Abstract
Purpose
Positron emission tomography (PET)/computed tomography (CT) with 68Ga-labelled 1,4,7,10-tetraazacyclododecane-N,N′,N″,N″‘-tetraacetic acid-d-Phe1-Tyr3-octreotide (DOTATOC) has been accepted as a diagnostic imaging tool especially for patients with neuroendocrine tumours. However, its clinical usefulness for restaging of renal cell carcinoma (RCC) has not been fully investigated. This retrospective study was performed to elucidate the clinical value of PET/CT using 68Ga-DOTATOC in patients with known or suspected recurrent RCC.
Methods
We analysed 25 consecutive patients who underwent DOTATOC-PET/CT scans after surgery for RCC (23 clear cell, 1 papillary, 1 unclassified). PET/CT findings were reviewed and the detection rate was calculated on a patient and lesion basis. The detectability was compared in patients who also underwent PET/CT scans with 18F-fluorodeoxyglucose (FDG). Histopathological findings or clinical follow-up were used as the reference standard.
Results
Based on the final diagnosis, 76 recurrent or metastatic lesions were confirmed in this population. Of these lesions, 66 lesions in 22 patients were positive by DOTATOC-PET/CT. The patient-based and lesion-based sensitivity was 88% (22/25) and 87% (66/76), respectively. Twelve patients underwent both DOTATOC-PET/CT and FDG-PET/CT. The lesion-based sensitivity of DOTATOC was 74% (20/27), while that of FDG was 59% (16/27). Eight lesions were identified only by DOTATOC, but four lesions from papillary RCC were detected only by FDG.
Conclusion
Our data indicate that DOTATOC-PET/CT would be useful for detecting recurrent foci in patients with clear cell RCC. DOTATOC-PET/CT and FDG-PET/CT are considered to have complementary roles.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) represents 2–3% of all adult cancers and is the third most common genitourinary malignancy. The incidence of RCC has increased during the past several years, contributing to a steadily increasing mortality rate [1,2,3]. The most common histological subtype of RCC is clear cell RCC, followed by papillary RCC and chromophobe RCC. With the recent progress in diagnostic imaging techniques, RCC can now be diagnosed at an early stage; however, approximately 20% of patients undergoing curative nephrectomy subsequently develop metastasis during the follow-up period [4].
Positron emission tomography (PET)/computed tomography (CT) using 18F-fluorodeoxyglucose (FDG) has been widely used for restaging in various malignancies. A review article of RCC demonstrated that FDG-PET or PET/CT shows relatively high diagnostic performance, with a pooled sensitivity and specificity of 86% and 88%, respectively, according to a meta-analysis based on 14 studies [5]. In some cases, however, FDG-PET/CT yields inconclusive information in the clinical setting because of the lower FDG-avidity of tumours.
Some RCCs are somatostatin receptor-positive, predominantly expressing subtype 2 [6, 7]. Therefore, metastatic foci derived from RCC has been depicted by somatostatin receptor imaging using 111In-labelled compounds in some case reports [8, 9]. PET/CT using 68Ga-labelled 1,4,7,10-tetraazacyclo dodecane-N,N′,N″,N″‘-tetraacetic acid-D-Phe1-Tyr3-octreotide (DOTATOC) has been accepted as a diagnostic imaging tool, especially for neuroendocrine tumours [10, 11]. They have replaced 111In-labelled compounds in Europe and the United States because 68Ga-labelled PET tracers, including DOTATOC, have higher diagnostic performance [12]. However, the clinical usefulness of PET/CT with 68Ga-labelled PET tracers for recurrent RCC has not been fully investigated, although there are several case reports [13,14,15,16].
Therefore, the purpose of this retrospective study was to elucidate the clinical value of PET/CT using 68Ga -DOTATOC in patients with known or suspected recurrent RCC.
Patients and methods
Patients
We retrospectively analysed 25 patients with known or suspected recurrent RCC who underwent DOTATOC-PET/CT in our single institute. The patients comprised 19 men and six women with a mean age of 64.2 years (range, 38–86 years). Of the 25 patients, 23 had clear cell RCC, one had papillary RCC, and one had unclassified RCC. The ethics committee of our institution approved the study, and written informed consent was obtained from all patients.
