Abstract
Purpose
To assess the localizing value of 18F-FDG PET in patients operated on for drug-resistant epilepsy due to focal cortical dysplasia type 2 (FCD2).
Methods
We analysed 18F-FDG PET scans from 103 consecutive patients (52 males, 7–65 years old) with histologically proven FCD2. PET and MRI data were first reviewed by visual analysis blinded to clinical information and FCD2 location. The additional value of electroclinical data and PET/MRI coregistration was assessed by comparison with pathological results and surgical outcomes.
Results
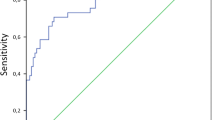
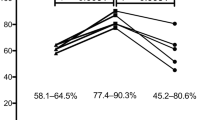
Visual analysis of PET scans showed focal or regional hypometabolism corresponding to the FCD2 in 45 patients (44%), but the findings were doubtful or misleading in 37 patients and negative in 21. When considering electroclinical data, positive localization was obtained in 73 patients, and this increased to 85 (83%) after coregistration of PET and MRI data. Under the same conditions, MRI was positive in 61 patients (59%), doubtful in 15 and negative in 27. The additional value of PET was predominant in patients negative or doubtful on MRI, localizing the FCD2 in 35 patients (83%). Interobserver agreement correlated with the grade of hypometabolism: it was good in patients with mild to severe hypometabolism (82–95%), but moderate in those with subtle/doubtful hypometabolism (45%). The main factors influencing positive PET localization were the grade of hypometabolism and the size of the FCD2 (P < 0.0001). Misleading location (nine patients) was associated with a small FCD2 in the mesial frontal and central regions. Following limited cortical resection mainly located in extratemporal areas (mean follow-up 5.6 years), a seizure-free outcome was achieved in 94% of patients, including Engel’s class IA in 72%.
Conclusion
In this series, 18F-FDG PET contributed to the localization of FCD2 in 83% of patients. This high localizing value was obtained by integration of electroclinical data and PET/MRI coregistration. This approach may help improve the surgical outcome in extratemporal epilepsy, even in patients negative on MRI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Focal cortical dysplasia type 2 (FCD2) is one of the most frequent pathologies in focal epilepsies that can be cured by surgery, in children as well as in adults [1]. These highly epileptogenic lesions are predominantly located in extratemporal areas, often involve the eloquent cortex, and remain difficult to detect even with optimal MRI [2, 3]. Improving the identification of such dysplastic lesions is crucial for referring patients for surgery and guiding the cortical resection. 18F-FDG PET has proved highly sensitive for the detection of FCD2, especially in patients negative on MRI [4, 5]. We aimed to assess the value of PET for localizing FCD2 in clinical practice. To this end, we compared the results of visual analysis alone with those obtained after integration of electroclinical data and coregistration of PET and MRI data in a large series of surgically treated patients. Our second goal was to assess the contribution of PET to the surgical outcome in this population.
Materials and methods
Patient population
From among 1,055 patients investigated by 18F-FDG PET for drug-resistant partial epilepsy at SHFJ, CEA (Orsay, France) between 2000 and 2016, we selected all patients in whom the diagnosis of FCD2 was suggested by MRI features and/or histologically confirmed after surgery. Some of these patients have been reported in previous studies [4, 6]. Inclusion criteria for the present study were: original PET and MRI files available for analysis on the workstation, surgery performed in the same institution (Centre Hospitalier Sainte-Anne) and histological diagnosis of FCD2. Among 112 selected patients, one was eliminated because histology was atypical and another because PET was performed after initial surgery, three others were not operated on despite typical FCD2 features on MRI, and four later patients were not included due to missing PET or MRI data. The final population consisted of 103 patients (52 males), including 31 children under 16 years of age. Their ages at PET examination ranged from 7 to 65 years (mean 24.8 years, SD 11.7 years). Age at epilepsy onset ranged from birth to 40 years (mean 7.1 years, SD 5.8 years) and epilepsy duration from 1 to 59 years (mean 17.7 years, SD 10.9 years). Most patients (80%) had high seizure frequency (one or more per day).
Presurgical work-up and surgery
Presurgical evaluation included video-EEG recordings, high-resolution MRI, functional MRI and 18F-FDG PET coregistered with MRI in all patients. In addition, 53 patients underwent stereoelectroencephalography (SEEG). Cortical resection was performed using microsurgical techniques, after multidisciplinary integration of preoperative data including the PET results. The diagnosis of FCD was established according to the ILAE classification [7]. Surgical outcome assessment was based on Engel’s classification [8].
