importance of renal sinus fat in various diseases such as hypertension and renal injury [12, 13]. In participants from the Framingham Heart Study, quantification of renal sinus fat was independently associated with blood pressure measurements and renal function [13]. Studies have also suggested the central role renal sinus fat may play in the development of obesity-induced renal damage [14, 15]. MR spectroscopy and advanced Dixon-based sequences such as proton density fat fraction (PDFF) are now commercially available and can be used to segment and quantify renal sinus fat and are currently considered the gold standard for quantification of visceral fat [16, 17]. The amount of normal renal sinus fat therefore varies from patient to patient but should not be confused with renal replacement lipomatosis and renal sinus lipomatosis which are due to fat proliferation in the renal sinus secondary to calculus disease or processes causing renal atrophy [18].
Detection of lipid within renal sinus neoplasms also helps formulate a diagnosis for fat/lipid-containing neoplasms. MR can accurately identify lesions in the renal sinus which contain intracytoplasmic lipid (such as clear cell RCC) and lesions containing bulk or macroscopic fat such as lipoma (Fig. 2), angiomyolipoma (AML) (Fig. 3), and less commonly liposarcoma and extra-adrenal myelolipoma. Angiomyolipoma can be differentiated from liposarcoma by the presence of a “claw sign” or a “feeding vessel sign” with the underlying renal cortex and by the absence of calcification [19]. Centrally located RCCs and oncocytomas located in the renal sinus region have been previously shown to potentially engulf renal sinus fat and therefore may appear to have bulk or macroscopic internal fat on imaging thereby mimicking a diagnosis of angiomyolipoma [20, 21].
A thirty-year-old female with incidentally detected renal mass on ultrasound. Axial T2W ssFSE/HASTE image (A) shows increased T2W signal intensity well-circumscribed mass (arrow) in the renal hilum. Axial T1W GRE in-phase (IP) (B) image (arrow) shows the mass is isointense to retroperitoneal fat. On corresponding axial T1 W GRE opposed phase (OP) (C) image (arrow), there is no etching artifact where the mass interfaces with the retroperitoneal fat and on axial T1 W chemically fat-suppressed GRE image (D) there is complete loss of signal (arrow) thereby confirming the presence of bulk or macroscopic fat. Axial (E) and coronal (F) T1W GRE UG phase images show the mass (arrows) is separate from the collecting system without any enhancing solid component. Multiple biopsies from the nodule confirmed a diagnosis of lipoma without features of liposarcoma and the mass was stable on follow-up imaging for several years (not shown)
A sixty-three-year-old female with pre-surgical MRI for known renal mass. Axial T1W GRE IP image shows a large well-circumscribed heterogeneous mass in the left renal hilum (arrow) with increased signal intensity which is isointense to the subcutaneous fat. Marked areas of etching artifact are observed on Axial T1W GRE OP image (B) (arrow) within the mass and corresponding axial fat-only image (derived from 2-point Dixon technique) (C) confirms that the mass consists of predominantly bulk or macroscopic fat (arrow). Axial T1W GRE FS image (D) shows areas of increased T1W signal intensity in keeping with hemorrhage and there is marked enhancement within this portion of the mass on gadolinium-enhanced T1W GRE image obtained during the NG phase of enhancement (E) (arrow). Pre-operative angiography (F) reveals innumerable small aneurysms within the mass (arrow) which are characteristic of angiomyolipoma. Subsequent nephrectomy and histopathology confirmed angiomyolipoma
Xanthogranulomatous pyelonephritis (XGP) is a rare form of chronic pyelonephritis which is characterized by lipid-laden foamy macrophages at histopathology; however, fat is only rarely, if ever, identified on imaging studies [22, 23]. The imaging diagnosis is instead usually readily established with the presence of the characteristic staghorn calculus and other characteristic MR imaging findings including restricted diffusion in the dilated calyces (having a classic ‘bear’s paw’ configuration) (Fig. 4).
A forty-three-year-old female with known renal stone disease. Axial unenhanced CT image (A) shows a large staghorn calculus (arrow). Axial T1W GRE (B) and axial T2W ssFSE/HASTE re-demonstrate the calculus (white arrows in B and C) and also better depict dilated fluid-filled calyces in a ‘bear’s paw’ configuration (black arrows in B and C). Axial ADC map (D) shows profound restricted diffusion within the calyces (arrow). Combined, the features are diagnostic of xanthogranulomatous pyelonephritis. The diagnosis was subsequently proven at histopathology after nephrectomy
Renal sinus cystic lesions
Most cystic lesions encountered in the renal sinus on imaging studies are due to benign parapelvic or peripelvic cysts (Fig. 5). Parapelvic cysts are usually single larger cysts presenting in the renal sinus most likely originating from the renal parenchyma, whereas peripelvic cysts are multiple confluent irregularly shaped cysts originating from lymphatic channels in the renal sinus itself. The encompassing term ‘renal sinus cyst’ may be used when it is occasionally not possible to differentiate between the two types on imaging. [24]. Occasionally other pathologies can mimic renal sinus cysts. MR helps to further characterize the nature of these less common cystic lesions which are usually incidentally detected.