PET/CT scanning
Approximately 150 MBq of 68Ga-DOTATOC (radiochemical purity of >95%, specific activity of approximately 10 MBq/nmol) was injected intravenously, and a whole-body PET/CT scan was performed approximately 60 min after injection using a combined PET/CT scanner (Discovery ST Elite or Discovery IQ; GE Healthcare, Waukesha, WI, USA). Initially, starting at the level of the thigh, a low-dose CT scan was performed with the following parameters: 40–60 mA, 120 kV, 0.6-s tube rotation, and 3.75-mm section thickness. The CT scan was acquired during shallow breathing and included the area from the upper thigh to the top of the skull. Immediately after the CT scan, a PET scan was acquired with an acquisition time of 3 min per bed position. The CT data were used for attenuation correction, and images were reconstructed using a commercial three-dimensional iterative reconstruction algorithm called VUE Point Plus (interval, 3.27 mm; 2 iterations and 14 subsets in Discovery ST Elite, and 4 iterations and 12 subsets in Discovery IQ).
Image analysis
Images were visually interpreted by at least two board-certified radiologists, who were also board-certified nuclear medicine physicians, on a consensus basis. Moderate to intense focal accumulations compared with the background, not considered physiological or noise, were regarded as abnormal and indicative of recurrence or metastasis. When faint or equivocal uptake in the lesions was clearly depicted on CT images, those lesions were read as negative in this study. If at least one lesion was positive in a patient with multiple lesions, the patient was counted as a true positive on a per-patient basis. In the quantitative analysis, the maximum standardised uptake value was calculated for each lesion when abnormal uptake indicating recurrence or metastasis was found. If the PET findings were negative but CT revealed a morphological abnormality (allowing us to measure a quantitative value) and the lesions were finally confirmed to be recurrent or metastatic sites, the regions of interest were determined with reference to the CT images. The sensitivity of DOTATOC-PET/CT was compared with that of FDG-PET/CT in 12 patients who underwent both scans (including 2 patients who underwent the examinations in other hospitals). In addition, cases in which unexpected lesions that had not been identified by conventional imaging modalities were depicted by DOTATOC-PET/CT, and cases in which DOTATOC-PET/CT findings were considered to affect the therapeutic management, were assessed as ‘additional information’ and ‘clinical impact’, respectively. When positive findings were finally considered irrelevant to RCC but clinically significant, we regarded them as additional information. The reference standard was the histopathological findings (n = 15) or clinical follow-up findings (n = 10), including the radiological findings, for at least 6 months except in one patient who died of metastatic disease 3 months later.
Statistical analysis
The detection rates of DOTATOC-PET/CT and FDG-PET/CT were compared using the McNemar test for paired proportions.
Results
Visual analysis
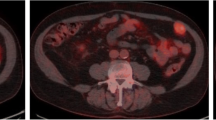
The patients’ profiles and PET results of the visual analysis are shown in Table 1, and the assessed lesions are summarised in Table 2, showing the averages and ranges of the quantitative values. Based on the final diagnosis, 76 recurrent or metastatic lesions were confirmed to be true lesions in this population. There were five lesions associated with local recurrence and 32, 15, 6, 5, 4, and 3 metastatic lesions to the bone, lung, pancreas, soft tissue, brain, and lymph nodes, respectively. The remaining six lesions comprised one metastatic lesion each to the liver, parathyroid, contralateral kidney, and mesentery and two metastatic lesions to the adrenal glands. A representative case in which metastasis to the parathyroid was unexpectedly identified is shown in Fig. 1. Of these lesions, 66 lesions in 22 patients were positive on DOTATOC-PET/CT. The patient-based and lesion-based sensitivity was 88% (22/25) and 87% (66/76), respectively. With respect to location, the detection rates for local recurrence and bone, lung, pancreatic, soft tissue, brain, and nodal metastases were 60%, 97%, 87%, 83%, 100%, 100%, and 33%, respectively, with an average maximum standardised uptake value of 8.3, 7.6, 3.3, 11.6, 11.2, 5.9, and 2.5, respectively. Three positive lesions were finally confirmed not to be recurrence or metastasis. These lesions were a meningioma in one patient and two residual lesions of haemangioblastoma in another patient with von Hippel–Lindau disease; all were considered irrelevant to metastatic RCC. Therefore, the estimated positive predictive value was 96% (66/69) in this population.
