Abstract
Purpose
Mesenteric ischemia and ischemic colitis are uncommon but potentially life-threatening causes of acute abdominal pain. Portal venous phase computed tomography (CT) is routinely ordered in the emergency room setting for abdominal pain, but subsequent MR angiography may be requested for additional evaluation of the mesenteric vasculature. We compare the concordance of CT and magnetic resonance angiography (MRA) for acute bowel ischemia.
Materials and Methods
Thirty-two patients who underwent contrast-enhanced MRA for bowel ischemia after having undergone CT evaluation within the preceding 2 weeks were identified. A retrospective review of imaging, treatment history, surgical, and pathology reports was conducted. Two radiologists each reviewed the imaging studies in a blinded fashion.
Results
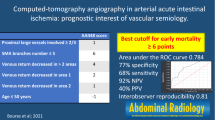
Ten cases of bowel ischemia were confirmed by endoscopy and/or surgical pathology. CT correctly identified bowel findings in all cases. Intraobserver agreement between CT and MRA for all vessels was 0.68 and 0.63, highest for the superior mesenteric artery. Interobserver agreement was 0.74 for MRA and 0.78 for CT. Vascular findings were only directly mentioned in 10 of 32 CT reports (and 7 of 10 cases with confirmed bowel ischemia). MRA only detected two additional or alternative diagnoses.
Conclusion
Portal venous phase CT and MRA demonstrate a high degree of concordance for vascular evaluation. Reviewed CT examinations were sufficient to assess the patency of the mesenteric vasculature, but vascular findings were not reported in most cases. A direct description within the report may have obviated the request for further MR imaging. MRA adds little value after portal venous CT in assessing bowel ischemia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Acute bowel ischemia (ABI) can be divided into two distinct entities: acute mesenteric ischemia (AMI) and ischemic colitis (IC). AMI is an uncommon but potentially devastating disease in patients presenting to the emergency department with abdominal pain. In an epidemiologic study of Malmö, Sweden, an estimate of incidence rate was given as 12.9 per 100,000 years [1], or 1 in 1000 acute hospital admissions [2] with estimated mortality rates of 60–80% [3]. AMI entails vascular compromise of the small bowel and encompasses a variety of etiologies, including mesenteric arterial embolic or thrombotic occlusion, mesenteric venous thrombosis, and nonocclusive mesenteric ischemia [4]. Acute arterial thromboembolism accounts for nearly two-third of cases [5], compared with smaller proportions for venous thrombosis (10%) and nonocclusive ischemia (25%) [6]. Patients with AMI present with a variety of often nonspecific complaints, including sudden or gradual onset of abdominal pain, nausea and vomiting, diarrhea, or bloody stools [7]. Pain out of proportion to physical exam findings is a classic but inconsistent finding.
IC, on the other hand, is a more common disease, accounting for greater than 50% of cases of intestinal ischemia [8]. Elderly patients are more commonly affected [9] with a better prognosis than AMI (estimated mortality rate of about 20%) [10]. The majorities of these cases are nonocclusive in nature and result from hypoperfusion or are medication induced, although vascular occlusion can more rarely be identified [9, 10]. The source of ischemia is frequently undiscovered, even after computed tomography (CT) or colonoscopy [10]. Most cases of IC are mild and self-limited in course or responsive to supportive therapy [11], although up to 20% may progress to transmural necrosis and require surgical resection [9]. Patients with IC, like AMI, often presents with nonspecific symptoms such as crampy abdominal pain, tenesmus, and hematochezia [8].
As a result, the diagnosis of ABI relies on a high index of clinical suspicion and appropriate imaging evaluation. Conventional angiography has long been considered the reference gold standard for diagnostic imaging while simultaneously offering therapeutic options [12], but its invasive nature, radiation exposure, length of examination and limited availability are considerable limitations. Noninvasive angiographic techniques utilizing multidetector-row computed tomographic angiography (CTA) [2, 12, 13], and more recently magnetic resonance angiography (MRA) [14, 15], have largely supplanted conventional angiography as initial tools in the evaluation of bowel ischemia, offering rapid and noninvasive evaluation of the emergency department patient. The 2013 ACR Appropriateness Criteria rate CTA at 9 and MRA at 7 in the evaluation of AMI [16], both in the “usually appropriate” range. MRA is rated lower than CTA due to the length of the examination and less availability compared with CTA. CTA demonstrates a sensitivity of 96% and specificity of 94% in detection of ABI using bowel and vascular findings [16].
