Abstract
Purpose
Evidence to date on the unique female determinants of cardiovascular risk is inadequate. Positron Emission Tomography (PET) is considered to have the highest accuracy for the assessment of myocardial perfusion in patients with suspected coronary artery disease (CAD), but its long-term prognostic accuracy in women has not been established.
Methods
A total of 619 consecutive patients (138 women, mean age 60.0 ± 11.8 years) underwent clinically indicated 13N-ammonia PET at our institution and were followed up (median 5.7 years) for major adverse cardiovascular events (MACE) including cardiac death, nonfatal myocardial infarction, hospitalization for any cardiac reason and late revascularization.
Results
During follow-up, 271 patients had at least one cardiac event, including 64 cardiac deaths and 33 nonfatal myocardial infarctions. In both women and men, abnormal myocardial perfusion was associated with reduced event-free survival (log rank p < 0.001). In women, abnormal myocardial perfusion was associated with a higher risk of a worse outcome than in men (adjusted HR 4.1, 95% CI 1.8–9.0 in women; HR 2.4, 95% CI 1.5–3.8 in men; pinteraction < 0.001). In contrast, abnormal coronary flow reserve (CFR) was a significant predictor of 10-year MACE in men (p = 0.006) but not in women (p = NS). Accordingly, an interaction term of sex and abnormal myocardial perfusion or CFR was significant (p < 0.001).
Conclusion
While perfusion findings in 13N-ammonia PET provide effective risk stratification in women and men, CFR adds incremental prognostic value for long-term cardiac outcomes only in men. Refined strategies in noninvasive imaging are needed in women to improve CAD risk prediction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For more than two decades, cardiovascular mortality has been higher in women than in men, and, while recent declines in cardiovascular deaths in men have been dramatic, declines are significantly less in women [1, 2]. Despite considerable scientific advances, there are currently only limited data on the female-specific aspects of cardiovascular disease. Indeed, assessment of coronary artery disease (CAD) in women presents a major challenge as contemporary imaging approaches for the diagnosis of CAD all have substantial limitations in women resulting in a lower test accuracy than in men [3,4,5,6]. In fact, poor categorization of women as to their pretest CAD likelihood, technical artefact issues related to breast tissue, obesity and smaller heart size, greater prevalence of nonobstructive CAD, poorer exercise capacity and more recent concerns regarding radiation safety all limit accurate assessment of risk in this population [3, 5, 7,8,9].
Myocardial perfusion imaging (MPI) with 82Rb or 13N-ammonia positron emission tomography (PET) is less commonly performed than single-photon emission computed tomography (SPECT) because of higher costs as well as technical and logistic challenges associated with these radiotracers. However, PET has demonstrated excellent properties for the diagnosis of CAD and its diagnostic accuracy appears to be superior to those reported for other imaging modalities [10]. In addition, the long-term prognostic values of MPI and coronary flow reserve (CFR) assessed by 13N-ammonia PET have recently been demonstrated [10,11,12,13,14]. In women, PET MPI has several advantages over other imaging modalities including its high spatial and temporal resolution, excellent attenuation correction, high diagnostic accuracy and a favourable safety profile with an effective radiation dose of 2–3 mSv as well as the added value of CFR quantification, all of which may provide a significant advantage in the evaluation of women with suspected myocardial ischaemia [10, 15,16,17]. However, despite substantial literature over the past 25 years, sex-specific data on the long-term prognostic value of MPI and CFR assessed by PET are lacking. Given that studies to date have failed to explore unique female imaging targets as major determinants of cardiovascular risk, the aim of the present study was to evaluate the long-term prognostic value of 13N-ammonia PET in women and men with suspected myocardial perfusion abnormalities. In addition, the potential added value of CFR in women with and without myocardial ischaemia was assessed.
Materials and methods
Study population
Myocardial perfusion was assessed in 619 consecutive patients (138, 22%, women) who underwent 13N-ammonia PET between August 1995 and October 2006 at our institution because of suspicion of CAD. Quantification of CFR was available in a subpopulation of 229 patients (159 men and 70 women). Patients were stratified by sex and were assigned to normal or abnormal myocardial perfusion and/or global CFR for outcome assessment. In patients with repeat evaluations during the study period, only the earliest evaluable study was included. Demographic factors and key elements of each patient’s history, including symptoms (typical, atypical or nonanginal chest pain, shortness of breath), risk factors and medication use, were ascertained at the time of the study by patient interview and review of medical records. A prior diagnosis of obstructive CAD and a history of coronary revascularization were documented. Pretest CAD likelihood was calculated based on the patient’s age, sex and typicality of chest pain symptoms [18]. The study population was partly (n = 229 and n = 389) shared with the PET imaging registry reported elsewhere [13, 14].