A 66-year-old woman with recurrent clear cell renal cell carcinoma. Maximum-intensity projection (a), axial CT (b), and fused (c) images are demonstrated. After resection of the right femoral lesion, a DOTATOC-PET/CT scan demonstrated intense focal uptake around the left lobe of the thyroid gland (arrows) in addition to metastases to soft tissue (aarrowheads). Metastasis to the parathyroid was confirmed during surgery
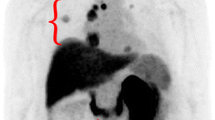
Comparison between DOTATOC and FDG
Twelve patients underwent both DOTATOC-PET/CT and FDG-PET/CT within 2 month of each other. The patient-based and lesion-based sensitivity of DOTATOC was 83% (10/12) and 74% (20/27), respectively, while that of FDG was 58% (7/12) and 59% (16/27), respectively. The differences in the patient-based and lesion-based sensitivities between the two methods were not statistically significant (p = 0.3711 and p = 0.3865, respectively). Eight lesions were identified only by DOTATOC, but four lesions in one patient with papillary RCC were detected only by FDG (Fig. 2). Figure 3 shows a scatter plot of 24 measurable lesions in patients who underwent both scans.
A 38-year-old man with recurrent papillary renal cell carcinoma. Maximum intensity projection images of FDG-PET and DOTATOC-PET (a) and axial slices of fusion images of both tracers (b) are demonstrated. No abnormal uptake is seen in DOTATOC-PET, but metastases to the bone (arrows) and lung (arrowheads) are clearly depicted in FDG-PET/CT. Focal uptakes indicating a left supraclavicular lymph node metastasis and local recurrence are also demonstrated in FDG-PET (asmall arrows)
Additional information and clinical impact
Table 3 summarises the additional information and clinical impact of DOTATOC-PET/CT. Among all 25 patients, additional information was obtained by DOTATOC-PET/CT for 9 patients (36%), including a meningioma and residual lesion of haemangioblastoma (irrelevant to recurrent RCC). These additional findings were considered to have affected the therapeutic strategy in three patients (12%).
Discussion
DOTATOC-PET/CT identified more recurrent or metastatic lesions with substantially high uptake after surgical treatment of RCC, especially clear cell RCC. However, some lesions with FDG avidity were not detected by DOTATOC-PET/CT. Our preliminary data indicate that DOTATOC-PET/CT may have a complimentary role in the detection of recurrent tumours in the postoperative state of RCC.
Several case reports have described positive findings of metastasis by 68Ga-DOTA peptide PET/CT as well as by somatostatin receptor scintigraphy using 111In-pentetreotide after nephrectomy for RCC [8, 9, 13,14,15]. In these reported cases, pancreatic tumours had been suspected to be a neuroendocrine tumour, and somatostatin receptor imaging revealed positive accumulation with confirmation of metastasis from RCC. It seems difficult to differentiate between pancreatic neuroendocrine tumours and pancreatic metastasis by somatostatin receptor imaging and conventional morphological imaging. The patient’s history may be useful in the consideration of differential diagnoses, but histopathological confirmation is still necessary for the final diagnosis.
In the present study, uptake of DOTATOC tended to be higher than uptake of FDG in most patients, among whom clear cell RCC was predominant in our series. However, in one patient who was confirmed to have papillary carcinoma, the lesions were depicted as a more strongly hypermetabolic area by FDG than by DOTATOC. We speculate that expression of somatostatin receptors may depend on the histopathological type of RCC, although Reubi and Kvols [6] stated that no evident correlations were found between the somatostatin receptor status in the tumour and the histopathological type or grade of the tumour by receptor autoradiography in 39 surgically removed human RCCs. Nevertheless, because only one patient had papillary carcinoma in our population, whether recurrent foci derived from papillary carcinoma tend to have lower expression of somatostatin receptors remains unknown. Further examinations involving more patients are needed to address this issue.
Compared with the detection rate in many lesions, the detection rate of nodal metastasis was relatively poor (sensitivity of only 33%). Three lesions were finally confirmed to be nodal metastasis from RCC. Of these three nodal metastases, one lesion of papillary RCC and one histologically confirmed para-aortic node (38 mm in size) from clear cell RCC were negative by DOTATOC-PET. Because the number of assessed lesions was small in this population, more cases are needed to determine the sensitivity for nodal metastasis.