Although CTA is acknowledged as the diagnostic imaging test of choice for AMI and will accurately identify cases of IC, many patients with unsuspected ABI present with nonspecific complaints for emergency care and are evaluated with routine single-phase portal venous computed tomography of the abdomen and pelvis (CT) as the first-line diagnostic imaging test. When ABI subsequently arises as a clinical suspicion, these patients may then later be evaluated with MRA. Studies have previously investigated the relative accuracy of CTA and MRA compared with the gold standard of conventional angiography [15], concluding that CTA provides better image quality and diagnostic accuracy than MRA, but to our knowledge, there have been no studies comparing single-phase portal venous CT with MRA in the evaluation of ABI. Our hypothesis is that vessel assessment with CT and MRA are highly concordant and that subsequent MRA adds time and expense but little clinical value in the evaluation of these patients. In this study, we investigate the rate of concordance between portal venous CT and MRA for evaluation of the mesenteric vasculature and detection of ABI, and MRA detection of additional or alternative diagnoses after initial CT.
Materials and methods
Patient selection
Following institutional review board approval, this retrospective study was conducted in compliance with Health Insurance Portability and Accountability Act (HIPAA) regulations. The radiology information system search tool was queried with the following search phrases, identifying patient examinations in which all of the words appeared in the report text: “magnetic resonance abdomen ischemia CT,” “magnetic resonance angiography abdomen ischemia CT,” and “magnetic resonance angiography abdomen ischemic CT.” The search included CT and MR examinations performed between January 1, 2006 and March 31, 2014 at our institution. Additionally, the medical record was searched to identify “ischemia” or “ischemic” within pathology, operative, and endoscopy reports of patients who underwent MRA and CT. The electronic medical record was then searched for patient demographic information, treatment history, laboratory data, surgical and endoscopy reports, and pathology reports. Patients were included in the study if they underwent an MRA examination within 2 weeks of the initial, intravenous contrast-enhanced CT examination.
Imaging parameters
All CT images were acquired on multidetector-row scanners, using a variety of scanners over the 8-year span, including the Volume Zoom (4 row), Sensation 10 (10 row), Sensation 16 (16 row), Sensation Open (20 row with flying focal spot), Definition AS+ (64 row with flying focal spot), and Definition Flash (dual source, 64-row with flying focal spot) CT scanners (Siemens Medical, Erlangen, Germany). CT images were reconstructed with 3-mm slice thickness and 2-mm reconstruction intervals. Studies were performed using 95–125 mL intravenous contrast (350 mg/mL iodine concentration) injected at 2–3 mL/s with a fixed delay of 70 s in a single-phase acquisition. In the few cases with multiphase CT imaging, the portal venous phase images were used exclusively for review. Oral contrast material is not routinely administered at our institution and was neither an inclusion nor exclusion criteria for the study.
MR images were acquired on 1.5 T scanners including the Espree, Sonata, Symphony, and Aera MR scanners (Siemens Medical, Erlangen, Germany). A specific mesenteric ischemia protocol was used, which has evolved over the years but currently consists of 6-mm transverse and coronal T2-weighted fast spin echo (HASTE), 6-mm axial and coronal fat-suppressed steady-state free precession (True FISP), 6-mm transverse 2D T1-weighted fat-suppressed gradient-recalled echo, and 2-mm coronal 3D T1-weighted fat-suppressed gradient-recalled echo images. A test bolus of intravenous gadolinium contrast was used to determine optimal timing for imaging of the abdominal aorta and mesenteric vessels, and post-contrast images were then obtained, consisting of 2-mm 3D coronal and sagittal T1-weighted fat-suppressed gradient-recalled echo and 6-mm 2D T1-weighted fat-suppressed gradient-recalled echo imaging. Maximum-intensity-projection and subtraction images were created from the source data. Intravenous gadolinium contrast agents used include gadoversetamide (Optimark, Mallinckrodt), gadobenate dimeglumine (MultiHance, Bracco), and most recently gadofosveset trisodium (Ablavar, Lantheus).
