Abstract
Objective
To determine if the attenuation of contrast material in the excluded stomach compared with the gastric pouch is helpful in diagnosing gastrogastric (GG) fistula.
Materials and methods
In a retrospective study, 13 CT scans in 12 patients (age 43.2 ± 9.2, 10 females) who had undergone Roux-en-Y gastric bypass and who had oral contrast in both the gastric pouch and excluded stomach were qualitatively and quantitatively evaluated for GG fistula by two radiologists, using upper GI series (UGI) as the gold standard. Quantitative analysis was performed by computing the relative attenuation (RA) ratio (HU in excluded stomach/HU in gastric pouch). Statistical analysis was performed to determine if the RA ratio values correlated with the UGI findings of GG fistula.
Results
46.2% (6/13) of UGI studies demonstrated a GG fistula. Statistical analysis demonstrated a significant difference in RA ratio (P < 0.05) between the fistula group (1.12 ± 0.29) and the reflux group (0.56 ± 0.19). A receiver operating characteristic analysis identified an RA ratio of 0.8 that maximized sensitivity (100%), at the expense of specificity (78.6%), for diagnosing GG fistula. In contrast, the initial qualitative evaluation for GG fistula yielded a lower sensitivity (45.8%) and a higher specificity (89.2%). After taking RA ratios into account, radiologists’ final conclusions achieved higher sensitivity (58.3%) and specificity (100%).
Conclusion
The relative attenuation ratio of oral contrast in the excluded stomach versus the gastric pouch can be a reliable tool in differentiating GG fistula from oral contrast reflux up the biliopancreatic limb on CT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Gastrogastric (GG) fistula is a well-recognized, albeit a relatively uncommon, complication of Roux-en-Y gastric bypass (RYGB) surgery [1,2,3,4,5]. The reported incidence of GG fistula is approximately 3% [1]. It is defined as a fistulous connection between the surgically created gastric pouch and excluded stomach. The fistulous connection between the gastric pouch and excluded stomach acts as a bidirectional roadway, allowing food to enter the gastric remnant thus resulting in poor weight loss or even weight gain, and permitting hydrochloric acid to enter the gastric pouch and cause stomach ulceration [2]. An upper gastrointestinal (UGI) fluoroscopic study is the modality of choice for diagnosing GG fistula [3, 5]. However, many cases of GG fistula are subclinical, as patients are asymptomatic and may not lose the sensation of early satiety [3]. Therefore, GG fistula may be an unsuspected finding at computed tomography (CT) imaging, and correctly making this diagnosis is important.
Computed tomography has become increasingly popular and is the imaging modality of choice in evaluating gastric bypass patients [6]. A GG fistula is definitively diagnosed on CT if the fistulous connection is directly visualized. However, this finding is rare [5]. A diagnostic dilemma occurs when the excluded stomach contains oral contrast material, which can either be the result of a GG fistula or retrograde flow from the jejunojejunostomy and biliopancreatic limb. In our experience, we have observed that in reflux of oral contrast through the biliopancreatic limb and into the excluded stomach, the oral contrast in the excluded stomach is more dilute than that in the gastric pouch. Sandrasegaran et al. [4] observed that the presence of dense contrast material in the excluded stomach implies a GG fistula. To our knowledge, no formal study has been published to validate these observations. Therefore, the purpose of this study is to determine if a GG fistula can be objectively diagnosed based on the attenuation of oral contrast material in the excluded stomach compared with the gastric pouch.
Materials and methods
This study was HIPAA compliant with a waiver of informed consent approved by the Human Investigation Committee at our institution.