Imaging data
MRI scans were performed using a 1.5-T magnet (Signa Excite; General Electric Healthcare, Milwaukee, WI, USA: 60 patients) and from 2010 using a 3-T MRI scanner (Discovery MR750; General Electric Healthcare: 43 patients). The MRI protocol included 3D T1-weighted 1.2-mm-thick contiguous slices, coronal T2-weighted and FLAIR (fluid-attenuated-inversion recovery) sequences. All MRI scans were reviewed by a trained neuroradiologist (C.M.) blinded to the PET results and localization of the lesions. MRI was classified as positive if the images demonstrated features characteristic of FCD2 [9] and doubtful if they showed only minor gyral abnormalities, and the findings were considered nonspecific and negative in the remaining cases.
18F-FDG PET examination was performed using either a head-dedicated PET camera (ECAT-953/31B; Siemens, Knoxville, TN, USA; 5.8 mm transverse, 5 mm axial resolution) in 9 patients or a 3D camera (HR+ CTI Exact; Siemens; 4.4 mm transverse, 4.2 mm axial resolution) in 58 patients, and then from 2009 a PET/CT system (Biograph 6; Siemens; 4.2 mm transverse, 4.5 mm axial resolution) in 36 patients. 18F-FDG was injected intravenously at a mean activity of 3 MBq/kg body weight. Images were acquired for 15–20 min starting 30 min after injection. Patients were studied in an awake, resting state in a quiet, dimly lit environment, and were carefully monitored for head movements and ictal events. Correction for attenuation was done using 68Ga/68Ge transmission scans for the ECAT/HR+ cameras and CT for the Biograph. No patient had seizures other than the usual type (i.e. secondary generalized) during the 7 days preceding the PET scan. Since most patients had a high frequency of seizures, 11 of them experienced a seizure less than 6 h before the PET scan and 21 others during the previous night without more precise information as to the time. In addition, 13 other patients had a seizure after injection of FDG and/or during the PET scan. However, seizures were brief (less than 30 s) and data were interpretable in all subjects except one, in whom PET was repeated in the interictal period.
Visual analysis was performed by an experienced nuclear physician (S.D.) using a semiquantitative grading of the metabolic changes. The look-up table roughly equally divided the colour scale with 80% upper scale normalization and 20% background noise, followed by a new upper scale normalization if necessary. Hypometabolism was classified as mild, moderate or severe according to the percentage SUV reduction (10–15%, 15–20%, >20%, respectively) and subtle/doubtful if <10%, in comparison with the contralateral symmetrical areas. PET and MRI images were coregistered either using Anatomist software (http://brainvisa.info) [10] or on a PET workstation (Siemens, GE). The location and extent of the metabolic abnormalities were classified as focal (involving a single gyrus), regional (involving several gyri in the same lobe) or widespread (involving the whole lobe or several lobes). Visual analysis of PET images was performed by one reader (S.D.), first blinded to the electroclinical data, then integrating this information and the coregistration with the MRI images. The second reader (F.C., epileptologist experienced in PET) reviewed the PET data with knowledge of the electroclinical data and after PET/MRI coregistration. Results were then compared with the preoperative report. The location of FCD2 was based on the MRI data, surgical findings and histology.
The visual PET findings were considered positively localizing when there was overlap between the hypometabolic area and the localization of FCD2, doubtful or misleading when hypometabolism was either subtle or detected in a lobe or a part of a lobe that did not contain the FCD2, and negative when no clear abnormalities were detected visually. PET/MRI coregistration was considered localizing (positive) if the hypometabolic area overlapped with the precise location of the FCD2, and nonlocalizing (negative) when only a doubtful hypometabolism was detected or when a misleading location was indicated (involving an area different from the FCD2, within the same lobe or not). The localizing value of PET was assessed according to the three types of analysis (visual alone, after integration of electroclinical data, and after PET/MRI coregistration). Interobserver agreement was assessed after integration of electroclinical and MRI data. It was considered fully concordant when the FCD2 was localized in the same location within the same lobe, partially concordant when the FCD2 was localized in the same lobe but not precisely at the same site, and discordant when the FCD2 was localized in a different lobe. Any disagreements were resolved by consensus. Of note, if the MRI findings were negative or doubtful, MRI images were reviewed after comparison with the PET images to search for mild structural abnormalities.
