Abstract
Purpose
To determine the performance accuracy of 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) after primary tumor treatment for both bladder cancer (BC) and upper tract urothelial cancer (UTUC). To compare the accuracy of FDG PET/CT with that of contrast-enhanced-ceCT and magnetic resonance imaging (MRI).
Methods
Data of patients with recurrent urothelial carcinomas (UC) after primary treatment were collected in a retrospective, international multicenter study. Inclusion criteria were (1) patients with a known history of UC in the BC and/or in the UTUC; (2) PET/CT images after curative intent treatment of the primary tumor; (3) conventional imaging modalities (abdominal ceCT or MRI, or total body ceCT, and chest X-ray: called C.I.) performed no more than 3 months from PET/CT; (4) available standard of reference (e.g., histological data or follow-up imaging modalities) for the validation of PET/CT findings. Exclusion criteria were other abdominal tumors, chemotherapy administration prior to and/or concomitant to imaging, and non-urothelial histologic variants. Sensitivities, specificities, positive, and negative predictive values were evaluated for all patients and separately for bladder and UTUC.
Results
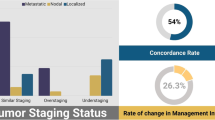
Overall, 287 patients were enrolled. Two-hundred thirteen patients underwent cystectomy (74.2%), 35 nephroureterectomy (12.2%), 31 both cystectomy + nephroureterectomy (10.8%), 5 both cystectomy + conservative treatment for UTUC (1.4%), and 3 (1%) other types of nephron-sparing treatments for UTUC. Neoadjuvant and adjuvant treatments were performed in 36 (12.5%) and 111 (38.7%) patients, respectively. Sensitivity and specificity (95% confidence intervals) of PET/CT for the detection of recurrent UC were 94% (91% to 96%) and 79% (68% to 88%), respectively. However, sensitivity was higher for BC than UTUC (95% vs. 85%) while specificity was lower in BC (78% vs. 85% for BC and UTUC, respectively). PET/CT and C.I. findings were available in 198 patients. The results were positively concordant in 137 patients, negatively concordant in 23 patients, and discordant in 38 patients (20 negative at C.I. vs. positive at PET/CT and 18 positives at ceCT/MRI vs. negative at PET/CT) (K Cohen = 0.426; p < 0.001). Sensitivities, specificities, and accuracies (95% confidence intervals) of PET/CT vs. C.I. for the detection of recurrent BC and UTUC were 94% (90% to 97%) vs. 86% (81% to 92%), 79% (67% to 92%) vs. 59% (44% to 74%), and 91% (87% to 95%) vs. 81% (75% to 86%), respectively.
Conclusions
FDG PET/CT has a high diagnostic accuracy for the identification of recurrent UC, particularly in patients with BC. Moreover, its accuracy outperforms C.I. for both BC and UTUC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Bladder cancer (BC) is the 7th most commonly diagnosed cancer in the male population worldwide, while it drops to 11th when both genders are considered. The worldwide age-standardized incidence rate (per 100.000 person/years) is 6.0 for men and 1.8 for women [23]. BC account for 90% to 95% of urothelial carcinomas (UC) while upper tract urothelial cancers (UTUC) are uncommon and account for the remaining 5% to 10% of UC [17, 23, 24]. Advanced UC has an aggressive biological behavior and a higher incidence of metastases resulting in a worse prognosis. Imaging studies are frequently performed for staging and re-evaluation of UC, in order to provide information for therapy and assess the prognosis.
Assessment of local tumor extension is usually performed with magnetic resonance imaging (MRI) or computed tomography (CT) scan [11, 14]. The assessment of other UC in the urinary system is performed with excretory-phase CT urography which has the highest diagnostic accuracy for UTUC [9]. However, conventional modalities have limitations, in particular for the assessment of lymph node involvement and distant metastasis, both in staging and re-staging settings.