Myocardial perfusion 13N-ammonia PET imaging protocol
All patients underwent 13N-ammonia myocardial perfusion PET as a 1-day protocol at rest and during adenosine stress at a standard rate (0.14 mg/min/kg) over 7 min, as previously described [13, 14]. Patients were asked to avoid caffeine intake during the 12 h preceding the PET study. The PET studies were performed on either a GE Advance PET scanner or a Discovery [LS/RX] PET/CT scanner (both GE Healthcare, Milwaukee, WI). Each acquisition was preceded by a CT transmission scan for photon attenuation correction. 13N-Ammonia was intravenously injected (700–900 MBq), and standardized rest and pharmacological stress imaging protocols were performed according to the American Society of Nuclear Cardiology guidelines [19].
Data reconstruction and image analysis
Images were reconstructed using filtered back projection, and for review the images were resliced into short-axis and vertical and horizontal long-axis orientations. Rest and stress images were visually scored using the 17-segment scoring system, and the percentage of abnormal myocardium during stress was determined from the summed stress score. A scan was considered normal if the summed stress score was <4 as previously reported [14]. Images were interpreted by two independent and experienced readers blinded to the clinical data. Divergent interpretations were resolved by consensus. The PMOD software package (versions 2.1 to 2.8; PMOD Technologies Ltd., Zurich, Switzerland) was used to quantify myocardial blood flow (MBF) by determining myocardial and blood pool time–activity curves corrected for radioisotope decay from the dynamic frames. MBF was estimated by model fitting of the blood pool and myocardial time–activity curves correcting for the partial volume effect and spillover, as previously described [14]. Although correcting baseline MBF for rate–pressure product (RPP), a parameter reflecting cardiac workload, has been shown to reduce variability in baseline MBF measurements in some studies [20], we did not normalize baseline MBF to RPP as this parameter was not retrieved in our patient sample. Per-patient global CFR was calculated as the ratio of stress to rest absolute MBF for the whole left ventricle and CFR >2.0 was considered normal [21].
Assessment of outcomes
Information on follow-up was obtained by telephone interview with the patient or a family member, from medical records and from the referring physician. Patients were followed for the occurrence of all-cause mortality and major adverse cardiac events (MACE) including cardiac death, nonfatal myocardial infarction, hospitalization for any cardiac reason and late revascularization. Patients who underwent early revascularization (within 60 days of 13N-ammonia PET) were excluded since these revascularizations may be considered to be triggered by the scan rather than to reflect the natural course of the disease. All patients were followed for a median of 5.8 years (interquartile range 3.9 to 7.4 years) for CAD-related events. Cardiac death was defined as fatal myocardial infarction, sudden cardiac death or death due to heart failure. All other deaths were categorized as all-cause deaths. The date of the last examination or consultation was used to determine follow-up.
Statistical analysis
Baseline characteristics are reported as rates with percentages for categorical variables and means with standard deviations for continuous variables. Clinical and anthropometric variables were compared between groups using the unpaired Student’s t test or the chi-squared test, as appropriate. For clinical convenience, CFR was displayed as a dichotomous variable using ≤2 as a cut-off value for an impaired ratio. The time to cardiac events was estimated using a Cox proportional hazards survival model, including assessment of univariate and multivariate associations between PET imaging variables and CAD mortality. The effect size of CFR on cardiac mortality was evaluated in a subgroup of 226 patients by constructing Cox proportional hazard models including CFR as a dichotomous predictor variable. Adjusted hazard ratios (HRs) with 95% confidence intervals (CIs) are reported. The multivariate model covariates included age, body mass index (BMI) and cardiovascular risk factors. To avoid overfitting, a history of CAD was not included in the multivariate model, as evidence of fixed or scarred myocardium would be summarized within the abnormal scan variable. A first-order interaction term of sex by abnormal perfusion or abnormal CFR was included in the model. Cumulative event-free survival curves for the primary MACE endpoint of cardiovascular death, nonfatal myocardial infarction, late revascularization and hospitalization for cardiac reasons were compared across dichotomous categories of impaired myocardial perfusion or CFR using Kaplan-Meier methodology and the log-rank test. A two-tailed p value of 0.05 was considered statistically significant. SPSS version 24.0 (IBM Corp., Armonk, NY) was used for all statistical analyses.