PET scans were performed as part of a research protocol until 2006 and thereafter as part of clinical routine. All patients provided informed consent before scanning. The study was approved by the Ethics Committee of Ile de France III and was found to conform to generally accepted scientific principles and ethical standards.
Statistical analysis
Statistical analysis was performed using SPSS Statistics (version 23) software. Several types of analysis were performed searching for correlations between the grade of hypometabolism and (1) demographic data (age at PET examination and epilepsy onset), (2) characteristics of epilepsy (duration, seizure frequency), (3) lobar location and size of FCD2 (gyral, infralobar, lobar) and (4) time between the last seizure and the PET examination (interictal if >6 h, peri-ictal if <6 h or during the PET scan). We also searched for factors influencing the localizing value of PET and interobserver agreement. Finally, we compared surgical outcome according to the positivity or negativity of MRI and PET, independently and in combination. We performed one-way ANOVA to analyse parametric variables and the chi-squared test for the effects of categorical variables. To assess factors influencing the localizing value of PET, a logistic multivariate regression analysis was done with localization by PET (positive versus negative) as the dependent variable and the variables hypometabolism grade, FCD2 size, localization, time since last seizure and type of camera as predictors. Surgical outcome was analysed by logistic regression with Engel’s class I and IA as dependent variables, and MRI and PET results (positive versus negative) as predictors. P values <0.05 were considered significant. For interobserver agreement, concordance analysis was conducted using the kappa index, classifying concordance as slight (0.00–0.20), fair (0.21–0.40), moderate (0.41–0.60), substantial (0.61–0.80), and almost perfect (0.81–1.00).
Results
PET analysis
Visual PET analysis detected hypometabolic areas concordant with the site of FCD2 in 45 patients (44%) but was negative, doubtful or misleading in the other patients. MRI was positive in 61 patients (59%), doubtful in 15 and negative in 27. When electroclinical data were taken into account, the proportion of patients with a positive localization by PET increased to 71%, and was higher in patients positive on MRI (79%) than in those negative/doubtful on MRI (60%). PET/MRI coregistration allowed the detection of a gyral, infralobar or lobar hypometabolism which was classified as subtle/doubtful (22 patients), mild (28 patients), moderate (33 patients) or severe (20 patients). This hypometabolism was fully concordant with the localization of FCD2 in 85 patients (PET-positive). However, in 18 other patients, the PET findings remained doubtful or misleading (PET-negative). PET was concordant with MRI in 50 MRI-positive patients (82%), either showing mild to severe hypometabolism (Fig. 1) or subtle/doubtful hypometabolism at the bottom of the sulcus (Fig. 2). In these latter patients, PET alone may be less sensitive than MRI, which was the case in six patients in this series. In five other patients, PET data were misleading, showing metabolic changes discordant with the structural abnormalities. However, three patients initially MRI-negative became positive after comparison of the MRI and PET data.
Axial 18F-FDG PET, MRI and coregistered PET/MRI images in a patient with a left central FCD2 (type 2B). Mild hypometabolism is apparent at the bottom of the dysplastic gyrus in the PET/MRI images without significant abnormalities on the PET image (MRI-positive, PET-positive after coregistration with MRI)
The major additional value of PET was found in 42 patients negative/doubtful on MRI (41%), in 35 (83%) of whom the FCD2 was localized (Figs. 3, 4 and 5). Of note, five patients negative/doubtful on both PET and MRI were positive on coregistered PET/MRI (Fig. 6). However, a doubtful/misleading localization was found in seven others. Therefore, the combination of visual analysis of 18F-FDG PET data, electroclinical data and MRI coregistration contributed to localizing the FCD2 in 85 patients (83%), including 35 patients negative/doubtful on MRI and three other patients in whom MRI became positive after comparison of the MRI and PET data. These results are summarized in Table 1.