Indeed, assessment of lymph node metastases is based solely on size and it is unreliable by the inability of both CT and MRI to identify metastases in normal-sized or minimally enlarged nodes [1]. A skeletal evaluation is not routinely indicated unless the patient has specific symptoms or lab abnormalities [1]. Positron emission tomography (PET)/CT imaging in UC has not been fully studied, in part because the urinary excretion of 18F-fluorodeoxyglucose (FDG) interferes with visualization of the primary BC and regional nodes. However, PET/CT provides anatomic and metabolic information for staging and re-staging and has been incorporated into the management of many urological [20] and non-urological malignancies [21]. FDG PET/CT in patients with UC may help to detect lesions that are indeterminate or undetectable by CT and/or MRI. Studies reporting the use of PET/CT in the UC in the staging and re-staging setting showed a per patient sensitivity and specificity ranging from 81% to 100% [5, 13] and 83% to 94% [3, 19], respectively. However, the level of evidence on these FDG PET/CT studies in UC is poor. Major limitations include 1-the retrospective nature of the studies, 2-small sample size [3, 8, 10]; 3-different histologic types [2, 5]; 4-few comparisons between the diagnostic accuracy of FDG PET/CT with conventional imaging [13]; 5-FDG PET/CT accuracy not independently assessed for BC and UTUC [5, 13]; 6-patients in staging and re-staging setting considered altogether [5, 13, 18]; and 7-accuracy rarely assessed for a per site-based analysis [5].
Therefore, the primary aim of this multicenter study was to determine the performance accuracy of FDG PET/CT after primary tumor treatment for both BC and UTUC in a per patient- and per site-based analysis. The secondary aim of the study was to compare the accuracy of FDG PET/CT with that of ceCT and MRI.
Materials and methods
Study approval and data collection
The study protocol was notified at IOV—IRCCS on April 2016 (Approval No. 005275). Major US and European urological centers experienced in urothelial cancers and FDG PET/CT were offered the participation to the study. Written informed consent for the execution of PET/CT and anonymous publication of disease-related information was signed by each patient. Available centers sent a list of anonymized cases in a dedicated Microsoft Excel file created for the purpose of the study. A computerized databank was generated for de-identified data transfer. After combining the datasets, reports were generated for each variable to identify data inconsistencies. Through regular communication with all sites, resolution of all identified anomalies was achieved before analysis. Finally, the database was frozen, and the final dataset was produced for the current analysis.
Patient population
From 2005 to 2015, FDG PET/CT scans of 287 patients with suspicious for recurrent UC, collected by San Raffaele Hospital in Milan (Italy), Mayo Clinic in Rochester (MN, USA), Veneto Institute of Oncology IOV – IRCCS in Padua (Italy), Sant’Orsola Malpighi Hospital in Bologna (Italy) and Hospital of Ferrara (Italy), were retrospectively reviewed. Median age was 70 years (range 32–94 years). Inclusion criteria for the study were (1) patients with a known history of BC and/or in the UTUC; (2) FDG PET/CT images after curative treatment of the primary tumor; (3) conventional imaging modalities (abdominal ceCT or MRI, or total body ceCT, and chest X-ray, called C.I.) performed no more than 3 months from PET/CT; (4) available standard of reference (e.g., histological data or imaging modalities) for the assessment of PET/CT findings. Exclusion criteria were advanced abdominal tumor or history of tumors within 5 years, and chemotherapy administration concomitant to imaging and non-urothelial cancer variants.
For each patient, at the time of PET/CT study and/or during follow-up the following variables were collected: demographic data (age, sex, body mass index-BMI), clinical data (history of BC, last clinical stage, history of renal cancer (RC), pTNM stage at RC, history of UTUC, UTUC location (renal pelvis, ureter, multifocal), UTUC treatment (nephroureterectomy, endourology, other conservative surgery), use and type of neoadjuvant treatments, and imaging data (site of positivity (local, lymph nodes, skeletal, lung, liver, and others); site and laterality of positive lymph nodes at PET/CT, ceCT scan, and/or MRI).
PET/CT equipment and image acquisition protocol
PET/CT images were acquired in all centers, by using a standard comparable protocol. All patients fasted for at least 6 h prior to imaging, and blood glucose levels were < 180 mg/dL at the time of tracer injection. To minimize FDG uptake in skeletal muscles, all patients were instructed to avoid talking, chewing, or any muscular activity before acquiring the PET/CT scan. PET/CT studies were acquired with integrated by PET/CT systems, according to different injected doses, PET/CT scanners, and image analysis method (Table 1). PET data of the whole-body tracer distribution were then acquired (3 min per bed) in 3-D mode starting 60 min after the i.v. administration of FDG. Attenuation correction was performed using CT images. CT and PET images were matched and fused into transaxial, coronal, and sagittal images. No contrast enhanced was used in PET/CT.