Image and clinical review
Two abdominal radiologists with expertise in body CT, emergency radiology, and vascular imaging independently reviewed the cases. The radiologists initially reviewed the MRA examinations for vascular findings and graded stenosis for the celiac artery (CA), superior mesenteric artery (SMA), and inferior mesenteric artery (IMA) according to the following scale: 0 = no stenosis, 1 = mild stenosis (<50% luminal diameter), 2 = moderate stenosis (50–70% luminal diameter), 3 = severe stenosis (>70% luminal diameter), and 4 = complete occlusion. Cases in which of the origin of the vessel could not be seen were categorized as complete occlusion. Bowel findings of ischemia, including bowel wall thickening, fat stranding, pneumatosis intestinalis, ascites, and free intraperitoneal or retroperitoneal air, were also recorded, along with alternative diagnoses for abdominal pain. After a 1-week washout period, CT examinations were then reviewed for the same findings. The reviewers were blinded to the clinical findings and patient outcomes during imaging review. The reference standard for diagnosis of mesenteric ischemia in this study was confirmation either through direct visualization at endoscopy or surgery, and/or pathologic analysis obtained from those procedures. The reports issued for the studies at the time of initial interpretation were also reviewed. Clinical follow-up of patients without a surgical or pathologic diagnosis was obtained from the medical record.
Data analysis
Data from the image review were tabulated in Microsoft Excel 2013 (Microsoft, Redmond, WA). Inter-test agreement between CT and MRA for all vessels in aggregate and for each vessel was analyzed for each reviewer using the quadratic-weighted Fleiss’ kappa statistic (κ). This statistic represents the rate of agreement between the two tests: 0 represents agreement at the level of chance, 0.01–0.20 is poor, 0.21–0.40 is fair, 0.41–0.60 is moderate, 0.61–0.80 is good, 0.81–0.99 is very good, and 1 represents complete agreement. Inter-test agreement was also analyzed by computing the intraclass correlation coefficient (ICC). Interobserver agreement between the two reviewers was analyzed in a similar fashion. Proportional differences were analyzed using a two-tailed Fisher’s exact test. A statistical value of p < 0.05 was considered statistically significant.
Results
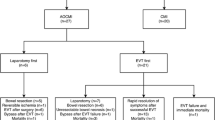
Thirty-two patients who underwent MRA for evaluation of mesenteric ischemia within 3 weeks of a contrast-enhanced abdominal/pelvic CT were included in this study (17 women, 15 men). The average patient age was 63.7 years. The data are summarized in Table 1. Of 32 patients, 10 were ultimately found to have bowel ischemia (1 case of AMI, 9 cases of IC), confirmed at endoscopy or surgery. Correlative bowel findings were identified by both readers on the CT examination for all 10 of these patients. However, correlative bowel findings on MR were identified in only 7 cases by reader 1 (p = 0.21) and 5 cases by reader 2 (p = 0.03) (Figs. 1, 2, 3). Overall, bowel findings were identified by reader 1 in 17 patients on CT and 10 patients on MRA (p = 0.13) and by reader 2 in 15 patients on CT and 12 on MRA (p = 0.61).
A 72-year-old woman with nonocclusive ischemic colitis of the colonic hepatic flexure. A Axial portal venous phase contrast-enhanced CT (CE-CT) demonstrating concentric thickening of the hepatic flexure (arrow). B Axial CE-CT demonstrating a patent superior mesenteric artery (arrow). C Coronal T2-weighted single-shot fast spin echo MRI demonstrating mild, less conspicuous thickening of the hepatic flexure (arrow). D Sagittal T1-weighted fat-suppressed 3D spoiled gradient-recalled echo contrast-enhanced MRA demonstrating a patent superior mesenteric artery (arrow). Ischemic colitis was confirmed at endoscopy.
