Abstract
Objectives
This study was performed to evaluate the efficacy of a novel computed tomography (CT) liver detection algorithm (LDA), which allows for targeted increase of radiation dose to the upper abdomen, on image quality of the liver.
Methods
We retrospectively evaluated the LDA by comparing 40 consecutive patients who had portal venous CT abdomen performed without use of the algorithm, to 40 patients in whom the algorithm was used. Image quality was assessed objectively by comparing the standard deviation (SD) of attenuation values in Hounsfield units (HU) of the abdominal organs. Qualitative analysis was performed by two blinded radiologists who independently graded the image quality of abdominal organs
Results
There was significant noise reduction in the liver (P < 0.001) and spleen (P < 0.001) in the LDA group compared to the conventional group. There was also a significant improvement in image quality of the liver (P < 0.001), kidney (P < 0.001), spleen (P < 0.001), pancreas (P < 0.001), and psoas (P = 0.005) in the LDA group compared to the conventional group. Overall dose between the two groups was similar.
Conclusions
This liver detection algorithm improves the subjective image quality of upper abdominal organs, in particular the liver, without increasing overall radiation dose.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Advances in state-of the-art computed tomography (CT) technology has generated great interest in its potential to improve image quality to aid diagnosis and simultaneously reduce the radiation dose to patients in accordance with the ALARA principle (as low as reasonable achievable). A major concern when reducing radiation dose by adjusting scan parameters is an increase in the image noise which can affect the diagnostic quality of images [1].
Maintaining adequate diagnostic confidence in low subject contrast organs, such as the liver, can be challenging when aiming to minimize patient dose. Noise reduction is critical in abdominal CT examinations as noise may obscure subtle lesions in such low contrast organs [1, 2]. Focal liver lesions are more readily depicted if there is a larger attenuation difference between the lesion and the surrounding normal liver parenchyma [3]. Attenuation differences of 5–40 hounsfield units (HU) typically allow confident detection in the normal liver [4]. As image noise increases detection of subtle lesions becomes more challenging [5]. The risk of missing hypovascular liver tumors in a noisy liver image substantially increases as the size of the patient increases [6].
Techniques such as noise-reducing image reconstruction algorithms, advanced dose modulation and post reconstruction noise reduction filters have been used in order to preserve the qualitative appearance of the scanned anatomy without a perceptible loss of anatomic structure delineation. However, these techniques are not without compromise [7, 8]. Liver lesions have been shown to be less conspicuous when post processing noise reduction filters are used when compared with base line low-dose CT [1, 2, 4, 9].
In May 2012 a novel liver detection algorithm (LDA) was installed on the study centre’s CT unit. The LDA allows for targeted increase of radiation dose to the liver and upper abdominal region to reduce the image noise whilst the dose to the pelvis is reduced. We hypothesize that the use of the LDA will allow for improved study interpretation of upper abdominal organs whilst having a minimal effect on interpretation of pelvic structures. The aim of this retrospective study was to evaluate the efficacy of this liver detection algorithm on the image quality of abdominal structures.
Methods and materials
Patients
Forty consecutive adult patients of all ages and genders who presented for a conventional portal venous phase iodinated contrast-enhanced abdominal CT during the month of March 2012, before the use of CT liver detection algorithm (LDA), and a further 40 consecutive adult patients of all ages and genders who presented for a portal venous phase iodinated contrast-enhanced abdominal CT, during the month of July 2012, after the installation of the CT LDA into the CT scanner were included in the study.
The exclusion criteria included the patients who did not have any iodinated contrast for their CT, whose CT images were degraded due to breathing and motion artefact and who were less than 18 years of age.
CT scanning and liver detection algorithm
These CT studies were undertaken using a 128-MDCT scanner with the LDA installed (Ingenuity, Philips Healthcare, Cleveland, USA). Both groups of patients utilized identical baseline scanning parameters with tube voltage of 100 kV, default mAs setting of 168 with dose modulation, together with a collimation of 64 × 0.625 mm. All CT images were reconstructed using the same statistical iterative reconstruction presets of level 4 iDose4 (Philips Healthcare, Cleveland, USA).
After the CT scanogram (scout) was performed, the LDA automatically placed a location line at the superior most aspect of the liver as detected from the initial scout images. A second location line was automatically placed at the default length 15cms inferior to this point (Fig. 1). The CT imaging technologist could then vary the position of each location line on the scout image to accurately reflect the liver extent, which was normally readily visualized on the scout. The defined segment of upper abdomen, within these two location lines, contained the liver and would receive a higher dose prescription while the abdomen and pelvis below the second location line received a lower dose. As a result, the overall dose of LDA CT would remain similar to that of conventional CT. The dose modulation varied between the LDA and control groups, even though all other default parameters were identical. The LDA was set up such that the radiation dose profile was shifted up by 24% for the defined upper abdomen while the dose was shifted lower for the remaining abdomen and pelvis below the liver. The outcome was that overall dose in both groups would be similar but the radiation dose distribution profiles in the z-axis direction were different.