Results
Patient characteristics stratified by sex
A total of 619 consecutive patients (138 women; mean age 60.1 ± 11.2 years in men and 59.4 ± 13.9 years in women) underwent clinically indicated 13N-ammonia PET at our institution. Of these patients, 75% had previously been diagnosed with CAD. Accordingly, the average Framingham risk in our study population was 16.3% (9.2% in women, 18.1% in men, p < 0.001). Men had a higher BMI, were more often smokers, more often had dyslipidaemia or diabetes and more often had a prior myocardial infarction and/or revascularization, while women were more often symptomatic, with symptoms including angina (CCS class ≥2: 13% vs. 8.1%, p = 0.08) and dyspnoea (NYHA ≥2: 10.1% vs. 5%, p = 0.026; Table 1). Notably, women more often reported atypical chest pain than men (12.3% vs. 6.0%, p = 0.002). The age difference between men and women was not significant (NS). Baseline characteristics of the study population are presented in Table 1.
Myocardial perfusion findings
In the overall population, the uptake of 13N-ammonia was normal in 152 patients and abnormal in 461 patients. Women had a higher prevalence of reversible perfusion defects during stress (16.8% vs. 8.3% in men, p = 0.004). Conversely, perfusion defects at rest were more often found in men (41.7% vs. 18.2% in women, p < 0.001). In a subgroup of 229 patients in whom CFR values were available, CFR was found to be abnormal (≤2.0) in 116 (50.7%). Abnormal CFR ≤2.0 was detected in 42.9% of women and 54.1% of men (p = 0.12). Overall, baseline MBF and stress MBF values were higher in women than in men (0.98 ± 0.22 mL/min/g vs. 0.83 ± 0.28 mL/min/g, p < 0.001, and 2.33 ± 0.89 mL/min/g vs. 1.75 ± 0.70 mL/min/g, p = 0.001, respectively). Accordingly, CFR was slightly higher in women than in men (2.42 ± 0.96 vs. 2.17 ± 0.80, p = 0.036). In patients with a normal myocardial perfusion scan, abnormal CFR was observed in 38.5% of women (n = 20) and 39.2% of men (n = 20).
Clinical endpoints by sex and myocardial perfusion 13N-ammonia PET
During follow-up, 271 patients had at least one cardiac event, including 64 cardiac deaths and 33 nonfatal myocardial infarctions (Table 1). Accordingly, the cumulative 10-year event rate was 42.7% for MACE (i.e. cardiac death, nonfatal myocardial infarction, hospitalization for any cardiac reason and late revascularization), 5.1% for nonfatal myocardial infarction, 10.1% for cardiac death, and 17.2% for all-cause mortality. In detail, 5.8% of women and 11.7% of men died from cardiac causes (p = 0.046), while a nonfatal myocardial infarction occurred in 2.9% of women and 6.0% of men (p = 0.20, Table 1). Of women with abnormal myocardial perfusion, 25% experienced a MACE, while the cumulative 10-year MACE rate was very low in women with normal myocardial perfusion on 13N-ammonia PET (6.6%, p < 0.001 vs. women with abnormal myocardial perfusion; Fig. 1a). Similarly, of men with abnormal myocardial perfusion, 42.3% experienced a MACE during the 10-year follow-up, while a MACE was observed in only 5.0% of men with normal myocardial perfusion (p < 0.001 vs. abnormal myocardial perfusion; Fig. 1a). In patients with abnormal myocardial perfusion, 23.5% of men and 10.9% of women experienced a myocardial infarction or died during follow-up, while these events occurred in 3.5% of men and 4.4% of women) with normal myocardial perfusion (Fig. 1b). Abnormal CFR was associated with a higher rate of MACE in men (13.2% vs. 27.0%, p = 0.007) but not in women (7.1% vs. 11.4%, p = 0.23; Fig. 1c). Accordingly, a higher rate of MACE was observed in men with normal myocardial perfusion and abnormal CFR (5.9% vs. 11.8%, p = 0.05; Fig. 1d), but not in women (9.6% vs. 5.8%, p = 0.31). The lack of risk stratification by CFR in women persisted when different threshold values for abnormal CFR (1.5–2.5) were applied (data not shown).