A 71-year-old woman with ischemic colitis of the descending colon. A Axial portal venous phase contrast-enhanced CT (CE-CT) demonstrating narrowing of the proximal celiac artery, interpreted as mild and moderate stenosis by the two readers (arrow). B Sagittal T1-weighted fat-suppressed 3D spoiled gradient-recalled echo MRA (3D SPGR) demonstrating severe stenosis of the proximal celiac artery with post-stenotic dilatation. C Axial CE-CT demonstrating apparent moderate narrowing of the proximal superior mesenteric artery (arrow). D Sagittal T1-weighted 3D SPGR MRA demonstrating no stenosis of the superior mesenteric artery (arrow). F Coronal T2-weighted single-shot fast spin echo MRI demonstrating thickening of the distal descending colon (arrow). E Axial CE-CT demonstrating thickening and pericolonic fat stranding of the descending colon (arrow). Ischemic colitis was confirmed at endoscopy.
A 84-year-old man with nonocclusive ischemic colitis of the descending colon. A Coronal portal venous phase contrast-enhanced CT (CE-CT) demonstrating long-segment mural thickening and pericolonic fat stranding of the descending colon (arrow). B Axial CE-CT demonstrating a patent inferior mesenteric artery (arrow). C Coronal T2-weighted single-shot fast spin echo MRI demonstrating mild, less conspicuous thickening of the descending colon (arrow). D Coronal T1-weighted fat-suppressed 3D spoiled gradient-recalled echo MRA demonstrating a patent inferior mesenteric artery (arrow). Ischemic colitis was confirmed at endoscopy.
Regarding outcomes, the single patient with AMI underwent exploratory laparotomy with small bowel resection and SMA embolectomy. All nine patients with ischemic colitis were successfully managed conservatively with intravenous hydration and bowel rest. Of the patients who did not go to surgery or endoscopy, none were diagnosed with ischemic colitis, and all were assigned alternative diagnoses for their clinical presentation.
Substantial intraobserver agreement for both readers was found between portal venous phase CT and MRA for grading of stenosis severity assessed for the CA, SMA, and IMA, and for the aggregate of all three vessels (Table 2). The aggregate κ was 0.68 for reader 1 and 0.63 for reader 2. This was the highest for the SMA for both the readers (κ of 0.82 for reader 1 and 0.76 for reader 2). Comparing agreement between the two readers for each modality (Table 3), substantially higher agreement was found for the superior and inferior mesenteric arteries than the CA with CT and MRA. Agreement for grading of the CA was higher with CT compared with MRA.
Additional and alternative diagnoses made from the MRA examinations performed after portal venous phase CT were also analyzed. Adenomyosis was identified on an MRA examination, and in another patient, cholelithiasis and possible choledocholithiasis occult on CT was identified. Otherwise, no additional or alternative diagnoses were identified on the subsequent MRA that were unapparent on the initial portal venous CT. Based on the clinical record, no change in final diagnosis occurred based on the MRA report. A specific description of patency of the mesenteric vasculature was supplied on CT reports in 10 of 32 CT reports, and 7 of 10 reports in patients with bowel findings of mesenteric ischemia (p < 0.01). Vessel patency descriptions were supplied on all 32 MRA reports.
Discussion
To our knowledge, there has been no previous study comparing single-phase portal venous CT and MRA in the assessment of bowel ischemia and the mesenteric vasculature. This represents an important comparison because of the nonspecific presentation of bowel ischemia and likelihood that patients presenting to the emergency room with will undergo a standard portal venous CT as opposed to CTA as their initial diagnostic imaging study. In a recent study of CT ordering patterns in a tertiary level 1 trauma center [17], 8.1% of patients who presented to the emergency room underwent a CT of the abdomen and pelvis, including 38.5% of patients presenting with abdominal pain. It is likely that only a small minority of those CT examinations were performed with a dedicated angiographic protocol to assess for mesenteric ischemia. In our study, only 31% of the CT reports for patients who subsequently underwent MRA included a description of mesenteric vessel findings. It is possible that if specific comments regarding the mesenteric vasculature had been provided on the initial CT report, no subsequent MRA would have been ordered as the necessary clinical information would be available.