A rare case in which unexpected metastasis to the parathyroid was confirmed by resection was encountered in the present study. In addition, DOTATOC-PET/CT depicted meningioma that was not associated with RCC as an unexpected finding. Whole-body DOTATOC-PET/CT would contribute to the detection of various unexpected findings, including soft tissue metastasis as has been demonstrated in a recent article [16], although the frequency may be not as high as that of FDG-PET/CT. Overall, additional information was obtained in about one-third of cases in the present study, which is considered comparable with FDG-PET for other malignancies. Therapeutic management was altered in only 10% of patients in this population, which is comparable with the frequency when we applied FDG-PET/CT to the restaging of RCC [17]. Patients with multiple metastases receive anti-cancer and/or molecular-targeted drugs. Therefore, therapeutic management is basically unchanged by the acquired findings of diagnostic imaging. We believe that the clinical impact is influenced by patient selection, and we need to consider when to apply this technique in restaging in terms of improving patients’ quality of life and cost effectiveness.
Residual haemangioblastoma in a patient with von Hippel–Lindau disease was also depicted by DOTATOC (images not shown). RCC is known to occur in patients with von Hippel–Lindau disease because of somatic mutations of the von Hippel–Lindau tumour suppressor gene [18]; haemangioblastoma and pancreatic neuroendocrine tumours can also occur as a result. Abnormal uptake in these lesions may be a potential pitfall when interpreting images in the postoperative state of RCC.
With respect to PET tracers other than FDG, some articles have described the clinical utility of prostate-specific membrane antigen (PSMA)-targeting tracers [19, 20], which have been widely accepted for prostate cancer [21, 22]. Interestingly, recurrent foci can be depicted by these tracers in clear cell RCC, while lesions are not always positive in non-clear cell RCC, including papillary RCC [23]. This tendency is similar to our somatostatin receptor imaging-based findings. The superiority of the diagnostic performance between somatostatin receptor-directed PET/CT and PSMA-directed PET/CT should be investigated in the future.
This study has some limitations. First, our preliminary evaluation included only 25 patients. Because of the small sample size, further studies with more patients are warranted. We could not obtain histopathological confirmation of the final diagnosis for all lesions because of ethical issues. This is a common limitation in clinical research, and some lesions considered to be true positive might have been false positive, resulting in overestimation of the sensitivity. However, all findings were verified by other imaging modalities and the clinical course during the follow-up period. We observed only one case of papillary RCC and one case of undifferentiated RCC. The diagnostic performance of DOTATOC-PET/CT for these rare histological types should be evaluated in the future. Finally, because at least one true positive metastatic or recurrent lesion was confirmed among all patients in this population, there were no cases in which recurrence had been suspected but no recurrence was finally confirmed. Therefore, the patient-based specificity was not calculated.
In conclusion, DOTATOC-PET/CT is useful for detecting recurrent tumours after surgical treatment of clear cell RCC. In some cases, therapeutic management might be altered by additional information obtained by this technique. However, the diagnostic performance of DOTATOC-PET/CT in other histological types, such as papillary and chromophobe RCC, still needs to be investigated. Because DOTATOC-PET/CT seems to have a complementary role with FDG-PET/CT, it can be a useful option when FDG-PET/CT is inconclusive.
References
Rini BI, Campbell SC, Escudier B. Renal cell carcinoma. Lancet. 2009;373:1119–32.
Ljungberg B, Bensalah K, Canfield S, Dabestani S, Hofmann F, Hora M, et al. EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol. 2015;67:913–24.
Bedke J, Gauler T, Grünwald V, Hegele A, Herrmann E, Hinz S, et al. Systemic therapy in metastatic renal cell carcinoma. World J Urol. 2017;35:179–88.
Volpe A, Bollito E, Bozzola C, Di Domenico A, Bertolo R, Zegna L, et al. Classification of histologic patterns of pseudocapsular invasion in organ-confined renal cell carcinoma. Clin Genitourin Cancer. 2016;14:69–75.
Ma H, Shen G, Liu B, Yang Y, Ren P, Kuang A. Diagnostic performance of 18F-FDG PET or PET/CT in restaging renal cell carcinoma: a systematic review and meta-analysis. Nucl Med Commun. 2017;38:156–63.
Reubi JC, Kvols L. Somatostatin receptors in human renal cell carcinomas. Cancer Res. 1992;52:6074–8.
Vikić-Topić S, Raisch KP, Kvols LK, Vuk-Pavlović S. Expression of somatostatin receptor subtypes in breast carcinoma, carcinoid tumor, and renal cell carcinoma. J Clin Endocrinol Metab. 1995;80:2974–9.
Kassabian A, Stein J, Jabbour N, Parsa K, Skinner D, Parekh D, et al. Renal cell carcinoma metastatic to the pancreas: a single-institution series and review of the literature. Urology. 2000;56:211–5.