Patient selection
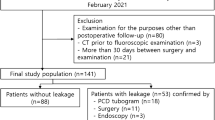
Our initial search criteria identified adult patients who were status post RYGB and have undergone an UGI examination during a 12-year period (January 1, 2004-December 31, 2015) at our institution. We used the Montage database radiology search engine (Montage Healthcare Solutions, Philadelphia, PA, USA) to obtain all UGI reports containing the words “gastric bypass,” and excluding the phrase “postoperative day one” in the text. Postoperative day one UGI studies were excluded due to the low frequency of immediate postoperative GG fistulas [7,8,9]. This yielded a total of 634 patients. In these patients, imaging studies were reviewed on our Picture Archiving and Communication System (Synapse-PACS Software Program System, Fujifilm, Tokyo, Japan) by a radiology resident (GG) to identify all patients who had a CT examination within 30 days of the UGI and that demonstrated oral contrast in both the gastric pouch and excluded stomach, with oral contrast distal to the jejunojejunostomy. CT scans that showed small bowel obstruction or external gastric devices, such as a percutaneous gastric tube, were excluded to avoid confounding factors (n = 3). This yielded 12 patients and 13 cases, as 1 patient had two sets of upper GI and CT studies. The patients’ medical records were reviewed to ensure that there was no surgical intervention between CT and UGI.
Imaging
All CT examinations were performed on MDCT scanners (GE Healthcare and Siemens) using automatic tube current modulation. The CT parameters varied but all cases were performed using 120 kVp with images reconstructed to 5-mm slice thickness in the axial plane. In some exams, coronal (n = 6, 5 mm slice thickness) and sagittal (n = 1, 5 mm slice thickness) images were also reconstructed.
CT exams were performed with IV and oral contrast (n = 11) or oral contrast only (n = 2). Four exams performed with IV contrast, a total of 100 mL of iohexol (Omnipaque 350, GE Healthcare) (n = 8) or 80 cc of iohexol (Omnipaque 300, GE Healthcare) (n = 3) was administered at 2–3 mL/sec using a scan delay of 70 s. Patients were asked to consume at least 500 cc of oral contrast as dilute (3%) Omnipaque 300 (n = 10) or 2% barium sulfate (Readi-Cat, EZ-EM) (n = 3) starting 1 h prior to the exam.
The UGI studies were performed using water-soluble contrast (n = 1), barium (n = 7), or both (n = 5) under fluoroscopy with spot and overhead films taken.
Imaging analysis
Two fellowship trained in abdominal radiology attendings (MM and PB) with 3.5 and 1.5 years of experience, respectively, separately evaluated the CT scans on a PACS system (Synapse, Fuji Medical Systems) and were asked to determine if a GG fistula was present, was not present, or was maybe present. A GG fistula was diagnosed if oral contrast was present in the excluded stomach but not in the biliopancreatic limb or if the fistulous tract was directly visualized. If a reader determined a GG fistula was not present, it was assumed that the contrast in the excluded stomach was secondary to reflux up the biliopancreatic limb. If the reader was unsure, the exam was recorded as maybe present. The radiologists were then instructed to compute a relative attenuation (RA) ratio of oral contrast density by first obtaining a Hounsfield unit (HU) measurement in the excluded stomach and gastric pouch, and then dividing the former by the latter. The radiologists were instructed to use an oval region of interest that covers more than 50% of the area that contains the brightest oral contrast on the axial slice (Figs. 1 and 2).
Example 1. Patient 1 52-year-old female status post RUGB presenting with abdominal pain and fever. A Axial CT image demonstrates contrast material in the gastric pouch (thin arrow) and excluded stomach (thick arrow). An RA ratio of 1.28 (320/251) indicates a gastrogastric fistula. B A spot fluoroscopic image from an UGI study confirms a GG fistula with contrast material passing from the gastric pouch (thin arrow) to the excluded stomach (thick arrow)
Example 2. Patient 2 28-year-old female status post gastric bypass presenting with abdominal pain. A Axial CT image demonstrates contrast material in the gastric pouch (thin arrow) and excluded stomach (thick arrow). An RA ratio of 0.64 (177/276) suggests the oral contrast within the excluded stomach is from biliopancreatic limb reflux, and not a GG fistula. B A spot fluoroscopic image from an UGI study shows a patent gastrojejunal anastomosis (thin arrow) without GG fistula
Since it has been observed that the presence of dense attenuation contrast material in the excluded stomach implies a GG fistula [4], the radiologists were asked to re-evaluate the CT images for GG fistula taking RA ratios into account.