A sixty-nine-year-old female with incidentally identified renal cysts on an MRI performed for evaluation of the pancreatic duct. Coronal T2W FS ssFSE/HASTE image (A) shows multiple simple cysts pointing towards the renal hilum (arrow) which are also well demonstrated on the thick slab maximum intensity projection (MIP) images (B) obtained from FS heavily T2W MRCP (arrow). Coronal T1W GRE NG phase (C) image shows no enhancing solid component (arrow) and axial ADC map (D) shows “T2 shine through” with increased signal intensity and no areas of restricted diffusion (arrow). Imaging features are classic for renal sinus cysts, most likely peripelvic cysts
A ballooned or blown out renal pelvis or calyces in adult patients usually stems from a congenital ureteropelvic junction obstruction (or transition) and can mimic a large parapelvic cyst on both ultrasound and CT [25, 26]. MR urographic phase imaging is diagnostic as it depicts contrast within a dilated pelvis which communicates with the collecting system. MR angiography can demonstrate a responsible crossing vessel as a potential cause in a minority of cases [27]. Strictures or sequelae from prior obstruction or infection can give a similar appearance at the calyceal level and the presence of intracystic calculi which can be identified on fluid sensitive sequences (but to lesser extent than with CT) and more importantly contrast filling on MR urographic phase establishes a diagnosis of calyceal diverticulum [28] (Fig. 6).
A thirty-five-year-old female with incidentally detected symptomatic complex renal sinus cyst on CT, MRI was suggested for further assessment. Axial T2W ssFSE/HASTE (A) and axial T1W GRE (B) show a lesion with characteristics compatible with cyst containing layering-dependent debris or calculi (arrows in A and B). Axial T1W GRE CM phase image (C) shows no enhancing solid component (arrow). Axial T1W GRE UG phase image (D) shows gadolinium accumulation within the cyst (arrow) confirming a diagnosis of a large calyceal diverticulum and not a renal sinus cyst. Fluoroscopic image from percutaneous nephrolithotomy (E) shows a needle placed within the diverticulum with the injected contrast outlining the diverticulum (white arrow) and the collecting system (black arrow). Neo-infundibulotomy was performed under fluoroscopic guidance and the urothelium was fulgurated using a resectoscope and cautery loop
Cystic nephroma is a complex benign cystic renal neoplasm that appears as a Bosniak Type III cystic lesion on imaging [29] and occurs most commonly in young boys and middle-aged female patients [30] with a reported propensity to herniate into the renal sinus and renal pelvis [31] (Fig. 7). MRI can reliably demonstrate the cystic nature of the tumor and depict renal sinus herniation [32]; however, imaging diagnosis remains limited as both of these features can be seen in other cystic masses including cystic RCC. Reporting herniation of tumor into the renal sinus is crucial if surgery is planned, as surgical techniques need to be modified accordingly [33]. In one study by Balyemez et al., DWI was helpful to differentiate cystic nephroma from cystic RCC; however, that study was limited by small sample sizes (< 10 lesions in either group) [34, 35]. The internal contents of a cystic nephroma may show variably high signal intensity on T1 W images due to the presence of internal hemorrhage and proteinaceous material [36]. Gadolinium-enhanced MRI with subtraction imaging performs better than CT for the identification of enhancing septal and solid components in hemorrhagic lesions [37].
A forty-four-year-old female with complex cystic lesions in the kidney and spleen detected on CT with suspicion of echinococcal disease, MRI was suggested for further evaluation. Coronal steady-state free precession (bSSFP) image (A) and axial FS T2W FSE image (B) show a complex cystic mass with multiple thin internal septations. The medial component of the cystic mass herniates into the renal sinus (arrows in A and B). Based on the presence of internal septae with measurable enhancement as depicted on coronal (C) and axial (D) FS T1W GRE gadolinium-enhanced images (arrows in C and D), a diagnosis of a Bosniak Type 3 cystic lesion was provided. Subsequent nephrectomy was performed and final histopathology revealed a diagnosis of multilocular cystic nephroma
Renal sinus vascular lesions
MRI is also helpful to differentiate other conditions of the renal sinus which may mimic sinus cysts. Large partially thrombosed renal aneurysms and arteriovenous malformations are occasionally misdiagnosed as complex cystic masses on ultrasound either due to lack of Doppler evaluation or due to large thrombosed component or calcification which limits visibility [38, 39]. These vascular lesions can occasionally also mimic renal neoplasms especially if incidentally discovered on an unenhanced or uniphasic-enhanced CT [40, 41] (Fig. 8). Multiphasic MRI accurately establishes diagnosis, and other important information can be derived from MR angiography including the exact vessel of origin of the aneurysm, size of aneurysm neck, and percentage of non-thrombosed portion. In aneurysms in which therapy is not contemplated, or in aneurysms which measure between 1 and 1.5 cm, MR can be used for surveillance [42]. Moreover, MRI can also provide helpful clues potentially elucidating the etiology of the aneurysm; for example, aneurysms associated with ‘string of beads’ appearance of the main or segmental arteries on MR angiography suggest a diagnosis of fibromuscular dysplasia [43], while the presence of bilateral microaneurysms suggests polyarteritis nodosa [44, 45]. Lastly, MRI can potentially diagnose other benign vascular tumors originating in the renal sinus such as hemangioma due to their characteristic high signal intensity on T2W, absence of restricted diffusion and characteristic appearance on multiphasic gadolinium-enhanced images with a progressive centripetal fill-in similar to hepatic hemangiomas and enhancement which follows the blood pool [46] (Fig. 9). A failure to suggest hemangioma on imaging studies would result in misdiagnosis as RCC and potentially result in total nephrectomy [47].