Axial 18F-FDG PET, MRI and coregistered PET/MRI images in a patient with a left prefrontal FCD2 (type 2B). Mild focal hypometabolism is apparent in the PET image corresponding to a single hypometabolic gyrus in the left lateral prefrontal cortex. Note the relative hypometabolism in the mesial frontal cortex bilaterally, corresponding to ictal spread. On the MRI image (initially considered negative) a mild blurring is apparent at the bottom of the hypometabolic sulcus (MRI-negative changing to MRI-positive after coregistration with the PET image)
Coronal 18F-FDG PET, MRI and coregistered PET/MRI images in a patient with a small left mesial prefrontal FCD2 (type 2B). Mild hypometabolism is well localized in the left anterior cingulate gyrus corresponding to the dysplastic cortex, without structural changes visible on the MRI image (MRI-negative, PET-positive)
Axial 18F-FDG PET, MRI and coregistered PET/MRI images in a patient with a left inferior frontal FCD2 (type 2B). Doubtful abnormalities are present on PET the and MRI images independently, identified as a hypometabolic gyrus in the left inferior frontal gyrus on the PET/MRI coregistered image, corresponding to the dysplastic cortex (MRI-negative/doubtful, PET-negative/doubtful, PET/MRI-positive)
Factors influencing the localizing value of PET
The main factors influencing positive localization by PET were the grade of hypometabolism and the size of the FCD2 (P < 0.0001). Time since the last seizure was significantly correlated with the grade of hypometabolism, obtaining a peri-ictal PET did not change significantly the results considering the FCD2 localization. Logistic regression analysis indicated that only the grade of hypometabolism was significant (P = 0.012). FCD2 location may also play a role but did not reach the threshold of significance (P = 0.095). Predominance in extratemporal areas, especially the frontocentral areas (78 patients) is in line with the characteristics of FCD2; the temporal lobe was involved in nine patients only. Notably, in extratemporal areas, mesial or paramedian locations were observed in nearly half of the patients, especially the frontal lobe. Moreover, the predominance of FCD2 locations near the midline was higher in patients negative/doubtful on MRI than in patients positive on MRI. These results are summaraized in Table 2.
The most challenging FCD2 to localize were small lesions located in regions difficult to analyse (i.e. the mesial part of the frontal lobe, insula). Misleading localizations mainly corresponded to mesial prefrontal regions, in which an anterior temporal hypometabolism may appear predominant. Other difficult locations were the precentral operculum and the supplementary motor area (SMA), in which a postcentral hypometabolism could also be misleading.
Interobserver agreement for the whole series was 79% in. This percentage varied considerably according to the grade of hypometabolism, ranging from 45% in patients with doubtful/subtle PET abnormalities to 82–95% in those with more obvious metabolic changes. This may account for the moderate kappa index (0.59, P < 0.0001).
Surgical data
SEEG was performed in all MRI-negative patients except one (96%) and in 67% of MRI-doubtful patients, but was less frequently performed in MRI-positive patients (28%). In MRI-negative/doubtful patients, preoperative PET findings were helpful for SEEG planning and cortical sampling, allowing the epileptogenic zone to be accurately localized. In each patient, the typical electrical signature of FCD2 [11] was observed within the site of maximal hypometabolism. In MRI-positive patients, SEEG was mostly performed in older patients (before 2006), whereas other patients were operated on directly on the basis of MRI and PET findings (including the three patients initially MRI-negative who changed to MRI-positive after comparison of the MRI and PET data). Thus, increasing experience with PET/MRI analysis allowed invasive monitoring to be avoided in some MRI-negative/doubtful patients (14%) and most MRI-positive patients. With a mean follow-up of 5.6 years (range 2–15 years), a favourable outcome (Engel’s class I) was achieved in 97 patients (94%) including 74 patients (72%) with an optimal outcome (class IA) and 40 who stopped antiepileptic drugs. This particularly high rate of successful procedures was observed in the whole population, including patients with the most challenging presentation (i.e. MRI-negative in functional areas) and patients operated on directly on the basis of PET/MRI comparison only. However, the MRI-negative/doubtful group achieved a significantly lower rate of class IA outcomes (60%) compared with the MRI-positive group (80%, P = 0.021). In addition, a dramatic decrease in the rate of class IA outcomes from 82% in MRI-positive/PET-positive patients to 40% in MRI-negative/PET-negative patients was observed. It should be added that most patients who underwent two operations belonged to the latter group. Logistic regression analysis indicated that MRI was associated with a higher odds ratio (OR 2.610, 95% confidence interval, CI, 1.018–6.694, P = 0.046) than PET (OR = 0.55, 95% CI 0.970–17.655, P = 0.055). These results are summaraized in Table 3.
Discussion
In this large surgical series, 18F-FDG PET was proven to have a high value for localizing FCD2 and contributed to excellent surgical outcomes in patients with severe drug-resistant focal epilepsy. This confirms the results of previous studies [12, 13] and those from our group focusing on MRI-negative patients [4]. Furthermore, it has allowed us to avoid invasive monitoring in an increasing number of patients, despite extratemporal locations and negative MRI findings in a great proportion of patients.