Statistical analysis
Statistical analysis was performed with Statistical Package of Social Science (SPSS, IBM Corp., Chicago, IL) for Windows version 20. Chi square test or Fisher’s exact test was used to compare the qualitative variables. Comparisons of quantitative variables between the two groups were conducted using Mann–Whitney U test. Reliability of categorical variables was assessed using Cohen κ weighted for differences between the final diagnoses. Reliability of continuous variables, including RA ratio, was assessed using intra-class correlation coefficients and coefficients of variation estimated from random effects models. Inter-observer reliability for measured RA ratios was assessed using intra-class correlation coefficients. Reliabilities of less than 0.4 were characterized as poor, 0.4–0.75 as fair to good, and greater than 0.75 as excellent [10]. A P value less than 0.05 was considered statistically significant. A receiver operating characteristic curve was used to identify the best cutoff point with which to maximize the sensitivity for discriminating patients with gastrogastric fistula.
Results
Six of 13 (46.2%) cases were confirmed to have a fistula by UGI, whereas the other 7 (53.8%) cases had no fistula (Table 1). Patient characteristics (age 43.2 ± 9.2, 84.6% female) and time between CT and UGI (mean 14.2 days, range 3–30 days) were similar for each of the two groups. All initial gastric bypass operations were performed for weight loss.
A significant difference in RA ratio (P < 0.05) between the fistula group (1.12 ± 0.29) and the reflux group (0.56 ± 0.19) was demonstrated. Four out of the six (66.7%) GG fistula cases showed higher attenuation of oral contrast material in the excluded stomach than the gastric pouch. There was excellent inter-observer reliability (interclass correlation 0.97, P < 0.001). A receiver operating characteristic analysis identified an RA ratio of 0.8 with 100% sensitivity and 78.6% specificity for diagnosing GG fistula (Fig. 3). Using RA ratio of 0.8 as the cut-off, the positive predictive value, negative predictive value, and accuracy are 85.7%, 100%, and 92.3%, respectively. In comparison, the radiologists’ initial impressions yielded a much lower sensitivity (45.8%) and a higher specificity (89.2%). After taking RA ratios into account, radiologists’ conclusions were more definitive, with higher sensitivity (58.3%) and specificity (100%).
Discussion
The diagnosis of GG fistula may be challenging. Many patients may present with nonspecific symptoms, such as failure to lose weight after RYGB [2, 3]. Furthermore, multiple investigators have reported cases of asymptomatic patients with GG fistula who achieved excellent weight loss [11,12,13]. While UGI and upper endoscopy are considered to be the gold standard for diagnosis [11], many cases of GG fistula are subclinical on presentation and may not be referred to these diagnostic procedures. Therefore, it is important to make the correct diagnosis of an unsuspected GG fistula on CT, a popular modality and the modality of choice in evaluating gastric bypass patients in the emergent setting [6].
The diagnosis of GG fistula can be made at CT if the fistulous tract can be identified [5]. However, this is a rare finding. Oral contrast within the excluded stomach can also be a sign of a GG fistula. However, this can also be seen in cases of reflux of contrast up the biliopancreatic limb. Therefore, when contrast material is present in the excluded stomach and a GG fistulous tract is not identified, the radiologist is presented with a quandary. It becomes unclear if a GG fistula is present, or not. Sandrasegaran et al. [4] observed that the presence of dense contrast material in the excluded stomach implies a GG fistula. Our study confirms this observation and has determined that an RA ratio of 0.8 or greater (excluded stomach/gastric pouch) is highly sensitive for GG fistula (100%), outperforming our readers’ sensitivity from initial impression (45.8%).While it is not known why the HU attenuation of contrast within the excluded stomach may be greater than that in the gastric pouch in cases of GG fistula, we hypothesize that swallowed saliva may dilute the gastric pouch contents prior to the CT scan and preferentially enter the Roux limb rather than the smaller fistulous connection with the excluded stomach.