A sixty-four-year-old female with right flank pain. Axial unenhanced renal colic protocol CT image (A) shows a nodule in the renal sinus with peripheral calcification (arrow) concerning for a solid renal mass and renal protocol MR was suggested for further characterization. Axial bSSFP (B) “bright-blood” image shows the nodule in direct communication with the right renal artery (arrow) and demonstrating similar signal intensity to the blood pool (compare signal to the aorta [arrowhead], for example). Axial FS T1W GRE gadolinium-enhanced images in the angiographic C and CM phase D demonstrate enhancement paralleling the blood pool and communication with the renal artery (arrows in C and D) thereby confirming a narrow-neck renal artery aneurysm. Due to size between 1 and 1.5 cm, conservative management was selected
A thirty-six-year-old female with hematuria. Axial unenhanced renal colic protocol CT image A shows a homogeneous nodule in the renal sinus (arrow) with a 10 mm calculus in a mid-pole lateral calyx (arrowhead). Axial contrast-enhanced CT UG phase image B shows solid enhancement within a portion of the nodule (arrow). Axial FS T2W ssFSE/HASTE image C shows that the nodule has homogeneous increased T2W signal intensity (arrow). Coronal FS T1W gadolinium-enhanced GRE images in the CM phase (D), portal venous phase (E), and NG phase (F) show progressive fill-in of the nodule with signal intensity paralleling the blood pool. The nodule was stable without any interval growth over a 12-year follow-up period. Lack of growth and imaging characteristics are consistent with hemangioma
Hilar RCC versus urothelial cell carcinoma (UCC)
Among malignant neoplasms of the genitourinary tract, both RCC and UCC are encountered in the renal sinus and are by far the most common malignant neoplasms which involve the renal sinus [48, 49]. Although RCCs are predominantly cortical, a proportion of RCCs may extend into the renal sinus [50]. Differentiation between UCC arising from the pelvis or calyceal system and central RCC with renal sinus invasion is particularly important because of differences in prognosis and management [51, 52]. UCC portends relatively poor prognosis and usually warrants nephroureterectomy with removal of bladder cuff [53], whereas RCC carries a more relatively favorable prognosis and can be managed by either radical nephrectomy or nephron sparing surgery depending on size and stage of the disease (the latter likely not possible with renal sinus involvement) [54].
Differentiating features having moderate to good levels of diagnostic accuracy have been described on MRI to differentiate between clear cell subtype of RCC and UCC. RCC is usually centered within the renal parenchyma, whereas UCC has its epicenter located in the collecting system [55]. RCC is more heterogeneous compared to UCC with internal necrotic areas or cystic changes. In addition to subjective assessment, internal heterogeneity can be further quantified using histogram and texture analysis [56]. Hemorrhage which can be depicted on MRI as areas of T1W hyperintensity within the mass is relatively common with RCC, and is almost never found with UCC [57, 58]. Approximately 30%–60% of clear cell RCCs (and 15% of papillary RCC) may show intracellular lipid on chemical shift-based MR pulse-sequences as a signal intensity drop on opposed phase compared to in-phase images, whereas UCC should not contain lipid [59,60,61]. While RCCs are identified as well-circumscribed nodular masses, UCC when it invades the kidney tends to preserve the normal shape of the kidney [55]. Following gadolinium administration, RCC (especially the most common clear cell variant) shows arterial hypervascularity and heterogeneous enhancement compared to UCC which are characteristically hypovascular and show relatively homogenous enhancement. MR urography depicts UCC as polypoidal filling defects or masses within the collecting system, whereas RCC usually only produces distortion of the collecting system due to extrinsic mass effect [62]. On DWI, UCC shows profoundly restricted diffusion, and quantitative assessment shows a comparatively lower normalized ADC for UCC when contrasted with RCC [63] (Figs. 10 and 11). The above features are useful in differentiation of the most common clear cell subtype of RCC from UCC. Other subtypes of RCC like papillary and chromophobe RCC, have MRI features which may overlap with UCC and differentiation may be difficult.
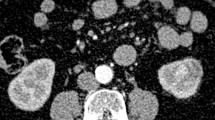
A sixty-three-year-old man with renal mass identified on ultrasound. Coronal T2W ssFSE/HASTE (A) reveals a heterogeneous signal intensity renal mass protruding into the renal sinus (arrow). Axial ADC map (B) shows mild restricted diffusion (arrow.) within the mass. Axial FS gadolinium-enhanced T1W GRE images obtained during the CM phase (C) and NG phase (D) demonstrate marked hyperenhancement (arrow) with washout of contrast (arrow); characteristic features of clear cell RCC. The medial extension of tumor and possibility of renal sinus invasion was not reported. Low-microscopic power hematoxylin and eosin-stained histopathology image demonstrates clear cell renal cancer (white arrow) with invasion into the renal sinus (black arrow) in keeping with T3a disease
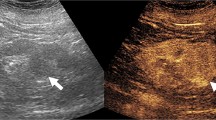
A Fifty-four-year-old male with hematuria undergoing MR urography. Axial T2W ssFSE/HASTE image (A) shows a homogeneously low T2W signal intensity mass (arrow) centered in the renal sinus. Axial ADC map image (B) shows profound restricted diffusion (arrow). Coronal (C) and axial (D) FS T1W GRE gadolinium-enhanced images during the CM phase (C) and NG phase (D) show the hypovascular homogeneous enhancement of the mass which is centered in the renal collecting system (arrows in C and D). Nephroureterectomy was performed and histopathology confirmed urothelial cell carcinoma
Other rare forms of centrally infiltrating tumors can also be potentially diagnosed with MRI. Collecting duct carcinomas present as hypovascular, T2W hypointense infiltrative masses with cystic components arising from renal medulla [64, 65]. Squamous cell carcinomas which are usually secondary to chronic irritation by renal calculi may present as heterogeneous hypovascular masses associated with renal stones [66]. Lastly, lymphoma may appear as a homogenously enhancing infiltrating sheet-like mass or masses with enhancement said to be less than that of adjacent renal cortex and with marked restricted diffusion [67] (Fig. 12). Inflammatory pseudotumor and other fibrosing conditions of the hilar or perinephric spaces could mimic hilar malignancy but are generally diagnosed histologically and not prospectively diagnosed with imaging without any contributing clinical history.