Optimizing the visual analysis of PET
The high sensitivity of PET for FCD2 localization was achieved by integration of electroclinical data and coregistration of PET and MRI data. In contrast, PET alone had a poor sensitivity (45%) accounting for its low contribution in extratemporal locations found in previous studies [14]. We highlight the impact of electroclinical data on the interpretation of PET in allowing a gain in sensitivity of 26%. Finally, coregistration with MRI data optimized the detection of FCD2 in 83% of patients, as previously demonstrated [4, 5, 15]. It is noteworthy that in three patients, MRI became positive only after comparison with PET data, and in five other patients positive PET/MRI registration was observed while both PET and MRI were negative/doubtful. These findings emphasize the role of coregistration, which improved the sensitivity of MRI and PET analysed independently. In addition, this type of analysis can be easily performed in clinical routine. Moreover, the increasing use of PET/MRI systems will also simplify the procedure [16].
FDG PET in MRI-negative FCD2
The already reported additional value of PET in MRI-negative/doubtful patients [4, 5, 15] was confirmed in this larger series, in which a high FCD2 localization rate (83%) was found in patients with this difficult presentation. This is worth noting because the detection of FCD2 by MRI remains a challenge despite the improvements in imaging techniques and postprocessing software [17,18,19,20,21,22,23]. In our series, MRI was doubtful/negative in 41% of patients, despite optimal technique and high level of experience of the radiologists. These data are concordant with the findings in other contemporary series in which the rates of MRI-negative FCD2 ranged from 21% to 42% [9, 19, 21, 24]. Besides the striking value of PET in MRI-negative/doubtful patients, its coregistration with MRI also helped delineate FCD2 in MRI-positive patients, allowing invasive monitoring to be avoided in most patients, even in functional areas. We also performed PET/MRI based surgical resections in an increasing number of MRI-negative/doubtful cases with favourable outcome. Finally, SEEG planning guided by PET findings permitted a more precise localization of the epileptogenic zone when invasive monitoring was indicated [25]. The value of PET in presurgical work-up has recently been investigated by other teams, showing an important contribution of PET to decision making for patient selection and surgical strategy, especially in those with difficult-to-localize epilepsy lesions and in MRI-negative patients [26, 27].
Surgical implications
It should be kept in mind that surgery for extratemporal MRI-negative epilepsy remains highly challenging with the lowest rate of successful procedures (37–47%) in previous series [28, 29]. Patients with MRI-negative FCD are also reported to have poor outcomes (32–46% of seizure-free patients) [30, 31]. In contrast, favourable outcomes have been obtained in 60–80% of patients with MRI-positive FCD [32,33,34] and in up to 90% of some selected patients [17, 35]. It has been clearly established that the detection and complete resection of FCD2 is the main factor predicting surgical outcome [6, 11, 17, 30, 33,34,35]. With outcomes in MRI-positive and MRI-negative patients similar to the best found in previously reported series, our results demonstrate the major contribution of PET to the localization of epilepsy lesions in these difficult-to-analyse regions. However, we stress that in patients with both negative/doubtful MRI and PET, the optimal outcome (Engel’s class IA) remains very difficult to achieve even when invasive monitoring is performed.
Limitations of the study
This was a retrospective study selecting all patients with histologically proven FCD2, but we could not assess the number of patients in whom an FCD2 was not detected by PET and who were therefore not referred for surgery. This may have increased the rate of false-negative results. In contrast, we found a low rate of false-positive results, since misleading findings in some regions (i.e. the frontotemporal junction, SMA and precentral operculum) could have been related to anatomofunctional connectivity and ictal spread [4]. These specific findings should be considered when analysing the metabolic abnormalities. The second important point relates to the PET analysis, which was deliberately limited to semiquantitative visual assessment. We are aware of the interest in automated quantitative methods in FCD2 detection, especially statistical parametric mapping (SPM) analysis. However, we aimed to assess the localizing value of PET in clinical routine, in which the quantification of metabolic changes requires complex and time-consuming methods. In addition, such methods involve comparison with a healthy subject database, which is rarely available in clinical practice. The different ways of overcoming this problem have come up against difficulties that limit their scope. In children, a cohort of pseudocontrols has been established, and has led to improvement in specificity but a lower sensitivity compared with adult control subjects [36]. Moreover, this database might optimally be used with a system comparable to that used for the examinations. The age of controls is also a limiting factor with databases of controls provided by manufacturers, which are often matched to patients studied for dementia rather than epilepsy [37]. A population of oncology patients without neurological history was tested in another study using high doses (5 MBq/kg) of 18F-FDG [38] and constituting a suboptimal control group.