Two experienced nuclear physicians reviewed PET/CT scan, partially blinded and based on visual analysis to identify the area of recurrent disease. Inconsistent findings between the two readers were discussed and agreed upon consensus.
A positive PET scanner was defined in the presence of pathological FDG uptake outside the areas of physiological biodistribution, later confirmed by co-registered CT abnormalities. No semiquantitative analysis was used for the re-interpretation of the PET scan due to the variability in image acquisition and reconstruction parameters.
Conventional imaging interpretation
Patients were generally observed according to standard pathologic procedures at each institution, every 3–6 months for the first year after surgery, and annually thereafter. Follow-up consisted of a history, physical examination, routine blood work, and serum chemistry studies, C.I, as per urologist and medical oncologist preference. With C.I. we considered all findings provided by abdomen and pelvis ceCT or abdomen and pelvis MRI. Whole-body ceCT was performed in selected patients at higher risk of recurrence. Furthermore, a ceCT of the thorax was routinely performed with a suspicious chest X-ray. As not explicitly recommended in the European and American guidelines, each center adopted their own imaging follow-up, but similar for this study.
Two radiologists with an experience of at least 5 years reinterpreted the abdominal–pelvis ceCT and MRI procedures. Inconsistent findings between the two readers were discussed and agreed upon consensus.
Recurrent disease was defined in accordance with the size of the lesions. For example, nodal lesions were considered malignant only if larger than 10 mm. However, the presence of local, lung, liver, and skeletal metastases was defined based on the anatomical characteristics of the lesions (size, margins, density, contrast enhancement parameters, and others).
Standard of reference
The standard of reference was established by histopathology and further C.I. scans that was different from those employed for the comparison of diagnostic performance. These imaging modalities were made after 3–6 months from FDG PET/CT scan and were used as standard of reference only in patients without an available histopathological analysis. The diagnosis of metastatic disease was obtained by the combination of positive clinical findings and/or the resolution of the lesions after appropriate therapy and/or increase of number/size/FDG uptake of preexisting lesions, whereas no disease was defined by combination of negative clinical findings and/or negative findings of other studies.
Statistical analysis
Categorical variables were reported as frequency, while continuous variables were reported as mean standard deviation (SD) for variables with a normal distribution. The differences between categorical and continuous variables were assessed by using χ2 test and t student test, respectively. A patient-based and a K agreement analysis were used to compare the findings of all three imaging modalities. Agreement among image modalities was considered to be poor when k was less than 0.20, fair when k ranged from 0.21 to 0.40, moderate when k ranged from 0.41 to 0.60, good when k ranged from 0.61 to 0.80, and very good when k was greater than 0.80 [4].The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), accuracy, and number of correctly recognized cases of PET/CT were calculated in a patient- and site-based analysis, respectively, for overall population and separately for BC and UTUC. An additional analysis was performed only for those patients with a histopathological examination as gold standard (see the “Standard of reference” section). Significance for all tests was set at p < 0.05. Analysis were performed using SPSS version 20 (IBM, Armonk, NY, USA).
Results
Clinical characteristics
Patient characteristics are summarized in Table 2. Two-hundred thirteen patients underwent cystectomy (74.2%), 35 nephroureterectomy (12.2%), 31 both cystectomy + nephroureterectomy (10.8%), 5 both cystectomy + conservative treatment for UTUC (1.4%), and 3 (1%) other types of nephron-sparing treatments for UTUC.
For those patients with BC, pathological T2 was found in 40 (13.9%), while a non-organ confined disease (≥ pT3) was present in 97 (33.8%) cases.
For those patients with UTUC, pathological T2 was found in 11 (14.8%) patients, while a non-organ confined disease (≥ pT3) was present in 28 (37.8%) cases. Neoadjuvant and adjuvant treatments were performed based on the initial staging in 36 (12.5%) patients and 111 (38.7%), respectively. Among adjuvant treatment, 89 (31%) patients were treated with chemotherapy, 19 (6.6%) with radiotherapy, and 3 (1%) by the combination of radiotherapy and chemotherapy.
FDG PET/CT, ceCT, and MRI results
A positive PET/CT was found in 225 (78.4%) patients. Of these, 58 were positive at local site, 126 at lymph nodes, 58 at skeletal site, 53 at lung, 28 at liver, and 26 in other sites. ceCT was available in 176 patients, being positive in 131 (74.4%) subjects. Twenty-eight patients had a positive ceCT in the local site, 58 in the lymph nodes, 18 in the skeletal, 39 in the lung, 9 in the liver, and 19 in the other sites. Finally, C.I. results were available in 198 patients, resulting positive in 155 (78.3%) patients. Forty-two patients had a positive finding in the local site, 69 in the lymph nodes, 25 in the bone, 42 in the lung, 10 in the liver, and 20 in other sites.