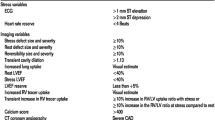
a Cumulative 10-year incidence of MACE in patients with abnormal myocardial perfusion. b Cumulative 10-year incidence of death and/or myocardial infarction in patients with abnormal myocardial perfusion. c Cumulative 10-year incidence of MACE in patients with abnormal CFR. d Cumulative 10-year incidence of MACE in patients with normal myocardial perfusion and abnormal CFR. CFR coronary flow reserve, MACE major adverse cardiac event, MI myocardial infarction. The chi-squared test was used for evaluation of differences between groups
Kaplan-Meier survival curves showed shorter times to MACE (event-free survival) in both women and men with abnormal myocardial perfusion scans (log rank p < 0.001, vs. normal myocardial perfusion; Fig. 2a, b). Similar tendencies were observed for the combined endpoint of myocardial infarction and death (log rank p = 0.005 for men and p = 0.022 for women, vs. normal myocardial perfusion; Fig. 2c, d) and when patients with prior myocardial infarction were excluded from the analysis (log rank p < 0.001 for men and women, vs. normal myocardial perfusion, data not shown). In contrast, shorter times to MACE and cardiac death (event-free survival) were observed in men with abnormal CFR, but not in women (for MACE, log rank p = 0.005 in men and p = 0.17 in women; and for cardiac death, log rank p = 0.001 and p = 0.53 in women, vs. normal CFR; Fig. 3a, b for MACE, and data not shown for cardiac death). Similarly, the time to the combined endpoint of myocardial infarction and death was shorter in men with abnormal CFR (log rank p = 0.016, vs. normal CFR; Fig. 3c), while no such risk stratification was seen in women (log rank p = 0.2, vs. normal CFR; Fig. 3d). The results were not significantly different when patients with prior myocardial infarction were excluded from the analysis (log rank p < 0.001 in men and p = 0.5 in women, data not shown).
As previous studies had indicated that absolute MBF during stress might be superior to CFR for the evaluation of cardiovascular risk [22], we stratified data by peak stress MBF (cut-off value 2.0 mL/min/g). Kaplan-Meier curves showed significantly shorter times to MACE (event-free survival) both in the overall population and in men with a stress MBF ≤2.0 mL/min/g (log rank p = 0.001 for the overall population and p = 0.007 for men, vs. stress MBF >2.0 mL/min/g; Fig. 4a, b). This risk stratification by stress MBF, however, was not observed in women (log rank p = 0.26 for stress MBF >2.0 mL/min/g vs. stress MBF ≤2.0 mL/min/g; Fig. 4c). In patients with normal perfusion, CFR did not allow prediction of events in the overall population (log rank p = 0.23; Fig. 5a) as the curves converged after 3 years of follow-up. However, when the data were stratified by sex, a significantly shorter time to MACE was observed in men with abnormal CFR, but not in women (log rank p = 0.031 for men and p = 0.7 for women; Fig. 5b, c).
Prognostic value of 13N-ammonia PET in women and men
Univariate and multivariate Cox regression analyses were performed to test the independence of the associations between 13N-ammonia PET findings and clinical endpoints at 10 years follow-up in women and men with adjustment for potential confounders (cardiovascular risk factors and left ventricular ejection fraction, LVEF). In unadjusted and adjusted models, abnormal myocardial perfusion assessed by 13N-ammonia PET was a strong predictor of 10-year MACE in both women and men (in women, adjusted HR 4.1, 95% CI 1.8–9.0, p = 0.001; in men, HR 2.4, 95% CI 1.5–3.8, p < 0.001; Table 2). The predicted risk of abnormal perfusion was higher in women than in men (pinteraction < 0.001). The addition of CFR to the model allowed further risk stratification in men, but not in women, for the full follow-up of 10 years (in men, adjusted HR 6.2, 95% CI 1.2–31.0, p = 0.029; in women, adjusted HR 0.2, 95% CI 0.2–3.9, p = NS; Table 2). Similarly, abnormal CFR alone as quantified by 13N-ammonia PET predicted th e10-year risk of MACE in men, but not in women (in men, adjusted HR 2.1, 95% CI 1.2–3.6, p = 0.006; in women, adjusted HR 2.0, 95% CI 0.6–6.7, p = NS; Table 2). Accordingly, in the unstratified dataset, a first-order interaction term of sex and abnormal myocardial perfusion or abnormal CFR was significant (p = 0.001 for abnormal myocardial perfusion, and p = 0.004 for CFR), confirming that the effect of CFR or myocardial perfusion is influenced by sex. The Cox proportional hazards survival models for 13N-ammonia PET findings estimating CAD mortality in women and men are presented in Table 2.
Discussion
Our study is the first to investigate the prognostic value of 13N-ammonia PET MPI in a sex-stratified population with a follow-up of 10 years. Our data illustrate that perfusion findings of 13N-ammonia PET provide independent long-term prognostic value in women and men, while the addition of CFR adds further risk stratification only in men. Indeed, women with a normal perfusion study on 13N-ammonia PET had an excellent prognosis as evidenced by a low cumulative MACE rate of 6.6% for the whole 10-year period, while event rates were slightly lower in men (5.0% for MACE). The observed event rates are well within the range of previously reported annualized values of 1.6% to 1.8% for MACE in patients with normal SPECT and PET scans, confirming that the present study included a representative patient population [17, 23]. Given the high prevalence (74.8%) of CAD in our population, our data indicate that normal perfusion PET may reliably exclude an adverse outcome even in the presence of coronary lesions. Conversely, abnormal myocardial perfusion was associated with adjusted HR for MACE of 4.1 in women and 2.4 in men, and cumulative 10-year MACE rates of 25.5% and 42.3%, respectively. Of note, in previous studies, annualized MACE rates have ranged widely in women with documented ischaemia, indicating that risk correlates that are undetected by contemporary imaging modalities may contribute to the varying clinical event rates observed in women [17, 24, 25].