A seventy-year-old man with constitutional symptoms and renal mass identified on ultrasound. Coronal T2W ssFSE/HASTE image (A) shows a homogenous mass infiltrating the kidney and extending into the renal sinus (arrow). Axial ADC map image (B) reveals profound restricted diffusion (arrow). Coronal FS T1W GRE gadolinium-enhanced image (C) during the NG phase shows low-level homogenous enhancement of the mass (arrow) which is less than the enhancement of the adjacent renal cortical parenchyma (arrowhead). Note how the mass infiltrates the kidney but preserves its reniform shape. Percutaneous biopsy was performed which revealed non-Hodgkin’s lymphoma. Due to the absence of involvement elsewhere in the body, this was classified as a case of primary renal lymphoma. The mass disappeared following chemotherapy (radiological complete response) and unenhanced CT (D) performed after completion of treatment shows complete resolution of the mass with a residual atrophic kidney (arrow)
Staging of RCC: implications of renal sinus invasion
In addition to having diagnostic implications, extension of RCC into the renal sinus has significant therapeutic and prognostic implications. Even with T1 tumors it is known that hilar location of RCC is associated with higher recurrence rates and that attempted partial nephrectomy is associated with poor recurrence-free survival when compared to radical nephrectomy [68]. Hilar location is also a known as a common cause for upstaging of a clinical T1 tumor to pathological T3a tumor after surgery [69]. Accurate pre-operative knowledge of renal sinus extension is a critical determining factor between radical nephrectomy and nephron sparing surgery; for example, current guidelines support the use of nephron sparing surgery only in T1/T2 tumors [70]. Renal sinus extension is the most common cause of intraoperative conversion of partial to radical nephrectomy [71].
Renal sinus invasion is considered the principal route of extrarenal extension of RCC due to the rich supply of small veins and lymphatics located in the renal sinus [72]. RCCs with size larger than 4 cm have 6 times higher frequency of sinus invasion when compared with smaller masses [73]. Anatomically the renal sinus is not separated from the renal cortex by a fibrous capsule [74], therefore, any signs of direct abutment of RCC with the renal sinus fat without normal intervening cortical parenchyma should be considered to represent renal sinus invasion (Fig. 10). This is in contrast to perinephric fat invasion, where a circumscribed, pushing tumor border that only protrudes into the perinephric fat beyond the normal outline of renal cortex may not necessarily constitute perinephric fat invasion due to the intact renal capsule which acts as a constraint for tumor spread and impedes growth to surrounding tissue [74, 75].
According to the current TNM system of staging of RCC, both renal sinus fat invasion and perinephric fat invasion are categorized under stage T3a. There is a growing body of evidence disputing the prognostic equivalence between the two forms of tumor spread with literature indicating that renal sinus invasion is an independent predictor of lower cancer-specific survival compared to perinephric fat invasion [76, 77]. In addition, patients with renal sinus fat infiltration also have higher Fuhrman nuclear grade, increased incidence of lymph node metastasis, increased rates of sarcomatoid differentiation and tumor necrosis; all of which are associated with higher rates of recurrence and poor prognosis [76].
MRI has an American College of Radiology (ACR) appropriateness criteria rating of 8/9 for staging of RCC [78]. Evaluation of tumor abutment or extension into renal sinus fat is critical; however, it is reported that diagnostic accuracy for sinus invasion by RCC with imaging is only modest [79]. Due to the low accuracy of imaging for diagnosis of sinus fat invasion, pathologic upstaging after surgery predominantly occurs from underestimating sinus fat involvement [80, 81] and patients who are upstaged after partial nephrectomy tend to have poorer oncologic outcomes [82, 83]. Multiple nephrometry scoring systems which have been developed, including the R.E.N.A.L. (Radius. Exophytic/endophytic. Nearness to sinus. Anterior/Posterior. Location relative to polar lines) and P.A.D.U.A. (pre-operative aspects and dimensions used for anatomic classification) scores, can be used to overcome this shortcoming [84, 85]. For example, three of the 4 scored components of R.E.N.A.L. and 4 of the 6 scored components of the P.A.D.U.A. systems pertain directly or indirectly to proximity with renal sinus, underscoring the importance of this finding. Higher scores in both nephrometry scoring systems have been associated with pathologic upstaging after nephrectomy, tumor recurrence after ablation and intraoperative conversion of nephron sparing surgery to nephrectomy [86,87,88].
Renal vein invasion is also an important prognostic factor in RCC [89]. Assessment is usually performed using post gadolinium-enhanced T1W images which can be used to detect frank venous invasion by tumor and to document the extent of thrombus. Bright blood bSSFP sequences are also helpful in patients to assess patency of renal vein when gadolinium is contraindicated or was not administered. Segmental vein involvement has been classified as T3a disease [90] and careful assessment on thin section images is crucial to detect early involvement. In a study by Karlo et al., a tumor-to-sinus distance of 0 mm measured on T2W sequences was highly sensitive and specific for muscular vein branch invasion [91].