Analysis
Objective assessment
The CT studies were blindly assessed by an experienced CT medical imaging technologist, who measured attenuation values in Hounsfield units and the corresponding standard deviation (SD) values by placing a region of interest (ROI) on the liver, spleen, kidneys, psoas, and bladder. The right and left lobes of the liver were assessed separately. The ROI was circular in shape and similar in size for the particular organ for all patients. Visualized vessels were avoided within the ROI. The SD of an attenuation value indicated the severity of image noise and could serve as part of the objective assessment of the image quality.
Subjective assessment
All these CT studies were de-identified, randomly and blindly reviewed by two CT radiologists, who had 19 and 10 years of CT abdominal experience. The image quality (IQ) of abdominal organs was assessed using a 5 point scale (5: excellent, 4: very good, 3: good, 2: poor, and 1: non diagnostic). Organs assessed included the liver, spleen, pancreas, kidneys, psoas muscle, and bladder.
The CTDI volume (CTDIvol) and dose-length product (DLP) of each CT study were recorded.
Statistical analysis
Data analysis was performed using the Stata software version 11 (StataCorp, Texas, USA). Objective measures of image quality were compared between groups (conventional vs LDA) using the Student’s t test with results reported as means (95% confidence intervals) as the data were found to be normally distributed. Subjective assessments were compared using the Mann–Whitney U test with results reported as medians (inter-quartile ranges) as the data were found to be non parametric. Agreement between radiologists was assessed using the Kappa statistic. A kappa value of 0.6–0.8 was considered as good agreement, 0.4–0.6 as moderate, 0.2–0.4 as fair, and <0.2 as poor agreement. A two-sided P value of less than 0.05 was considered as statistically significant.
Low risk ethics approval was obtained from the local hospital Human ethics and research committee as the study was conducted retrospectively.
Results
Eighty patients who presented for a portal venous phase CT abdomen were selected for review. Forty patients (16 men, 24 women) with a mean age of 51.8 years were scanned in the conventional group and 40 patients (18 men, 22 women) with a mean age of 56.8 years were scanned in the LDA group. There was no exclusion. Two patients in the conventional group were also included in the LDA group.
Overall dose
The conventional group had a mean CTDIvol of 7.86 and a DLP of 426. The LDA group was similar with a mean CTDIvol of 7.7 and a DLP of 402.
Image quality (noise)
The SD of the attenuation value in HU indicates image noise, which can be regarded as an objective measure.
The average noise values in the two groups are shown in Fig. 2. There was a significant noise reduction in the liver (P < 0.001) and spleen (P < 0.001) in the LDA group compared to the conventional group. However, there was no significant difference in the psoas and bladder between the two groups.
Image quality (subjective)
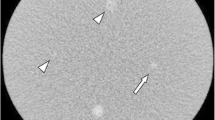
The median (inter-quartile range) grading of image quality for each of the assessed organs is presented in Table 1. There was a significant improvement in grading of the liver (P < 0.001), kidney (P < 0.001), spleen (P < 0.001), pancreas (P < 0.001), and psoas (P = 0.005) in the LDA group compared to the conventional group (Figs. 3,4, 5, and 6). However, the median grading was the same for the bladder in the two groups.
Contrast-enhanced portal venous phase CT of abdomen of a 70-year-old female who was also included in both conventional and LDA group displayed sharper interfaces between the liver edge and the intra-abdominal fat, and between the liver and gallbladder in LDA scan, as well as better vessel clarity in liver (B) as compared to conventional CT (A), even allowing for minor variation in the contrast phase
Conventional portal venous phase CT abdomen with no LDA of a 72-year-old female (A) demonstrated an abscess in segment 3 of her liver (black arrow). The same patient was subsequently scanned in the LDA group. On the follow-up CT (B), the margin of the abscess was more clear due to reduced image noise, although the abscess mildly increased in size between the 2 scans
Portal venous phase CT of pelvis in a 69-year-old female with no LDA (A) and LDA (B) showed no image degradation of the pelvic structures and iliacus-psoas muscles. There was a small amount of free fluid in the adnexal region which appeared more dense on the initial non-LDA image, likely related to some blood or protein content in the fluid
Inter-observer agreement
Results from Cohen’s Kappa test indicated that there was substantial agreement among reviewers for IQ of the liver with the LDA (Kappa value = 0.63). In comparison there was moderate agreement for IQ of the liver in the conventional group (Kappa value = 0.57). Results for the spleen demonstrate almost perfect agreement (Kappa value = 0.82) in the conventional group and only fair agreement (Kappa value = 0.39) in the LDA group.