Our data confirm previous evidence derived from SPECT studies, showing that MPI is able to effectively risk stratify women [26, 27]. Similarly, in a recent 82Rb PET study [17], abnormal stress perfusion was found to be independently predictive of cardiovascular mortality in women and men after a median follow-up of 2.2 years. Notably, in our study, survival curves continued to diverge over the entire 10-year follow-up period underlining the strong power of 13N-ammonia PET MPI to predict the long-term natural course of CAD in women and men. In addition, while previous studies have shown increased risk of cardiac events predominantly in patients with large and severe MPI defects, we found that 13N-ammonia PET perfusion defects were predictive regardless of size and severity of the perfusion abnormality.
One distinct advantage of stress PET MPI is the ability to calculate absolute blood flow across the coronary vessels, which allows calculation of PET CFR. Damped CFR suggests underlying vascular dysfunction and may aid in the detection of microvascular CAD, which may be particularly helpful in the evaluation of women with more prevalent nonobstructive CAD. However, in this study, while perfusion defects were an excellent predictor of adverse cardiovascular events in women, there was a significant influence of sex on the predictive power of CFR. In fact, CFR did not further stratify risk in women beyond PET MPI findings. This finding contrasts with the results of a recent study by Murthy et al. [28]. In their study, CFR predicted MACE in 813 women with no previous history of CAD and normal PET MPI during a median follow-up of 1.3 years [28]. However, it is difficult to compare our results and those of previous studies because inclusion criteria and follow-up times differ substantially across our studies. Indeed, we have previously shown that the predictive value of CFR as assessed by 13N-ammonia PET is maintained only over 3 years of follow-up, while survival curves converge during the following years, suggesting that normal CFR cannot predict disease onset in the long term [14]. We now extend this observation to a sex-stratified population by demonstrating that CFR predicts 10-year risk in men, but not in women.
The mechanisms relating to the lack of long-term prognostic value of CFR in women cannot be determined from our study and are likely to be multifactorial. For example, a higher resting coronary flow in women than in men has been widely reported, indicating that sex-specific normative values of CFR might be needed to reliably predict risk in both sexes [29,30,31,32]. However, when different threshold values for abnormal CFR, ranging from 1.5 to 2.5, were applied in the present study, the lack of risk stratification by CFR in women persisted. In addition, because absolute stress MBF had been suggested to be superior to CFR in the detection of CAD, we also stratified data by peak stress MBF [22]. Notably, while stress MBF ≤2 mL/min/g was associated with an increased event-rate in men, it did not predict cardiovascular risk in women, indicating that variables other than sex differences in baseline MBF may alter risk prediction in women. Indeed, sex-related differences in autonomic regulation [33, 34] and in responses to adenosine [35] as well as a higher susceptibility to stress-induced ischaemia [36] have all been reported in women, and may alter CFR quantification and risk stratification in unpredictable ways.
In addition, microvascular dysfunction is at least partly reversible and might be used to guide interventions aimed at reducing the burden of risk factors [37, 38]. Thus, sex differences in early treatment strategies based on 13N-ammonia PET findings might have influenced long-term prognosis in our population. Indeed, in this study the MACE rate in the first year was 4.5-fold higher in women with abnormal MPI than subsequent event rates (vs. 2.1-fold in men), suggesting that PET MPI findings play an important role in decision making in women. In contrast to our observations in women, abnormal CFR was a significant and independent predictor of MACE in men. Indeed, CFR improved risk stratification in men not only independently of perfusion findings, but also among those with visually normal PET scans. While previous studies have shown similar tendencies in populations without sex stratification and during shorter follow-up times (<3 years), in this study the predictive value of CFR in men was maintained to the end of the 10-year follow-up period [21, 39]. This suggests that impaired CFR may reflect extension of the disease beyond the epicardial coronary vessels down to the microcirculation, which indicates a more advanced disease stage.