Our study has several limitations. It was performed at a single tertiary care institution as a retrospective review and may not be universally applicable to other hospital or outpatient settings. Our sample size was small given the rarity of the studied condition and our strict exclusion criteria, although a statistical significance was still reached. There may be a selection bias as all but one CT were performed for abdominal pain. Although an UGI is considered the study of choice for diagnosing GG fistula, it is possible that falsely negative UGI exams occurred. Furthermore, while we only selected CTs performed within a short time frame of UGI (mean 14.2 days, range 3–30 days), with no surgical intervention in between, it is conceivable that a fistula may have developed in the interim. It should also be noted that while measuring the attenuation of oral contrast in both the gastric pouch and excluded stomach and then computing the relative attenuation ratio, may not be practical in some busy radiology practices, it seems to be a useful tool when the correct diagnosis is in doubt. Also, two different types of oral contrast were used in this study and it is possible that the native attenuation of the oral contrast may contribute to the overall RA ratio.
The RA ratio of oral contrast in the excluded stomach to the gastric pouch can be a useful diagnostic tool in identifying GG fistula. Our study demonstrated that an RA ratio of 0.8 or greater (excluded stomach/gastric pouch) is highly sensitive for the diagnosis of GG fistula.
References
Capella JF, Capella RF (1999) Gastro-gastric fistulas and marginal ulcers in gastric bypass procedures for weight reduction. Obes Surg 9(1):22–27
D’Hondt M, Vansteenkiste F, Van Rooy F, Devriendt D (2006) Gastrogastric fistula after gastric bypass–is surgery always needed? Obes Surg 16(11):1548–1551
Merkle EM, Hallowell PT, Crouse C, Nakamoto DA, Stellato TA (2005) Roux-en-Y gastric bypass for clinically severe obesity: normal appearance and spectrum of complications at imaging 1. Radiology. 234(3):674–683
Sandrasegaran K, Rajesh A, Lall C, et al. (2005) Gastrointestinal complications of bariatric Roux-en-Y gastric bypass surgery. Eur Radiol 15(2):254–262
Varghese JC, Roy-Choudhury SH (2009) Radiological imaging of the GI tract after bariatric surgery. Gastrointest Endosc 70(6):1176–1181
Scheirey CD, Scholz FJ, Shah PC, et al. (2006) Radiology of the laparoscopic Roux-en-Y gastric bypass procedure: conceptualization and precise interpretation of results 1. Radiographics. 26(5):1355–1371
Blachar A, Federle MP, Pealer KM, Ikramuddin S, Schauer PR (2002) Gastrointestinal complications of laparoscopic Roux-en-Y gastric bypass surgery: clinical and imaging findings 1. Radiology. 223(3):625–632
Dresel A, Kuhn JA, McCarty TM (2004) Laparoscopic Roux-en-Y gastric bypass in morbidly obese and super morbidly obese patients. Am J Surg 187(2):230–232
Gould JC, Garren MJ, Starling JR (2004) Lessons learned from the first 100 cases in a new minimally invasive bariatric surgery program. Obes Surg 14(5):618–625
Fleiss JL (1981) Statistical methods for rates and proportions. New York: Wiley, p 218
Stanczyk M, Deveney CW, Traxler SA, McConnell DB, Jobe BA (2006) O’rourke RW. Gastro-gastric fistula in the era of divided Roux-en-Y gastric bypass: strategies for prevention, diagnosis, and management. Obes Surg 16(3):359–364
Carrodeguas L, Szomstein S, Soto F, et al. (2005) Management of gastrogastric fistulas after divided Roux-en-Y gastric bypass surgery for morbid obesity: analysis of 1292 consecutive patients and review of literature. Surg Obes Relat Dis 1(5):467–474
Gustavsson S, Sundbom M (2003) Excellent weight result after Roux-en-Y gastric bypass in spite of gastro-gastric fistula. Obes Surg 13(3):457–459
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Guangzu Gao, M.D., Nariman Nezami, M.D., Mahan Mathur, M.D., Patricia Balcacer, M.D., Gary Israel, M.D., and Michael Spektor, M.D. declares that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Gao, G., Nezami, N., Mathur, M. et al. Diagnosis of gastrogastric fistula on computed tomography: a quantitative approach. Abdom Radiol 43, 1329–1333 (2018). https://doi.org/10.1007/s00261-017-1304-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1304-3