The results of FDG PET/CT and ceCT was positively concordant in 116 patients, negatively concordant in 24 patients, and discordant in 36 patients (21 negative at ceCT vs. positive at PET/CT and 15 positive at ceCT and negative at PET/CT) (K Cohen = 0.438; p < 0.001). Moreover, the results of PET/CT and C.I. were positively concordant in 137 patients, negatively concordant in 23 patients, and discordant in 38 patients (20 negative at C.I. vs. positive at PET/CT and 18 positives at C.I. and negative at PET/CT) (K Cohen = 0.426; p < 0.001).
Patient-based analysis
As gold standard, final pathology, clinical evaluation, and C.I. modalities were available in 160 (55.7%), 40 (13.9%), and 87 (30.3%) patients, respectively. In Table 3 and Fig. 1 are reported the diagnostic performances of PET/CT, ceCT, and C.I, per patient-based analysis. As illustrated, PET/CT was more sensitive and specific than ceCT and C.I. in all patients and in those with BC. Similarly, a higher specificity than C.I. was reported in patients with UTUC.
Site-based analysis
Diagnostic accuracies of PET/CT, ceCT, and C.I. are reported in Table 4. As shown, PET/CT had a high specificity and PPV in all patients, while its sensitivity and accuracy was low-moderate, resulting in equal to 61% in the lymph nodes. By comparing the accuracies of C.I. and FDG PET/CT in 198 patients, FDG PET/CT showed a sensitivity of 60% vs. 42% of C.I. at lymph node level. Moreover, the specificity in the lung site was higher for FDG PET/CT than C.I. (95% vs. 77%) and finally, the accuracy for bone metastases was higher for PET/CT than C.I. (40% vs. 31%). Similar results were reported by the comparison between FDG PET/CT and ceCT for the same site of disease (Table 1s). For the lymph nodes, PET/CT was able to better identify the recurrencice in all sites as compared both ceCT and C.I. In particular, its contribution was reported for the lymph nodes in the inter-aorto-caval, para-caval, and peri-aortic region.
Discussion
An optimum clinical scenario for FDG PET/CT application is the instance of tumor re-staging or evaluation for suspected urothelial recurrence. Although PET/CT has a consolidated role in the re-staging after primary treatment of some urological cancers [7, 12], its application in UC is still understudied and unevaluated. Here in, we selected a population of patients affected by urothelial cancer who underwent 18F-FDG PET/CT in order to evaluate the presence of recurrent disease, for the suspicious of recurrence at C.I, or indeterminate C.I. findings or with a high risk disease (T3 or other unfavorable prognostic data).
In the present study involving 287 patients with UC, FDG PET/CT showed a good sensitivity (94%, CI 95%: 91% to 96%) and specificity (79%, CI 95%: 68% to 88%), for the detection of recurrence in both BC and UTUC, being also higher than ceCT and ceCT/MRI. Similarly, the accuracy of PET/CT, by a site-based analysis evaluation, showed a general higher performance of PET/CT in comparison to the other C.I. These results are in line with previous retrospective studies where an overall good performance of PET/CT has been shown in a patient-based analysis (Table 5). Alongi et al. [3] in a study with 41 recurrent BC patients found a sensitivity, specificity, PPV, NPV, and accuracy of 87%, 94%, 95%, 85%, and 90%, respectively. Ozturk et al. [12] in 51 recurrent UC found a sensitivity, specificity, PPV, NPV, and accuracy of 92%, 83%, 94%, 77%, and 90%, respectively. Similarly, Kitajima et al. [11] found in 83 patients with either BC or UTUC, a sensitivity, specificity, PPV, NPV, and accuracy of 97.4%, 93.3%, 92.5%, 97.7%, and 95.2%, respectively. To the best of our knowledge, no studies have evaluated the performance of PET/CT only for UTUC recurrence after primary treatment. The only terms of comparison are two studies assessing the role of 11C-choline PET/CT for the primary tumor staging. In these studies, a sensitivity and specificity for the lymph node invasion was found in 100% and 100% [22] and 83% and 100% [6], respectively.