Some limitations of our analyses merit consideration. First, our study was a single-centre retrospective study with a limited number of patients and was subject to all of the limitations of this study design. Accordingly, we were only able to adjust for a limited number of potential confounding variables in the survival analyses. Thus, it is likely that some residual confounding remains, despite adjustment for clinically relevant covariates. Similarly, we did not apply a semiquantitative measure of perfusion abnormality, such as scores for size and severity. These methods, however, have become very popular only over the past few years and were therefore not available for most of our scans that were acquired many years ago. Second, a limitation of the present study may be the use of global and not regional CFR, as regional findings may be diluted in the global value. However, global CFR values represent an integration of both extent and severity of perfusion defects, and the repeatability and reproducibility of global CFR are substantially superior to those of regional CFR [40]. Third, rest MBF measurements in our study were not normalized to RPP. The latter, however, has been shown to reduce heterogeneity of this variable within and between individuals in some studies [20]. Nevertheless, previous work has demonstrated excellent reproducibility and low variability of rest MBF as assessed by 13N-ammonia or 82Rb PET in patients with and without CAD, and the latter does not significantly change after correction for RPP [40,41,42]. Similarly, sex differences in baseline MBF have been shown to persist after correction for RPP, indicating that other variables account for the higher baseline MBF observed in women [31]. Fourth, while our unselected study population comprised patients with a high prevalence of CAD (>70%), and therefore reflected a real-world scenario, the populations investigated in previous studies included lower proportions of patients with CAD [17, 21]. Finally, given that our sample comprised patients seen in daily clinical routine, the results of the 13N-ammonia PET study were communicated to the referring physician. Thus, a bias caused by subsequent treatment decisions based on the MPI data cannot be completely ruled out in our study.
Taken together, our study indicates that risk stratification based on the presence or absence of abnormal perfusion as assessed by 13N-ammonia PET provides incremental long-term prognostic value in women and men, while CFR does not further delineate this classification in women. Our data underscore the limitations of contemporary imaging modalities in women and emphasize the need for further research to identify imaging targets reflecting female anatomy and physiology. Given the sizeable gap in the prognosis of CAD between women and men, integrated, sex-specific diagnostic strategies are needed to achieve sex equality in cardiovascular risk prediction.
References
Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016;37(42):3232–45. https://doi.org/10.1093/eurheartj/ehw334.
Wilmot KA, O’Flaherty M, Capewell S, Ford ES, Vaccarino V. Coronary heart disease mortality declines in the United States from 1979 through 2011: evidence for stagnation in young adults, especially women. Circulation. 2015;132(11):997–1002. https://doi.org/10.1161/CIRCULATIONAHA.115.015293.
Mieres JH, Gulati M, Bairey Merz N, Berman DS, Gerber TC, Hayes SN, et al. Role of noninvasive testing in the clinical evaluation of women with suspected ischemic heart disease: a consensus statement from the American Heart Association. Circulation. 2014;130(4):350–79. https://doi.org/10.1161/CIR.0000000000000061.
Gianrossi R, Detrano R, Mulvihill D, Lehmann K, Dubach P, Colombo A, et al. Exercise-induced ST depression in the diagnosis of coronary artery disease. A meta-analysis. Circulation. 1989;80(1):87–98.
Baldassarre LA, Raman SV, Min JK, Mieres JH, Gulati M, Wenger NK, et al. Noninvasive imaging to evaluate women with stable ischemic heart disease. JACC Cardiovasc Imaging. 2016;9(4):421–35. https://doi.org/10.1016/j.jcmg.2016.01.004.
Pepine CJ, Ferdinand KC, Shaw LJ, Light-McGroary KA, Shah RU, Gulati M, et al. Emergence of nonobstructive coronary artery disease: a woman’s problem and need for change in definition on angiography. J Am Coll Cardiol. 2015;66(17):1918–33. https://doi.org/10.1016/j.jacc.2015.08.876.
Sanders GD, Patel MR, Chatterjee R, Ross AK, Bastian LA, Coeytaux RR, et al. Noninvasive technologies for the diagnosis of coronary artery disease in women: future research needs: identification of future research needs from comparative effectiveness review no. 58. Rockville, MD: Agency for Healthcare Research and Quality (US); 2013.
Botvinick EH. Breast attenuation artifacts in Tl-201 scintigraphy. Radiology. 1988;168(3):878–9. https://doi.org/10.1148/radiology.168.3.878-c.
Hansen CL, Crabbe D, Rubin S. Lower diagnostic accuracy of thallium-201 SPECT myocardial perfusion imaging in women: an effect of smaller chamber size. J Am Coll Cardiol. 1996;28(5):1214–9. https://doi.org/10.1016/s0735-1097(96)00304-x.
Nandalur KR, Dwamena BA, Choudhri AF, Nandalur SR, Reddy P, Carlos RC. Diagnostic performance of positron emission tomography in the detection of coronary artery disease: a meta-analysis. Acad Radiol. 2008;15(4):444–51. https://doi.org/10.1016/j.acra.2007.08.012.