Discussion
The liver has low intrinsic soft tissue subject contrast, and therefore, hypovascular lesions may be difficult to detect where there is a lot of image noise. Hepatic metastases are commonly hypovascular [3]. The relatively low contrast between these metastases and adjacent liver tissue, reduces detection, particularly if the lesions are small [9]. Given the high prevalence of liver disease in patients referred for abdominal CT examinations, it is important that scanning techniques are optimized for detection of liver pathology on routine CT abdomen [3].
Current CT technology utilizes a variety of automatic tube current modulation techniques. One of these is z-axis modulation. Z-axis modulation attempts to make all images have similar noise irrespective of patient size and anatomy along the z-direction [10]. As a result, the mAs profile along the z-axis is calculated so that the same noise level is maintained in all of the slices along the z-axis. The liver detection algorithm is a novel technique that goes beyond the use of body eccentricity and attenuation characteristics to optimize image noise. This advanced technique allows the identification of the upper abdominal portion that contains liver, on the scout image, and subsequently, targets more radiation dose to this defined region and less dose to the lower abdomen and pelvis. This enables better image quality of the important low subject contrast organs, such as the liver and spleen, without increasing radiation exposure to other regions or organs. Sensitivity for detection of liver lesions improves in proportion to a decrease in image noise [5] therefore the LDA should enable better detection of subtle liver lesions.
To maintain a similar overall radiation dose for the entire abdomen and pelvis, the LDA involves lowering the pelvic dose. The reduced dose to the pelvis is unlikely to be of diagnostic consequence as it is well documented that ultrasound is the preferred technique for evaluation of pelvic structures that includes the ovaries, uterus, and prostate. Ultrasound is the first line study of choice for evaluating adnexal masses, acute pelvic pain in the reproductive age group and lower urinary tract symptoms [11–13]. Contrast-enhanced CT is not routinely recommended for evaluating pelvic structures as it has poor contrast resolution and involves ionizing radiation [14]. In women with pelvic pain, CT is generally used only in emergency settings when ultrasound is inconclusive [11]. CT does, however, play an important role in diagnosing inflammatory conditions within the pelvis such as appendicitis and diverticulitis. It has been previously shown that low-dose CT techniques, in which dose reductions of 75–90% have been used, demonstrate similar sensitivity and specificity for depicting findings of acute diverticulitis because of the good interface between edema/stranding and adjacent peritoneal fat. [15]. The dose reduction to the pelvis associated with the LDA is therefore unlikely to significantly impact diagnosis of common inflammatory conditions. Masses, including collections and hematomas, as well as lymphadenopathy, are usually easily depicted on CT even if there is an increase in image noise.
Our study results confirmed a significant reduction in image noise based on the SD and significant improvement of image quality based on observational evaluation by two experienced radiologists of both the liver and spleen, which are included in the target field of the LDA. Therefore, based on previous studies demonstrating an inverse relationship between image noise and lesion detection [1, 2, 5] the LDA should enable better parenchymal evaluation and lesion detection. Other structures, such as the kidneys, psoas, and bladder, do not show any significant deterioration of image noise and observed image quality in our study. Subjective assessment of imaging quality of the liver, spleen, kidneys, and pancreas all demonstrated significant improvement. Interestingly image quality of the psoas was also graded higher for the LDA group. The psoas muscle extends from the upper portion of the abdomen into the pelvic region. The perceived better image quality of the upper half of psoas due to LDA likely resulted in the readers’ impression of overall improvement. Grading of the bladder was similar for both the LDA and conventional group despite the reduced dose to the pelvis in the LDA group, likely because of excellent density difference between urine and bladder wall which did not show any apparent degradation even at the lower pelvic radiation dose.
There was an excellent inter-observer agreement regarding image quality of the liver in the LDA group. By comparison, agreement was only moderate in the conventional group, reflecting that image perception of an organ might vary when there is increased image noise. There was, however, poor agreement for image quality of the spleen in the LDA group. One possible explanation for this is that the spleen commonly demonstrates a variable pattern of contrast enhancement depending on the volume of contrast that may have reached the spleen when the CT data were acquired. Similar to image noise, the perception of image quality in a heterogeneously enhancing organ may have varied.
Our study also showed that there was no radiation dose penalty with the use of the liver detection algorithm, as the CTDIvol and DLP were similar in both groups.