The results of the study confirm our hypothesis that portal venous phase CT and MRA demonstrate a high degree of concordance in grading mesenteric vascular stenoses. The κ values of 0.69 and 0.62 for all vessels indicate substantial agreement between CT and MRA, the highest for the SMA (κ = 0.82 and 0.77). With appropriate bolus timing and thin slice thickness being the norm on standard portal venous CT imaging of the abdomen and pelvis at our institution, nonangiographic CT equaled the performance of MRA in our study in identifying cases of acute mesenteric occlusion. MRA provided little to no new diagnostic information in most cases. While there were instances in which bowel abnormalities were identified on CT and not subsequent MRA, the differences in detection were not statistically significant and could also be accounted for by the time lag between the initial CT and subsequent MRA examination. The CT findings may also have been of questionable importance given normal biopsy results in a few cases.
Based on our results, one may question what the role is for MRA in further evaluation for ABI after portal venous CT. In our series, portal venous CT correctly identified cases of colitis without instances in which MRA subsequently identified a case missed by CT. Ischemic colitis, by its pathophysiologic nature, is most frequently nonocclusive, and the combination of bowel findings and mesenteric vascular assessment from standard portal venous phase CT should suffice for cross-sectional imaging in the majority of patients and correctly guide the clinician toward colonoscopy as the next potential diagnostic step in management. Performing MRA after CT did not affect patient outcomes in this series, as bowel findings from CT led to the definitive endoscopic or surgical evaluation and the single patient who underwent surgical intervention had concordant findings of SMA occlusion on both CT and MRA. The few additional findings made by MRA were not described as final causative diagnoses for any of the patients in this series.
Limitations of this study include its retrospective design and small patient sample size. Patients who received noncontrast CT examinations followed by MRA were excluded from this study as the presence of contrast enhancement on the initial CT examination was necessary for evaluation of vascular stenoses. The number of patients with acute mesenteric occlusion as a cause of bowel ischemia were low, likely due to the fact that this would be detected on initial CT evaluation and thus preclude the need for subsequent MRA imaging. Patients who undergo mesenteric ischemia protocol CT angiography as their initial diagnostic study are unlikely to go on for further investigation with MRA. Thus, the number of patients eligible for this study is limited and includes a higher proportion of patients with IC than AMI. Conventional angiography was not used as the reference standard for assessing vessel stenosis and patency as no patients in the study underwent angiography as part of their evaluation, but the study was designed to assess concordance rather than accuracy. Another possible limitation could be the influence of reviewing the initial CT examination prior to interpreting the MRA images, which was avoided in this study by reviewing the MRA prior to the CT with a washout period. Future avenues for research include investigating patients who underwent noncontrast CT as their initial diagnostic study followed by MRA to assess for AMI to determine how frequently clinically relevant mesenteric vascular disease is found by MRA in the absence of bowel findings on noncontrast CT.
In summary, routine single-phase portal venous CT and MRA are highly concordant in evaluation of the mesenteric vasculature. Given how frequently single-phase portal venous phase CT is used as the first-line diagnostic imaging study for emergency department patients presenting with abdominal pain, reporting of mesenteric vascular findings should be considered standard practice, which may obviate subsequent clinical requests for MRA. A patient with IC diagnosed on portal venous CT should not require subsequent imaging with MRA as little value is added.