Finally, using patients with cryptogenic temporal epilepsy (including hippocampal sclerosis) as controls [39] is problematic because it is typically in this location that the most severe and extensive metabolic abnormalities are found. It should be noted that, in these different studies, the value of techniques with quantification was assessed by comparison with visual analysis of PET scans alone and not with PET/MRI coregistration. In a previous study, we tested the respective value of visual versus SPM analysis using a cohort of healthy subjects as the reference population [4]. We found that visual analysis of coregistered PET and MRI data provided better results than SPM (91% versus 72% of positive localizations). The discrepancy was due to small FCD2 deeply located in the mesial aspect of the brain or at the bottom of a sulcus, where metabolism does not differ clearly from that of the white matter. However, we concluded that SPM analysis provided objective data supporting the visual analysis and that the two techniques are complementary. Similarly a previous study has shown the same sensitivity of visual and SPM PET analysis for the detection of FCD [13]. Moreover, in another study, visual re-assessment of PET data by experienced readers proved superior to SPM analysis, taking into account the above-mentioned methodological limitations [40]. Improvement in automated detection is indeed an important issue that will help the interpretation of PET scans. Nevertheless, comparison of automated quantified data with visual analysis is mandatory to avoid false interpretation.
The reader’s experience and the non-reproducibility of interpretations are often put forward as arguments against visual analysis. We obtained an interobserver agreement of 79% for the whole series, which unsurprisingly increased with the severity of the anomalies. The greatest variations were observed in subtle or doubtful hypometabolism and it is unlikely that automated analysis would have provided better results under these conditions. Moreover, considering the overrepresentation of small FCD2 at the bottom of the sulcus and in the mesial frontal regions, the additional value of automated analysis remains to be demonstrated.
Finally, a substantial proportion of patients (23%) had a PET scan performed while in a peri-ictal state due to the high seizure frequency characteristic of FCD2. We are well aware that an examination performed under these conditions is quite different from that performed during the interictal period as recommended, but frequent seizures are common in our patient population. We therefore carefully examined the potential effects of these conditions of examination and found a significant relationship between the grade of hypometabolism and time since last seizure, but this did not significantly influence the localization value of PET. However, if a peri-ictal PET scan provides doubtful results, performing a second examination, as was done in one patient in this series, should be discussed.
Conclusion
18F-FDG PET data coregistered with MRI data and integrated with electroclinical data appears particularly helpful in providing accurate localization of FCD2 in a high proportion of patients, and radically influences both the surgical indication and outcome in these patients with severe drug-resistant epilepsies. These benefits lead us to recommend the routine use of PET and systematic coregistration with MRI data in the presurgical work-up of patients with neocortical cryptogenic epilepsy.
Change history
28 April 2018
The original version of this article has added numbers in the text which are unnecessary. Correct line should be: “We also performed PET/MRI based surgical resections in an increasing number of MRI negative/ doubtful cases with favourable outcome.”
References
Blumcke I, Spreafico R, Haaker G, Coras R, Kobow K, Bien CG, et al. Histopathological findings in brain tissue obtained during epilepsy surgery. N Engl J Med. 2017;377:1648–56.
Ryvlin P, Cross JH, Rheims S. Epilepsy surgery in children and adults. Lancet Neurol. 2014;13:1114–26.
Guerrini R, Duchowny M, Jayakar P, Krsek P, Kahane P, Tassi L, et al. Diagnostic methods and treatment options for focal cortical dysplasia. Epilepsia. 2015;56:1669–86.
Chassoux F, Rodrigo S, Semah F, Beuvon F, Landré E, Devaux B, et al. FDG-PET improves surgical outcome in negative-MRI Taylor type focal cortical dysplasias. Neurology. 2010;75:2168–75.
Rubí S, Setoain X, Donaire A, Bargalló N, Sanmartí F, Carreño M, et al. Validation of FDG-PET/MRI coregistration in nonlesional refractory childhood epilepsy. Epilepsia. 2011;52:2216–24.
Chassoux F, Landre E, Mellerio C, Turak B, Mann MW, Daumas-Duport C, et al. Type II focal cortical dysplasia: electro-clinical phenotypes and surgical outcome related to imaging. Epilepsia. 2012;53:349–58.
Blümcke I, Thom M, Aronica E, Armstrong DD, Vinters HV, Palmini A, et al. The clinicopathologic spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia. 2011;52:158–74.