Not unlike renal sinus fat invasion, invasion into the pelvicalyceal system may also provide additional independent prognostic value. The latest 2017 American Joint Committee on caner 8th edition cancer staging manual has newly added invasion of pelvicalyceal system in stage T3a [90]. Therefore, every effort must be made to detect calyceal invasion on MR urographic phase images.
Mesenchymal neoplasms
A spectrum of benign and malignant mesenchymal neoplasms can occur in the renal sinus including fibroma, leiomyoma, neurogenic tumors, teratoma, leiomyosarcoma, fibro sarcoma, rhabdomyosarcoma, hemangiopericytoma, and malignant fibrous histiocytoma [46]. Owing to the relative rarity of these neoplasms, imaging characteristics have not been well described and usually overlap with the more common renal or urothelial carcinomas. An accurate pre-surgical diagnosis is therefore not typically possible although sarcomas have been described as large hypovascular masses with epicenter in the renal sinus [92] (Fig. 13). MRI still plays a role in local staging of mesenchymal neoplasms by delineating the extent and identifying local invasion [93]. This information is important for the surgeon in deciding between the various therapeutic choices and may also help guide percutaneous biopsy attempts at histological diagnoses.
A seventy-seven-year-old female with incidental renal mass identified on ultrasound. Axial (A) and coronal (B) T2W ssFSE/HASTE images show a large heterogeneous mass with epicenter in the renal hilum (arrows in A and B). FS T1W GRE gadolinium-enhanced axial NG phase (C) and coronal UG phase (D) images show the hypovascular nature of the mass (arrows in C and D). Malignant fibrous histiocytoma was identified at histopathology after resection
Conclusion
In conclusion, MRI is valuable for diagnosis of renal sinus disorders when performed correctly to optimize imaging and with a systematic approach to diseases which may involve the renal sinus. An up-to-date multi-parametric MRI protocol of the kidneys is sufficient to evaluate most renal sinus diseases but should specifically include multi-planar imaging and consider the effects of concentrated Gadolinium when evaluating the collecting system and performing DWI as both urographic phase T1W GRE and EPI sequences are degraded by T2* effects of concentrated Gadolinium in the collecting systems. The majority of cystic and fat-containing renal sinus diseases can be diagnosed accurately with MRI; however, cystic nephroma remains indistinguishable from cystic RCC based upon imaging features alone. Vascular lesions should always be considered when evaluating suspected renal sinus masses. Mesenchymal tumors arising from the renal hilum occur but are rare and imaging diagnosis is generally not possible although descriptions of local extent can facilitate biopsy and surgical planning. Differentiating hilar RCC from UCC is of paramount importance due to differences in treatment and patient prognosis and a provisional diagnosis can be suspected in most cases. For RCC, involvement of the renal sinus fat and muscle containing venous branches has important prognostic implications and significantly upstages disease, and these two findings should be critically assessed on pre-operative MR imaging studies to provide accurate clinical staging.
References
Pallwein-Prettner L, Flory D, Rotter CR, et al. (2011) Assessment and characterisation of common renal masses with CT and MRI. Insights Imaging 2(5):543–556
Klatte T, Ficarra V, Gratzke C, et al. (2015) A literature review of renal surgical anatomy and surgical strategies for partial nephrectomy. Eur Urol 68(6):980–992
Ramamurthy NK, Moosavi B, McInnes MD, Flood TA, Schieda N (2015) Multiparametric MRI of solid renal masses: pearls and pitfalls. Clin Radiol 70(3):304–316
Chung AD, Schieda N, Shanbhogue AK, et al. (2016) MRI evaluation of the urothelial tract: pitfalls and solutions. AJR Am J Roentgenol 207(6):W108–W116
Chavhan GB, Babyn PS, Jankharia BG, Cheng HL, Shroff MM (2008) Steady-state MR imaging sequences: physics, classification, and clinical applications. Radiographics 28(4):1147–1160
Kalb B, Sharma P, Salman K, et al. (2010) Acute abdominal pain: is there a potential role for MRI in the setting of the emergency department in a patient with renal calculi? J Magn Reson Imaging 32(5):1012–1023
Schieda N, Isupov I, Chung A, Coffey N, Avruch L (2017) Practical applications of balanced steady-state free-precession (bSSFP) imaging in the abdomen and pelvis. J Magn Reson Imaging 45(1):11–20
Leyendecker JR, Barnes CE, Zagoria RJ (2008) MR urography: techniques and clinical applications. Radiographics 28(1):23–46 (discussion 46–27)
O’Connor OJ, McLaughlin P, Maher MM (2010) MR Urography. AJR Am J Roentgenol 195(3):W201–W206
Dym RJ, Chernyak V, Rozenblit AM (2013) MR imaging of renal collecting system with gadoxetate disodium: feasibility for MR urography. J Magn Reson Imaging 38(4):816–823