References
Acosta S (2010) Epidemiology of mesenteric vascular disease: clinical implications. Semin Vasc Surg 23:4–8. doi:10.1053/j.semvascsurg.2009.12.001
Menke J (2010) Diagnostic accuracy of multidetector CT in acute mesenteric Ischemia: systematic review and meta-analysis. Radiology 256:93–101. doi:10.1148/radiol.10091938
Wyers MC (2010) Acute mesenteric ischemia: diagnostic approach and surgical treatment. Semin Vasc Surg 23:9–20. doi:10.1053/j.semvascsurg.2009.12.002
Gore RM, Thakrar KH, Mehta UK, et al. (2008) Imaging in intestinal ischemic disorders. Clin Gastroenterol Hepatol 6:849–858. doi:10.1016/j.cgh.2008.05.007
Reginelli A, Iacobellis F, Berritto D, et al. (2013) Mesenteric ischemia: the importance of differential diagnosis for the surgeon. BMC Surg 13:S51. doi:10.1186/1471-2482-13-S2-S51
Turkbey B, Akpinar E, Cil B, et al. (2008) Utility of MDCT in emergency setting of acute mesenteric ischemia. Diagn Interv Radiol . doi:10.4261/1305-3825.DIR.1597-07.3
Acosta S, Björck M (2014) Modern treatment of acute mesenteric ischaemia. Br J Surg 101:e100–e108. doi:10.1002/bjs.9330
Taourel P, Aufort S, Merigeaud S, et al. (2008) Imaging of ischemic colitis. Radiol Clin N Am 46:909–924. doi:10.1016/j.rcl.2008.06.003
Iacobellis F, Berritto D, Fleischmann D, et al. (2014) CT findings in acute, subacute, and chronic ischemic colitis: suggestions for diagnosis. Biomed Res Int 2014:895248. doi:10.1155/2014/895248
Washington C, Carmichael J (2012) Management of ischemic colitis. Clin Colon Rectal Surg 25:228–235. doi:10.1055/s-0032-1329534
Mazzei M, Guerrini S, Squitieri N, et al. (2013) Magnetic resonance imaging: Is there a role in clinical management for acute ischemic colitis? World J Gastroenterol 19:1256–1263. doi:10.3748/wjg.v19.i8.1256
Barmase M, Kang M, Wig J, et al. (2011) Role of multidetector CT angiography in the evaluation of suspected mesenteric ischemia. Eur J Radiol 80:e582–e587. doi:10.1016/j.ejrad.2011.09.015
Ofer A, Abadi S, Nitecki S, et al. (2009) Multidetector CT angiography in the evaluation of acute mesenteric ischemia. Eur Radiol 19:24–30. doi:10.1007/s00330-008-1124-5
Schaefer PJ, Boudghene FP, Brambs HJ, et al. (2006) Abdominal and iliac arterial stenoses: comparative double-blinded randomized study of diagnostic accuracy of 3D MR angiography with gadodiamide or gadopentetate dimeglumine. Radiology 238:827–840. doi:10.1148/radiol.2383041769
Schaefer P, Pfarr J, Trentmann J, et al. (2013) Comparison of noninvasive imaging modalities for stenosis grading in mesenteric arteries. RöFo—Fortschritte auf dem Gebiet der Röntgenstrahlen und der bildgebenden Verfahren 185:628–634. doi:10.1055/s-0033-1335212
Oliva IB, Davarpanah AH, Rybicki FJ, et al. (2013) ACR appropriateness criteria® imaging of mesenteric ischemia. Abdom Imaging 38:714–719. doi:10.1007/s00261-012-9975-2
Levine MB, Moore AB, Franck C, et al. (2013) Variation in use of all types of computed tomography by emergency physicians. Am J Emerg Med 31:1437–1442. doi:10.1016/j.ajem.2013.07.003
Acknowledgments
The authors would like to acknowledge the contributions of Mark Hammer, M.D., from the Mallinckrodt Institute of Radiology
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shetty, A.S., Mellnick, V.M., Raptis, C. et al. Limited utility of MRA for acute bowel ischemia after portal venous phase CT. Abdom Imaging 40, 3020–3028 (2015). https://doi.org/10.1007/s00261-015-0492-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-015-0492-y