However, the advantages provided by the present study in comparison to the previous ones are several. First, this is the largest multicenter study reported in the literature. Second, the study population is fairly homogeneous with all having undergone primary treatment and suspected UC recurrence. Third, accuracy of PET/CT was assessed separately for UTUC and BC. Although still UC, the sites of metastasis or specifically nodal involvement are different [15, 16]. Therefore, it is prudent to consider these tumors as two separate entities. Fourth, accuracy of PET/CT was compared with the conventional imaging, such as ceCT and MRI, which is the gold standard for the staging and re-staging of UC. The main limitation to use ceCT and MRI as a gold standard is the intrinsic uncertainty of the false negatives or false positives results. This could explain why agreement between PET/CT and conventional imaging was found to be moderate (K = 0.46), underling the need for further research in this field.
However, this research describes not only promising results, but also raises new questions that only further studies may answer.
New alternative PET tracers (i.e., 11C-choline or other future agents) and markers, as well as better software and machines, have the potential to improve PET/CT imaging, although they have been used in the staging setting and not in the re-staging one when a high percentage of tumors with unfavorable prognosis are present. In particular, the use of a co-registration CT urography with PET/CT data could allow a better staging of UC recurrence in either the residual urinary tract after surgery or in the lymph nodes. In fact, the type of urinary diversion whether continent or incontinent may alter the detection rate of retroperitoneal or pelvic lymph nodes. Indeed, the intensely diverted intraluminal urine activity can hinder the detection of an adjacent small local recurrence or metastatic lesions. Thus, a stratification according to the urinary diversion may improve the staging of retroperitoneal and pelvic lymph nodes.
At site-based analysis, FDG PET/CT showed a higher diagnostic accuracy than C.I, particularly for the lymph node detection. Moreover, PET/CT seems able to better identify the presence of distant lymph node involvement (e.g., inter-aortocaval, para-caval, and peri-aortic nodes).
Finally, an economic evaluation investigating the cost-effectiveness of FDG PET/CT scanning should be investigated in order to justify the routine use of this imaging technique in UC patients in comparison to C.I.
As a retrospective multicenter study, limitations are inherent. The final pathology was not available for all cases. The low sensitivity in a per site-based analysis was due to the inability to completely assess the NPV since the tissue was not all sampled. Moreover, no peculiar preparation and/or strategy concerning hydration (i.e., diuretic administration), and start of whole-body scan from the pelvis was used.
Finally, images were not centrally reviewed, although all the radiologists and nuclear medicine physicians have at least 5 years of experience in genitourinary imaging and FDG PET/CT.
Conclusion
By a per patient-based analysis, FDG PET/CT has a good accuracy in the detection of both BC and UTUC recurrence after primary treatment. In a per site-based analysis, FDG PET/CT has also a higher accuracy than C.I. in lymph node assessment. From a clinical standpoint, these findings have important implications in the follow-up after primary treatment and in therapeutic decision-making of urothelial recurrences; however, the role of FDG PET/CT in UC is still emerging and definitive recommendations cannot be made yet. It is indisputable that it would be of great importance to investigate the clinical value of FDG PET/CT prospectively.