Engel J Jr, Van Ness PC, Rasmussen TB, Ojemann LM. Outcome with respect to epileptic seizures. In: Engel J Jr, editor. Surgical treatment of the epilepsies. 2nd ed. New York: Raven; 1993. p. 609–21.
Mellerio C, Labeyrie MA, Chassoux F, Daumas-Duport C, Landre E, Turak B, et al. Optimizing MR imaging detection of type 2 focal cortical dysplasia: best criteria for clinical practice. AJNR Am J Neuroradiol. 2012;33:1932–8.
Rivière D, Geffroy D, Denghien I, Souedet N, Cointepas Y. BrainVISA: an extensible software environment for sharing multimodal neuroimaging data and processing tools. In: Proceedings of the 15th Annual Meeting of the Organization for Human Brain Mapping, 18–23 June 2009, San Francisco, California. http://brainvisa.info.
Chassoux F, Devaux B, Landre E, Turak B, Nataf F, Varlet P, et al. Stereo-electroencephalography in focal cortical dysplasia: a 3D approach to delineating the dysplastic cortex. Brain. 2000;123:1733–51.
Lee SK, Choe G, Hong KS, Nam HW, Kim JY, Chung CK, et al. Neuroimaging findings of cortical dyslamination with cytomegaly. Epilepsia. 2001;42:850–6.
Kim YK, Lee DS, Lee SK, Chung CK, Chung JK, Lee MC. (18)F-FDG PET in localization of frontal lobe epilepsy: comparison of visual and SPM analysis. J Nucl Med. 2002;43:1167–74.
Knowlton RC, Elgavish RA, Bartolucci A, Ojha B, Limdi N, Blount J, et al. Functional imaging: II. Prediction of epilepsy surgery outcome. Ann Neurol. 2008;64:35–41.
Salamon N, Kung J, Shaw SJ, Koo J, Koh S, Wu JY, et al. FDG-PET/MRI coregistration improves detection of cortical dysplasia in patients with epilepsy. Neurology. 2008;71:1594–601.
Paldino MJ, Yang E, Jones JY, Mahmood N, Sher A, Zhang W. Comparison of the diagnostic accuracy of PET/MRI to PET/CT-acquired FDG brain exams for seizure focus detection: a prospective study. Pediatr Radiol. 2017;47:1500–7.
Urbach H, Scheffler B, Heinrichsmeier T, von Oertzen J, Kral T, Wellmer J, et al. Focal cortical dysplasia of Taylor's balloon cell type: a clinicopathological entity with characteristic neuroimaging and histopathological features, and favorable postsurgical outcome. Epilepsia. 2002;43:33–40.
Besson P, Andermann F, Dubeau F, Bernasconi A. Small focal cortical dysplasia lesions are located at the bottom of a deep sulcus. Brain. 2008;13:3246–55.
Wagner J, Weber B, Urbach H, Elger CE, Huppertz HJ. Morphometric MRI analysis improves detection of focal cortical dysplasia type II. Brain. 2011;134:2844–54.
Mellerio C, Labeyrie MA, Chassoux F, Roca P, Alami O, Plat M, et al. 3T MRI improves the detection of transmantle sign in type 2 focal cortical dysplasia. Epilepsia. 2014;55:117–22.
Hong SJ, Kim H, Schrader D, Bernasconi N, Bernhardt BC, Bernasconi A. Automated detection of cortical dysplasia type II in MRI-negative epilepsy. Neurology. 2014;83:48–55.
Mellerio C, Roca P, Chassoux F, Danière F, Cachia A, Lion S, et al. The power button sign: a newly described central sulcal pattern on surface rendering MR images of type 2 focal cortical dysplasia. Radiology. 2015;274:500–7.
Roca P, Mellerio C, Chassoux F, Rivière D, Cachia A, Charron S, et al. Sulcus-based MR analysis of focal cortical dysplasia located in the central region. PLoS One. 2015;10:e0122252.
Colombo N, Tassi L, Deleo F, Citterio A, Bramerio M, Mai R, et al. Focal cortical dysplasia type IIa and IIb: MRI aspects in 118 cases proven by histopathology. Neuroradiology. 2012;54:1065–77.
Chassoux F, Navarro V, Catenoix H, Valton L, Vignal JP. Planning and management of SEEG. Neurophysiol Clin. 2018;48:25–37.
Rathore C, Dickson JC, Teotónio R, Ell P, Duncan JS. The utility of 18F-fluorodeoxyglucose PET (FDG PET) in epilepsy surgery. Epilepsy Res. 2014;108:1306–14.