The major limitation of our study was the small number of subjects recruited. Further, the pre and post liver detection algorithm studies would have been ideally performed on the exact same patient group to eliminate biophysical difference in order to produce better comparable results. However, this was not practically possible due to ethical considerations. There was no record of patients’ weight and height during the time of scanning to allow us to assess any difference of body-mass index between the two groups. The inclusion of 40 patients in each arm of the study would possibly limit the biophysical differences to some extent. A future prospective study with a larger number of patients randomized between conventional and LDA CT scans of abdomen, with the inclusion of liver lesions for evaluation and consideration of body-mass index of the patients would be able to confirm the benefits of utilizing the LDA.
Conclusion
To our knowledge, this is the first study in the literature that assesses the efficacy of a targeted liver detection CT algorithm in reduction of image noise whilst maintaining a similar radiation dose across the entire abdomen and pelvis. This technique offers improved evaluation of liver parenchyma, and therefore, detection of liver lesions without compromising overall dose and may become an important CT scanning technique in the future.
Abbreviations
- CT:
-
Computed tomography
- DLP:
-
Dose length product
- HU:
-
Hounsfield units
- LDA:
-
Liver detection algorithm
- ROI:
-
Region of interest
- SD:
-
Standard deviation
References
Kalra MK, Maher MM, Blake MA, et al. (2004) Detection and characterization of lesions on low—radiation dose abdominal CT images postprocessed with noise reduction filters. Radiology 232(3):791–797
Funama Y, Awai K, Miyazaki O, et al. (2006) Improvement of low contrast detectability in low dose hepatic multidetector computed tomography using a novel adaptive filter: evaluation with a computer simulated liver including tumors. Invest Radiol 41:1–7
Baron RL (1994) Understanding and optimizing use of contrast material for CT of the liver. AJR Am J Roentgenol 163(2):323–331
Awai K, Takada K, Onishi H, Hori S (2002) Aortic and hepatic enhancement and tumor to liver contrast: analysis of the effect of different concentrations of contrast material at multi-detector row helical CT. Radiology 224:757–763
Kalpana MK, Chung JH, Wang J, et al. (2011) Image noise and liver lesion detection with MDCT: a phantom study. AJR Am J Roentgenol 197(2):437–441
Schindera ST, Torrente JC, Ruder TD, et al. (2011) Decreased detection of hypovascular liver tumours with MCDT in obese patients: a phantom study. AJR Am J Roentgenol 196(6):772–776
Baker ME, Dong F, Primak A, et al. (2012) Contrast-to-noise ratio and low-contrast object resolution on full- and low-dose MDCT: SAFIRE versus filtered back projection in a low-contrast object phantom and in the liver. AJR Am J Roentgenol 199(1):8–18
Mieville FA, Gudinchet F, Brunelle F, et al. (2013) Iterative reconstruction methods in two different MDCT scanners: Physical metrics and 4-alternative forced-choice detectability experiments—a phantom approach. Phys Med. 2012 Jan 2.
Robinson PJ (2000) Imaging liver metastases: current limitations and future prospects. Br J Radiol 73(867):234–241
Kalra MK, Maher MM, Toth TL, et al. (2004) Techniques and applications of automatic tube current modulation for CT. Radiology 233(3):649–657
Friedman B, Leyendecker JR, Blaufox MD, et al. (2014) Expert Panel on urologic imaging. ACR Appropriateness criteria lower urinary tract symptoms: suspicion of benign prostatic hyperplasia. American College of Radiology [Online publication]. Available from: http://www.guideline.gov/content.aspx?id=48292. Accessed on 22 Dec 2014
Andreotti RF, Lee SI, DeJesus Allison SO, et al. (2011) ACR Appropriateness criteria: acute pelvic pain in the reproductive age group. American College of Radiology [Online publication] Accessed 2014 October 22. Available from http://www.guideline.gov/content.aspx?id=32643. Accessed on Dec 2014
Harris RD, Javitt MC, Glanc P, et al. Expert Panel Women’s Imaging. (2012) ACR Appropriateness Criteria clinically suspected adnexal mass. American College of Radiology [Online publication]. Available from http://www.guideline.gov/content.aspx?id=48292. Accessed on 22 Dec 2014
Hodler RA Kubik-Huch, von Schuitness GK, Zollikofer CL (2014) Diseases of the Abdomen and Pelvis: diagnostic imaging and interventional techniques. Milan: Springer
McNamara MM, Lalani T, Camacho MA, et al. Expert Panel on Gastrointestinal Imaging. ACR Appropriateness Criteria left lower quadrant pain- suspected diverticulitis. American College of Radiology [Online publication]. Accessed Nov 2015
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Devapalasundaram, A., Lau, K.K., Paul, E. et al. Liver detection algorithm: its efficacy for CT noise reduction in the liver. Abdom Radiol 41, 493–499 (2016). https://doi.org/10.1007/s00261-015-0617-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-015-0617-3