Rha SE, Byun JY, Jung SE, et al. (2004) The renal sinus: pathologic spectrum and multimodality imaging approach. Radiographics 24(Suppl 1):S117–S131
Chughtai HL, Morgan TM, Rocco M, et al. (2010) Renal sinus fat and poor blood pressure control in middle-aged and elderly individuals at risk for cardiovascular events. Hypertension 56(5):901–906
Foster MC, Hwang SJ, Porter SA, et al. (2011) Fatty kidney, hypertension, and chronic kidney disease: the Framingham Heart Study. Hypertension 58(5):784–790
Krievina G, Tretjakovs P, Skuja I, et al. (2016) Ectopic adipose tissue storage in the left and the right renal sinus is asymmetric and associated with serum kidney injury molecule-1 and fibroblast growth factor-21 levels increase. EBioMedicine 13:274–283
Irazabal MV, Eirin A (2016) Role of renal sinus adipose tissue in obesity-induced renal injury. EBioMedicine 13:21–22
Graffy PM, Pickhardt PJ (1062) Quantification of hepatic and visceral fat by CT and MR imaging: relevance to the obesity epidemic, metabolic syndrome and NAFLD. Br J Radiol 2016(89):20151024
Reeder SB, Hu HH, Sirlin CB (2012) Proton density fat-fraction: a standardized MR-based biomarker of tissue fat concentration. J Magn Reson Imaging 36(5):1011–1014
Karasick S, Wechsler RJ (2000) Case 23: replacement lipomatosis of the kidney. Radiology 215(3):754–756
Ellingson JJ, Coakley FV, Joe BN, et al. (2008) Computed tomographic distinction of perirenal liposarcoma from exophytic angiomyolipoma: a feature analysis study. J Comput Assist Tomogr 32(4):548–552
Curry NS, Schabel SI, Garvin AJ, Fish G (1990) Intratumoral fat in a renal oncocytoma mimicking angiomyolipoma. AJR Am J Roentgenol 154(2):307–308
Prando A (1991) Intratumoral fat in a renal cell carcinoma. AJR Am J Roentgenol 156(4):871
Dani R, Gandhi V, Prajapati H, et al. (2005) Case report: Xanthogranulomatous pyelonephritis—an unusual variety. Indian J Radiol Imaging 15(2):195–198
Verswijvel G, Oyen R, Van Poppel H, Roskams T (2000) Xanthogranulomatous pyelonephritis: MRI findings in the diffuse and the focal type. Eur Radiol 10(4):586–589
Amis ES Jr, Cronan JJ (1988) The renal sinus: an imaging review and proposed nomenclature for sinus cysts. J Urol 139(6):1151–1159
Tarzamni MK, Sobhani N, Nezami N, Ghiasi F (2008) Bilateral parapelvic cysts that mimic hydronephrosis in two imaging modalities: a case report. Cases J 1(1):161
Ma TL, Neild GH (2013) Parapelvic cyst misdiagnosed as hydronephrosis. Clin Kidney J 6(2):238–239
El-Nahas AR, Abou El-Ghar ME, Refae HF, Gad HM, El-Diasty TA (2007) Magnetic resonance imaging in the evaluation of pelvi-ureteric junction obstruction: an all-in-one approach. BJU Int 99(3):641–645
Stunell H, McNeill G, Browne RF, Grainger R, Torreggiani WC (2010) The imaging appearances of calyceal diverticula complicated by uroliathasis. Br J Radiol 83(994):888–894
Lane BR, Campbell SC, Remer EM, et al. (2008) Adult cystic nephroma and mixed epithelial and stromal tumor of the kidney: clinical, radiographic, and pathologic characteristics. Urology 71(6):1142–1148
Li Y, Pawel BR, Hill DA, Epstein JI, Argani P (2017) Pediatric cystic nephroma is morphologically, immunohistochemically, and genetically distinct from adult cystic nephroma. Am J Surg Pathol 41(4):472–481
Wood CG, Stromberg LJ, Harmath CB, et al. (2015) CT and MR imaging for evaluation of cystic renal lesions and diseases. Radiographics 35(1):125–141
Kettritz U, Semelka RC, Siegelman ES, Shoenut JP, Mitchell DG (1996) Multilocular cystic nephroma: MR imaging appearance with current techniques, including gadolinium enhancement. J Magn Reson Imaging 6(1):145–148
Lebed B, Jani SD, Kutikov A, Iffrig K, Uzzo RG (2010) Renal masses herniating into the hilum: technical considerations of the “ball-valve phenomenon” during nephron-sparing surgery. Urology 75(3):707–710
Balyemez F, Aslan A, Inan I, et al. (2017) Diffusion-weighted magnetic resonance imaging in cystic renal masses. Can Urol Assoc J 11(1–2):E8–E14
Ozturk M, Ekinci A, Elbir SF, et al. (2017) Usefulness of apparent diffusion coefficient of diffusion-weighted imaging for differential diagnosis of primary solid and cystic renal masses. Polish J Radiol 82:209–215
Silver IM, Boag AH, Soboleski DA (2008) Best cases from the AFIP: Multilocular cystic renal tumor: cystic nephroma. Radiographics 28(4):1221–1225 (discussion 1225–1226)
Muglia VF, Westphalen AC (2014) Bosniak classification for complex renal cysts: history and critical analysis. Radiol Brasileira 47(6):368–373
Silver PR, Budin JA (1990) Unusual manifestations of renal artery aneurysms. Urol Radiol 12(2):80–83
Vitale V, Di Serafino M, Vallone G (2013) Renal artery aneurysm mimicking a solid parenchymal lesion. J Ultrasound 16(3):131–134
Wong C, Leveillee RJ, Yrizarry JM, Kirby K (2002) Arteriovenous malformation mimicking a renal-cell carcinoma. J Endourol 16(9):685–686
Vasavada SP, Manion S, Flanigan RC, Novick AC (1995) Renal arteriovenous malformations masquerading as renal cell carcinoma. Urology 46(5):716–721