Rubinger L, Chan C, D'Arco F, Moineddin R, Muthaffar O, Rutka JT, et al. Change in presurgical diagnostic imaging evaluation affects subsequent pediatric epilepsy surgery outcome. Epilepsia. 2016;57:32–40.
Lee SK, Lee SY, Kim KK, Hong KS, Lee DS, Chung CK. Surgical outcome and prognostic factors of cryptogenic neocortical epilepsy. Ann Neurol. 2005;58:525–32.
Chapman K, Wyllie E, Najm I, Ruggieri P, Bingaman W, Lüders J, et al. Seizure outcome after epilepsy surgery in patients with normal preoperative MRI. J Neurol Neurosurg Psychiatry. 2005;76:710–3.
Krsek P, Maton B, Jayakar P, Dean P, Korman B, Rey G, et al. Incomplete resection of focal cortical dysplasia is the main predictor of poor postsurgical outcome. Neurology. 2009;72:217–23.
Widdess-Walsh P, Jeha L, Nair D, Kotagal P, Bingaman W, Najm I. Subdural electrode analysis in focal cortical dysplasia: predictors of surgical outcome. Neurology. 2007;69:660–7.
Tassi L, Colombo N, Garbelli R, Francione S, Lo Russo G, Mai R, et al. Focal cortical dysplasia: neuropathological subtypes, EEG, neuroimaging and surgical outcome. Brain. 2002;125:1719–32.
Fauser S, Schulze-Bonhage A, Honegger J, Carmona H, Huppertz HJ, Pantazis G, et al. Focal cortical dysplasias: surgical outcome in 67 patients in relation to histological subtypes and dual pathology. Brain. 2004;127:2406–18.
Kim DW, Lee SK, Chu K, Park KI, Lee SY, Lee CH, et al. Predictors of surgical outcome and pathologic considerations in focal cortical dysplasia. Neurology. 2009;72:211–6.
Harvey AS, Mandelstam SA, Maixner WJ, Leventer RJ, Semmelroch M, MacGregor D, et al. The surgically remediable syndrome of epilepsy associated with bottom-of-sulcus dysplasia. Neurology. 2015;84:2021–8.
Archambaud F, Bouilleret V, Hertz-Pannier L, Chaumet-Riffaud P, Rodrigo S, Dulac O, et al. Optimizing statistical parametric mapping analysis of 18F-FDG PET in children. EJNMMI Res. 2013;3:2.
Mendes Coelho VC, Morita ME, Amorim BJ, Ramos CD, Yasuda CL, Tedeschi H, et al. Automated online quantification method for 18F-FDG positron emission tomography/CT improves detection of the epileptogenic zone in patients with pharmacoresistant epilepsy. Front Neurol. 2017;8:453.
Mayoral M, Marti-Fuster B, Carreño M, Carrasco JL, Bargalló N, Donaire A, et al. Seizure-onset zone localization by statistical parametric mapping in visually normal (18)F-FDG-PET studies. Epilepsia. 2016;57:1236–44.
Tan YL, Kim H, Lee S, Tihan T, Ver Hoef L, Mueller SG, et al. Quantitative surface analysis of combined MRI and PET enhances detection of focal cortical dysplasias. Neuroimage. 2018;166:10–8.
van't Klooster MA, Huiskamp G, Zijlmans M, Debets RM, Comans EF, Bouvard S, et al. Can we increase the yield of FDG-PET in the preoperative work-up for epilepsy surgery? Epilepsy Res. 2014;108:1095–105.
Acknowledgments
The authors thank the team of SHFJ, Patrick Bodilis, Christine Baron, Brigitte Jouve, Vincent Brulon, Philippe Gervais and Thierry Le Kieffre, for performing the PET scans.
Author information
Authors and Affiliations
Contributions
All authors were involved in drafting and revising the article.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
The original version of this article was revised: There were added numbers in the text which are unnecessary. Correct line should be: “We also performed PET/MRI based surgical resections in an increasing number of MRI negative/ doubtful cases with favourable outcome.”
Rights and permissions
About this article
Cite this article
Desarnaud, S., Mellerio, C., Semah, F. et al. 18F-FDG PET in drug-resistant epilepsy due to focal cortical dysplasia type 2: additional value of electroclinical data and coregistration with MRI. Eur J Nucl Med Mol Imaging 45, 1449–1460 (2018). https://doi.org/10.1007/s00259-018-3994-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-3994-3