Kajander S, Joutsiniemi E, Saraste M, Pietila M, Ukkonen H, Saraste A, et al. Cardiac positron emission tomography/computed tomography imaging accurately detects anatomically and functionally significant coronary artery disease. Circulation. 2010;122(6):603–13. https://doi.org/10.1161/circulationaha.109.915009.
Jaarsma C, Leiner T, Bekkers SC, Crijns HJ, Wildberger JE, Nagel E, et al. Diagnostic performance of noninvasive myocardial perfusion imaging using single-photon emission computed tomography, cardiac magnetic resonance, and positron emission tomography imaging for the detection of obstructive coronary artery disease: a meta-analysis. J Am Coll Cardiol. 2012;59(19):1719–28. https://doi.org/10.1016/j.jacc.2011.12.040.
Fiechter M, Gebhard C, Ghadri JR, Fuchs TA, Pazhenkottil AP, Nkoulou RN, et al. Myocardial perfusion imaging with 13N-ammonia PET is a strong predictor for outcome. Int J Cardiol. 2013;167(3):1023–6. https://doi.org/10.1016/j.ijcard.2012.03.076.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve. J Am Coll Cardiol. 2009;54(2):150–6. https://doi.org/10.1016/j.jacc.2009.02.069.
Bateman TM, Heller GV, McGhie AI, Friedman JD, Case JA, Bryngelson JR, et al. Diagnostic accuracy of rest/stress ECG-gated Rb-82 myocardial perfusion PET: comparison with ECG-gated Tc-99m sestamibi SPECT. J Nucl Cardiol. 2006;13(1):24–33. https://doi.org/10.1016/j.nuclcard.2005.12.004.
Neglia D, Rovai D, Caselli C, Pietila M, Teresinska A, Aguade-Bruix S, et al. Detection of significant coronary artery disease by noninvasive anatomical and functional imaging. Circ Cardiovasc Imaging. 2015;8:e002179. https://doi.org/10.1161/circimaging.114.002179.
Kay J, Dorbala S, Goyal A, Fazel R, Di Carli MF, Einstein AJ, et al. Influence of sex on risk stratification with stress myocardial perfusion Rb-82 positron emission tomography: results from the PET (Positron Emission Tomography) Prognosis Multicenter Registry. J Am Coll Cardiol. 2013;62(20):1866–76. https://doi.org/10.1016/j.jacc.2013.06.017.
D’Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743–53. https://doi.org/10.1161/circulationaha.107.699579.
Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. Circulation. 2009;119(22):e561–87. https://doi.org/10.1161/circulationaha.109.192519.
Nagamachi S, Czernin J, Kim AS, Sun KT, Bottcher M, Phelps ME, et al. Reproducibility of measurements of regional resting and hyperemic myocardial blood flow assessed with PET. J Nucl Med. 1996;37(10):1626–31.
Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Di Carli G, et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation. 2011;124(20):2215–24. https://doi.org/10.1161/circulationaha.111.050427.
Joutsiniemi E, Saraste A, Pietila M, Maki M, Kajander S, Ukkonen H, et al. Absolute flow or myocardial flow reserve for the detection of significant coronary artery disease? Eur Heart J Cardiovasc Imaging. 2014;15(6):659–65. https://doi.org/10.1093/ehjci/jet274.
Van Tosh A, Supino PG, Nichols KJ, Garza D, Horowitz SF, Reichek N. Prognosis of a normal positron emission tomography 82Rb myocardial perfusion imaging study in women with no history of coronary disease. Cardiology. 2010;117(4):301–6. https://doi.org/10.1159/000323841.
Shaw LJ, Bugiardini R, Merz CN. Women and ischemic heart disease: evolving knowledge. J Am Coll Cardiol. 2009;54(17):1561–75. https://doi.org/10.1016/j.jacc.2009.04.098.
Berman DS, Kang X, Hayes SW, Friedman JD, Cohen I, Abidov A, et al. Adenosine myocardial perfusion single-photon emission computed tomography in women compared with men. Impact of diabetes mellitus on incremental prognostic value and effect on patient management. J Am Coll Cardiol. 2003;41(7):1125–33.
Marwick TH, Shaw LJ, Lauer MS, Kesler K, Hachamovitch R, Heller GV, et al. The noninvasive prediction of cardiac mortality in men and women with known or suspected coronary artery disease. Economics of Noninvasive Diagnosis (END) Study Group. Am J Med. 1999;106(2):172–8.
Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol. 2004;11(2):171–85. https://doi.org/10.1016/j.nuclcard.2003.12.004.
Murthy VL, Naya M, Taqueti VR, Foster CR, Gaber M, Hainer J, et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation. 2014;129(24):2518–27. https://doi.org/10.1161/circulationaha.113.008507.