Khosa F, Krinsky G, Macari M, Yucel EK, Berland LL (2013) Managing incidental findings on abdominal and pelvic CT and MRI, Part 2: white paper of the ACR Incidental Findings Committee II on vascular findings. J Am Coll Radiol 10(10):789–794
Willoteaux S, Faivre-Pierret M, Moranne O, et al. (2006) Fibromuscular dysplasia of the main renal arteries: comparison of contrast-enhanced MR angiography with digital subtraction angiography. Radiology 241(3):922–929
Ozaki K, Miyayama S, Ushiogi Y, Matsui O (2009) Renal involvement of polyarteritis nodosa: CT and MR findings. Abdom Imaging 34(2):265–270
Norwood MGA, Salem MK, Markose G, Naylor AR (2009) Renal artery aneurysms: careful investigation is critical. EJVES Extra 18(3):38–40
Katabathina VS, Vikram R, Nagar AM, et al. (2010) Mesenchymal neoplasms of the kidney in adults: imaging spectrum with radiologic-pathologic correlation. Radiographics 30(6):1525–1540
Takaoka E, Sekido N, Naoi M, et al. (2008) Cavernous hemangioma mimicking a cystic renal cell carcinoma. Int Journal Clin Oncol 13(2):166–168
Decastro GJ, McKiernan JM (2008) Epidemiology, clinical staging, and presentation of renal cell carcinoma. Urol Clin N Am 35(4):581–592
Munoz JJ, Ellison LM (2000) Upper tract urothelial neoplasms: incidence and survival during the last 2 decades. J Urol 164(5):1523–1525
Bonsib SM, Gibson D, Mhoon M, Greene GF (2000) Renal sinus involvement in renal cell carcinomas. Am J Surg Pathol 24(3):451–458
Izumi K, Saito K, Nakayama T, et al. (2017) Contact with renal sinus is a significant risk factor for metastasis in pT1 clear cell renal cell carcinoma. Eur Urol 16(3):e1124–e1126
Hall MC, Womack S, Sagalowsky AI, et al. (1998) Prognostic factors, recurrence, and survival in transitional cell carcinoma of the upper urinary tract: a 30-year experience in 252 patients. Urology 52(4):594–601
Latchamsetty KC, Porter CR (2006) Treatment of upper tract urothelial carcinoma: a review of surgical and adjuvant therapy. Rev Urol 8(2):61–70
Jonasch E, Gao J, Rathmell WK (2014) Renal cell carcinoma. BMJ 349:g4797
Raza SA, Sohaib SA, Sahdev A, et al. (2012) Centrally infiltrating renal masses on CT: differentiating intrarenal transitional cell carcinoma from centrally located renal cell carcinoma. AJR Am J Roentgenol 198(4):846–853
Just N (2014) Improving tumour heterogeneity MRI assessment with histograms. Br J Cancer 111(12):2205–2213
Xing W, He X, Kassir MA, et al. (2013) Evaluating hemorrhage in renal cell carcinoma using susceptibility weighted imaging. PLoS ONE 8(2):e57691
Murray CA, Quon M, McInnes MD, et al. (2016) Evaluation of T1-weighted MRI to detect intratumoral hemorrhage within papillary renal cell carcinoma as a feature differentiating from angiomyolipoma without visible fat. AJR Am J Roentgenol 207(3):585–591
Moosavi B, Shabana WM, El-Khodary M, et al. (2016) Intracellular lipid in clear cell renal cell carcinoma tumor thrombus and metastases detected by chemical shift (in and opposed phase) MRI: radiologic-pathologic correlation. Acta Radiol 57(2):241–248
Schieda N, van der Pol CB, Moosavi B, et al. (2015) Intracellular lipid in papillary renal cell carcinoma (pRCC): T2 weighted (T2W) MRI and pathologic correlation. Eur Radiol 25(7):2134–2142
Jhaveri KS, Elmi A, Hosseini-Nik H, et al. (2015) Predictive value of chemical-shift MRI in distinguishing clear cell renal cell carcinoma from non-clear cell renal cell carcinoma and minimal-fat angiomyolipoma. AJR Am J Roentgenol 205(1):W79–W86
Silverman SG, Leyendecker JR, Amis ES Jr (2009) What is the current role of CT urography and MR urography in the evaluation of the urinary tract? Radiology 250(2):309–323
Wehrli NE, Kim MJ, Matza BW, et al. (2013) Utility of MRI features in differentiation of central renal cell carcinoma and renal pelvic urothelial carcinoma. AJR Am J Roentgenol 201(6):1260–1267
Pickhardt PJ, Siegel CL, McLarney JK (2001) Collecting duct carcinoma of the kidney: are imaging findings suggestive of the diagnosis? AJR Am J Roentgenol 176(3):627–633
Zhu Q, Wu J, Wang Z, et al. (2013) The MSCT and MRI findings of collecting duct carcinoma. Clin Radiol 68(10):1002–1007
Kalayci OT, Bozdag Z, Sonmezgoz F, Sahin N (2013) Squamous cell carcinoma of the renal pelvis associated with kidney stones: radiologic imaging features with gross and histopathological correlation. J Clin Imaging Sci 3:14
Prasad SR, Humphrey PA, Menias CO, et al. (2005) Neoplasms of the renal medulla: radiologic-pathologic correlation. Radiographics 25(2):369–380
Shim M, Song C, Park S, et al. (2015) Hilar location is an independent prognostic factor for recurrence in T1 renal cell carcinoma after nephrectomy. Ann Surg Oncol 22(1):344–350
Gorin MA, Ball MW, Pierorazio PM, et al. (2013) Outcomes and predictors of clinical T1 to pathological T3a tumor up-staging after robotic partial nephrectomy: a multi-institutional analysis. J Urol 190(5):1907–1911
Maroni P, Moss J (2014) Nephron-sparing surgery. Seminars Interv Radiol 31(1):104–106