References
Alfred Witjes J, Lebret T, Comperat EM, et al. (2016) Updated 2016 EAU guidelines on muscle-invasive and metastatic bladder cancer. Eur Urol 71(3):462–475
Aljabery F, Lindblom G, Skoog S, et al. (2015) PET/CT versus conventional CT for detection of lymph node metastases in patients with locally advanced bladder cancer. BMC Urol 15:87
Alongi P, Caobelli F, Gentile R, et al. (2017) Recurrent bladder carcinoma: clinical and prognostic role of 18 F-FDG PET/CT. Eur J Nucl Med Mol Imaging 44:224–233
Altamn D (1991) Practical statistics for medical research. Boca Raton: Chapman & Hall/CRC
Apolo AB, Riches J, Schoder H, et al. (2010) Clinical value of fluorine-18 2-fluoro-2-deoxy-d-glucose positron emission tomography/computed tomography in bladder cancer. J Clin Oncol 28:3973–3978
Asai S, Fukumoto T, Tanji N, et al. (2015) Fluorodeoxyglucose positron emission tomography/computed tomography for diagnosis of upper urinary tract urothelial carcinoma. Int J Clin Oncol 20:1042–1047
Bouchelouche K, Choyke PL (2015) PET/computed tomography in renal, bladder, and testicular cancer. PET Clin 10:361–374
Chaudhry MA, Wahl R, Kadhim LA, et al. (2013) Contrast enhanced computed tomography characterization of fluorodeoxygluocose-avid regional and non-regional lymph nodes in patients with suspicion of metastatic bladder cancer. J Clin Imaging Sci 3:66
Cowan NC (2012) CT urography for hematuria. Nat Rev Urol 9:218–226
Jadvar H, Quan V, Henderson RW, et al. (2008) [F-18]-Fluorodeoxyglucose PET and PET-CT in diagnostic imaging evaluation of locally recurrent and metastatic bladder transitional cell carcinoma. Int J Clin Oncol 13:42–47
Kim JK, Park SY, Ahn HJ, et al. (2004) Bladder cancer: analysis of multi-detector row helical CT enhancement pattern and accuracy in tumor detection and perivesical staging. Radiology 231:725–731
Kitajima K, Yamamoto S, Fukushima K, et al. (2016) Update on advances in molecular PET in urological oncology. Jpn J Radiol 34:470–485
Kitajima K, Yamamoto S, Fukushima K, et al. (2016) FDG-PET/CT as a post-treatment restaging tool in urothelial carcinoma: comparison with contrast-enhanced CT. Eur J Radiol 85:593–598
Mallampati GK, Siegelman ES (2004) MR imaging of the bladder. Magn Reson Imaging Clin N Am 12:545–555
Matin SF, Sfakianos JP, Espiritu PN, et al. (2015) Patterns of lymphatic metastases in upper tract urothelial carcinoma and proposed dissection templates. J Urol 194:1567–1574
Moschini M, Karnes RJ, Sharma V, et al. (2016) Patterns and prognostic significance of clinical recurrences after radical cystectomy for bladder cancer: a 20-year single center experience. Eur J Surg Oncol 42:735–743
Munoz JJ, Ellison LM (2000) Upper tract urothelial neoplasms: incidence and survival during the last 2 decades. J Urol 164:1523–1525
Ozturk H (2015) Detecting metastatic bladder cancer using (18)F-fluorodeoxyglucose positron-emission tomography/computed tomography. Cancer Res Treat 47:834–843
Ozturk H, Karapolat I (2015) Efficacy of 18F-fluorodeoxyglucose-positron emission tomography/computed tomography in restaging muscle-invasive bladder cancer following radical cystectomy. Exp Ther Med 9:717–724
Rioja J, Rodriguez-Fraile M, Lima-Favaretto R, et al. (2010) Role of positron emission tomography in urological oncology. BJU Int 106:1578–1593
Rohren EM, Turkington TG, Coleman RE (2004) Clinical applications of PET in oncology. Radiology 231:305–332
Sassa N, Kato K, Abe S, et al. (2014) Evaluation of 11C-choline PET/CT for primary diagnosis and staging of urothelial carcinoma of the upper urinary tract: a pilot study. Eur J Nucl Med Mol Imaging 41:2232–2241
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67:7–30
Soria F, Shariat SF, Lerner SP, et al. (2016) Epidemiology, diagnosis, preoperative evaluation and prognostic assessment of upper-tract urothelial carcinoma (UTUC). World J Urol 35(3):379–387
Tanaka H, Yoshida S, Komai Y, et al. (2016) Clinical value of 18F-fluorodeoxyglucose positron emission tomography/computed tomography in upper tract urothelial carcinoma: impact on detection of metastases and patient management. Urol Int 96(1):65–72
Acknowledgements
The authors are thankful to Dr. Marco Bartolomei (Department of Nuclear Medicine, Hospital of Ferrara, Ferrara, Italy), Dr. Francesco Massari (Department of Oncology, Sant’Orsola-Malpighi Hospital, Bologna, Italy), Prof. Eugenio Brunocilla (Department of Urology, Sant’Orsola-Malpighi Hospital, Bologna, Italy), and Prof. Filiberto Zattoni (Department of Urology, University of Padua, Padua, Italy) for their support in the execution of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zattoni, F., Incerti, E., Colicchia, M. et al. Comparison between the diagnostic accuracies of 18F-fluorodeoxyglucose positron emission tomography/computed tomography and conventional imaging in recurrent urothelial carcinomas: a retrospective, multicenter study. Abdom Radiol 43, 2391–2399 (2018). https://doi.org/10.1007/s00261-017-1443-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1443-6