Johnson NP, Gould KL. Integrating noninvasive absolute flow, coronary flow reserve, and ischemic thresholds into a comprehensive map of physiological severity. JACC Cardiovasc Imaging. 2012;5(4):430–40. https://doi.org/10.1016/j.jcmg.2011.12.014.
Gould KL, Johnson NP, Bateman TM, Beanlands RS, Bengel FM, Bober R, et al. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol. 2013;62(18):1639–53. https://doi.org/10.1016/j.jacc.2013.07.076.
Chareonthaitawee P, Kaufmann PA, Rimoldi O, Camici PG. Heterogeneity of resting and hyperemic myocardial blood flow in healthy humans. Cardiovasc Res. 2001;50(1):151–61.
Range FT, Kies P, Schafers KP, Breithardt G, Schober O, Wichter T, et al. Sex differences in absolute myocardial perfusion. Non-invasive H2(15)O-PET in young healthy adults. Nuklearmedizin. 2016;55(5):196–202. https://doi.org/10.3413/Nukmed-0821-16-04.
Momen A, Gao Z, Cohen A, Khan T, Leuenberger UA, Sinoway LI. Coronary vasoconstrictor responses are attenuated in young women as compared with age-matched men. J Physiol. 2010;588(Pt 20):4007–16. https://doi.org/10.1113/jphysiol.2010.192492.
Kim A, Deo SH, Vianna LC, Balanos GM, Hartwich D, Fisher JP, et al. Sex differences in carotid baroreflex control of arterial blood pressure in humans: relative contribution of cardiac output and total vascular conductance. Am J Physiol Heart Circ Physiol. 2011;301(6):H2454–65. https://doi.org/10.1152/ajpheart.00772.2011.
Heaps CL, Bowles DK. Gender-specific K(+)-channel contribution to adenosine-induced relaxation in coronary arterioles. J Appl Physiol (1985). 2002;92(2):550–8. https://doi.org/10.1152/japplphysiol.00566.2001.
Vaccarino V, Wilmot K, Al Mheid I, Ramadan R, Pimple P, Shah AJ, et al. Sex differences in mental stress-induced myocardial ischemia in patients with coronary heart disease. J Am Heart Assoc. 2016;5:e003630. https://doi.org/10.1161/jaha.116.003630.
Eriksson BE, Tyni-Lenne R, Svedenhag J, Hallin R, Jensen-Urstad K, Jensen-Urstad M, et al. Physical training in syndrome X: physical training counteracts deconditioning and pain in syndrome X. J Am Coll Cardiol. 2000;36(5):1619–25.
Hambrecht R, Adams V, Erbs S, Linke A, Krankel N, Shu Y, et al. Regular physical activity improves endothelial function in patients with coronary artery disease by increasing phosphorylation of endothelial nitric oxide synthase. Circulation. 2003;107(25):3152–8. https://doi.org/10.1161/01.cir.0000074229.93804.5c.
Taqueti VR, Everett BM, Murthy VL, Gaber M, Foster CR, Hainer J, et al. Interaction of impaired coronary flow reserve and cardiomyocyte injury on adverse cardiovascular outcomes in patients without overt coronary artery disease. Circulation. 2015;131(6):528–35. https://doi.org/10.1161/circulationaha.114.009716.
Kaufmann PA, Gnecchi-Ruscone T, Yap JT, Rimoldi O, Camici PG. Assessment of the reproducibility of baseline and hyperemic myocardial blood flow measurements with 15O-labeled water and PET. J Nucl Med. 1999;40(11):1848–56.
Manabe O, Yoshinaga K, Katoh C, Naya M, de Kemp RA, Tamaki N. Repeatability of rest and hyperemic myocardial blood flow measurements with 82Rb dynamic PET. J Nucl Med. 2009;50(1):68–71. https://doi.org/10.2967/jnumed.108.055673.
Sawada S, Muzik O, Beanlands RS, Wolfe E, Hutchins GD, Schwaiger M. Interobserver and interstudy variability of myocardial blood flow and flow-reserve measurements with nitrogen 13 ammonia-labeled positron emission tomography. J Nucl Cardiol. 1995;2(5):413–22.
Funding
This study was funded by the Swiss National Science Foundation (SNSF), the Olga Mayenfisch Foundation, Switzerland, the OPO Foundation, Switzerland, the Novartis Foundation, Switzerland, and the Swissheart Foundation (to C.G.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
Our study was approved by the Cantonal Ethics Board in Zurich, Switzerland (BASEC No. 2017–01112). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards, and were conducted in accordance with institutional guidelines.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Gebhard, C., Fiechter, M., Herzog, B.A. et al. Sex differences in the long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography. Eur J Nucl Med Mol Imaging 45, 1964–1974 (2018). https://doi.org/10.1007/s00259-018-4046-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4046-8