Petros FG, Keskin SK, Yu K-J, et al. (2017) Intraoperative conversion from partial to radical nephrectomy: Predictive factors and outcomes. J Clin Oncol 35:483–483
Bonsib SM (2004) The renal sinus is the principal invasive pathway: a prospective study of 100 renal cell carcinomas. Am J Surg Pathol 28(12):1594–1600
Bonsib SM (2005) T2 clear cell renal cell carcinoma is a rare entity: a study of 120 clear cell renal cell carcinomas. J urol 174(4 Pt 1):1199–1202 (discussion 1202)
Trpkov K, Grignon DJ, Bonsib SM, et al. (2013) Handling and staging of renal cell carcinoma: the International Society of Urological Pathology Consensus (ISUP) conference recommendations. Am J Surg Pathol 37(10):1505–1517
Samaratunga H, Gianduzzo T, Delahunt B (2014) The ISUP system of staging, grading and classification of renal cell neoplasia. J Kidney Cancer VHL 1(3):26–39
Zhang Z, Yu C, Velet L, et al. (2016) The difference in prognosis between renal sinus fat and perinephric fat invasion for pT3a renal cell carcinoma: a meta-analysis. PLoS ONE 11(2):e0149420
Bertini R, Roscigno M, Freschi M, et al. (2009) Renal sinus fat invasion in pT3a clear cell renal cell carcinoma affects outcomes of patients without nodal involvement or distant metastases. J Urol 181(5):2027–2032
Vikram R, Beland MD, Blaufox MD, et al. (2016) ACR appropriateness criteria renal cell carcinoma staging. J Am Coll Radiol 13(5):518–525
Hallscheidt PJ, Bock M, Riedasch G, et al. (2004) Diagnostic accuracy of staging renal cell carcinomas using multidetector-row computed tomography and magnetic resonance imaging: a prospective study with histopathologic correlation. J Comput Assist Tomogr 28(3):333–339
Pruthi DK, Chhibba R, Drachenberg DE, McGregor T (2015) Renal nephrometry score and predictors of pathologic upstaging in patients undergoing partial and radical nephrectomies. J Clin Oncol 33:412
Goel MC, Mohammadi Y, Sethi AS, Brown JA, Sundaram CP (2008) Pathologic upstaging after laparoscopic radical nephrectomy. J Endourol 22(10):2257–2261
Mouracade P, Kara O, Dagenais J, et al. (2017) Perioperative morbidity, oncological outcomes and predictors of pT3a upstaging for patients undergoing partial nephrectomy for cT1 tumors. World J Urol 35:1425–1433
Nayak JG, Patel P, Saarela O, et al. (2016) Pathological upstaging of clinical T1 to pathological T3a renal cell carcinoma: a multi-institutional analysis of short-term outcomes. Urology 94:154–160
Parsons RB, Canter D, Kutikov A, Uzzo RG (2012) RENAL nephrometry scoring system: the radiologist’s perspective. AJR Am J Roentgenol 199(3):W355–W359
Okhunov Z, Rais-Bahrami S, George AK, et al. (2011) The comparison of three renal tumor scoring systems: C-Index, P.A.D.U.A., and R.E.N.A.L. nephrometry scores. J Endourol 25(12):1921–1924
Tay MH, Thamboo TP, Wu FM, et al. (2014) High R.E.N.A.L. Nephrometry scores are associated with pathologic upstaging of clinical T1 renal-cell carcinomas in radical nephrectomy specimens: implications for nephron-sparing surgery. J Endourol 28(9):1138–1142
Camacho JC, Kokabi N, Xing M, et al. (2015) R.E.N.A.L. (Radius, exophytic/endophytic, nearness to collecting system or sinus, anterior/posterior, and location relative to polar lines) nephrometry score predicts early tumor recurrence and complications after percutaneous ablative therapies for renal cell carcinoma: a 5-year experience. J Vasc Interv Radiol 26(5):686–693
Kobayashi K, Saito T, Kitamura Y, et al. (2013) The RENAL nephrometry score and the PADUA classification for the prediction of perioperative outcomes in patients receiving nephron-sparing surgery: feasible tools to predict intraoperative conversion to nephrectomy. Urol Int 91(3):261–268
Wagner B, Patard JJ, Mejean A, et al. (2009) Prognostic value of renal vein and inferior vena cava involvement in renal cell carcinoma. Eur Urol 55(2):452–459
Robins DJ, Small AC, Amin MB, et al. (2017) MP86-17 THE 2017 American Joint Committee on Cancer Eighth Edition Cancer Staging Manual: Changes in Staging Guidelines for Cancers of the Kidney, Renal Pelvis and Ureter, Bladder, and Urethra. J Urol 197(4):1163
Karlo CA, Di Paolo PL, Donati OF, et al. (2013) Renal cell carcinoma: role of MR imaging in the assessment of muscular venous branch invasion. Radiology 267(2):454–459
Lalwani N, Prasad SR, Vikram R, et al. (2011) Pediatric and adult primary sarcomas of the kidney: a cross-sectional imaging review. Acta Radiol 52(4):448–457
Nikolaidis P, Gabriel H, Khong K, et al. (2008) Computed tomography and magnetic resonance imaging features of lesions of the renal medulla and sinus. Curr Probl Diagn Radiol 37(6):262–278
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this manuscript.
Conflict of interest
None of the authors declare any conflicts of interests.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Krishna, S., Schieda, N., Flood, T.A. et al. Magnetic resonance imaging (MRI) of the renal sinus. Abdom Radiol 43, 3082–3100 (2018). https://doi.org/10.1007/s00261-018-1593-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1593-1