Chan K, Luong TV, Navalkissoor S. 111In-DTPA-octreotide SPECT (OctreoScan) uptake in metastatic renal cell carcinoma to the pancreas. Clin Nucl Med. 2018;43:e29–30.
Barrio M, Czernin J, Fanti S, Ambrosini V, Binse I, Du L, et al. The impact of somatostatin receptor-directed PET/CT on the management of patients with neuroendocrine tumor: a systematic review and meta-analysis. J Nucl Med. 2017;58:756–61.
Graham MM, Gu X, Ginader T, Breheny P, Sunderland JJ. (68)Ga-DOTATOC imaging of neuroendocrine tumors: a systematic review and metaanalysis. J Nucl Med. 2017;58:1452–8.
Deppen SA, Blume J, Bobbey AJ, Shah C, Graham MM, Lee P, et al. 68Ga-DOTATATE compared with 111In-DTPA-octreotide and conventional imaging for pulmonary and gastroenteropancreatic neuroendocrine tumors: a systematic review and meta-analysis. J Nucl Med. 2016;57:872–8.
Peter L, Sänger J, Hommann M, Baum RP, Kaemmerer D. Molecular imaging of late somatostatin receptor-positive metastases of renal cell carcinoma in the pancreas by 68Ga DOTATOC PET/CT: a rare differential diagnosis to multiple primary pancreatic neuroendocrine tumors. Clin Nucl Med. 2014;39:713–6.
Vamadevan S, Le K, Shen L, Loh H, Mansberg R. 68Ga-DOTATATE uptake in solitary pancreatic metastasis from clear cell renal Cancer. Clin Nucl Med. 2017;42:700–1.
Nadebaum DP, Lee ST, Nikfarjam M, Scott AM. Metastatic clear cell renal cell carcinoma demonstrating intense uptake on (68)Ga-DOTATATE positron emission tomography: three case reports and a review of the literature. World J Nucl Med. 2018;17:195–7.
Vamadevan S, Le K, Shen L, Stevanovic A, Loh H, Mansberg R. 68Ga-DOTATATE uptake in a soft tissue metastasis from clear cell renal cell cancer. Clin Nucl Med. 2018;43:44–5.
Nakatani K, Nakamoto Y, Saga T, Higashi T, Togashi K. The potential clinical value of FDG-PET for recurrent renal cell carcinoma. Eur J Radiol. 2011;79:29–35.
Kim WY, Kaelin WG. Role of VHL gene mutation in human cancer. J Clin Oncol. 2004;22:4991–5004.
Rowe SP, Gorin MA, Hammers HJ, Som Javadi M, Hawasli H, Szabo Z, et al. Imaging of metastatic clear cell renal cell carcinoma with PSMA-targeted 18F-DCFPyL PET/CT. Ann Nucl Med. 2015;29:877–82.
Siva S, Callahan J, Pryor D, Martin J, Lawrentschuk N, Hofman MS. Utility of (68) Ga prostate specific membrane antigen - positron emission tomography in diagnosis and response assessment of recurrent renal cell carcinoma. J Med Imaging Radiat Oncol. 2017;61:372–8.
Ceci F, Uprimny C, Nilica B, Geraldo L, Kendler D, Kroiss A, et al. (68)Ga-PSMA PET/CT for restaging recurrent prostate cancer: which factors are associated with PET/CT detection rate? Eur J Nucl Med Mol Imaging. 2015;42:1284–94.
Perera M, Papa N, Christidis D, Wetherell D, Hofman MS, Murphy DG, et al. Sensitivity, specificity, and predictors of positive (68)Ga-prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: a systematic review and meta-analysis. Eur Urol. 2016;70:926–37.
Yin Y, Campbell SP, Markowski MC, Pierorazio PM, Pomper MG, Allaf ME, et al. Inconsistent detection of sites of metastatic non-clear cell renal cell carcinoma with PSMA-targeted [(18)F]DCFPyL PET/CT. Mol Imaging Biol. 2018. https://doi.org/10.1007/s11307-018-1271-2.
Funding
This study was funded by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology, Japan (25461816).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the ethics committee of Kyoto University Graduate School and Faculty of Medicine Kyoto University Hospital (reference number C0454).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakamoto, Y., Ishimori, T., Shimizu, Y. et al. Clinical utility of 68Ga-DOTATOC positron emission tomography/computed tomography for recurrent renal cell carcinoma. Eur J Nucl Med Mol Imaging 46, 1524–1530 (2019). https://doi.org/10.1007/s00259-019-04298-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04298-4