Abstract
Purpose
In patients with newly diagnosed head and neck squamous cell carcinoma (HNSCC), we wanted to examine the differences in overall treatment decisions, i.e. curative versus palliative treatment intent, reached by a multidisciplinary team conference (MDTC) based on 18F–fluoro-deoxy-glucose-positron emission tomography/computed tomography (PET/CT) or chest X-ray + MRI of the head and neck (CXR/MRI).
Patients and methods
This was a prospective blinded cohort study based on paired data. Consecutive patients with histologically verified primary HNSCC were invited to participate. All included patients underwent CXR/MRI and PET/CT before diagnostic biopsy. An ordinary MDTC using all available imaging was conducted as per standard practice. After at least 3 months (to eliminate recall bias in the team), the first project MDTC was conducted, based on either CXR/MRI or PET/CT, and the tumor board drew conclusions regarding treatment. After an additional 3 months, a second project MDTC was conducted using the complementary imaging modality.
Results
A total of 307 patients were included. Based on CXR/MRI, 303 patients (99%) were recommended for curative treatment and only four patients (1%) for palliative treatment. Based on PET/CT, the MDTC concluded that 278 (91%) patients were suitable for curative treatment and 29 (9%) patients for palliative treatment. The absolute difference of 8% was statistically significant (95% CI: 4.8%–11.5%, p < 0.001).
Conclusions
A PET/CT-based imaging strategy significantly changed the decisions regarding treatment intent made by a MDTC for patients diagnosed with HNSCC, when compared with the standard imaging strategy of CXR/MRI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
18F–fluoro-deoxy-glucose-positron emission tomography/computed tomography scan (PET/CT) has shown promising results for diagnosis and staging of head and neck squamous cell carcinoma (HNSCC) when compared with standard imaging modalities, i.e. magnetic resonance imaging of the head and neck including chest X-ray (CXR/MRI) [1,2,3,4]. In addition to its possible superiority in detecting distant metastasis, PET/CT may also improve detection of synchronous cancers [5,6,7,8,9,10]. Still, the European guidelines from the European Head & Neck Society and the European Society for Medical Oncology recommend a standard clinical imaging strategy with CXR/MRI for evaluating patients with primary HNSCC, and consideration of chest computed tomography to rule out distant metastasis and synchronous cancer. PET/CT is only recommended for evaluating patients with malignant cervical adenopathy from an unknown primary tumor [11]. Appropriate diagnostic imaging allows better decision making with respect to the optimal treatment strategy, including treatment intent (i.e. curative versus palliation), subsequent detailed tumor description for optimal choice of treatment modality (surgery, radiotherapy, chemotherapy), and “intra-modality” planning (definitive planning) such as radiation treatment volumes, extent of surgical resection and neck dissection.Studies have demonstrated that the use of PET/CT modifies the treatment approach in 14–31% of head and neck cancer patients [2, 4, 12,13,14,15,16,17,18,19,20,21]. However, most of these studies were based on PET alone, not PET/CT. Furthermore, the additive impact of PET or PET/CT to CXR/MRI was investigated, but a head-to-head comparison of PET/CT versus CXR/MRI was not performed. Lastly, the main consideration in patient management, namely treatment intent, was not the primary objective. From a patient’s point of view, treatment intent remains the most important factor. Appropriate patient treatment is also a central element in ensuring cost-effective use of health care resources. The objectives of the current study were to examine the overall treatment conclusion, i.e. curative versus palliative treatment intent, reached by the multidisciplinary team conference (MDTC) based on either an imaging strategy with PET/CT or CXR/MRI of patients diagnosed with HNSCC.
Methods
A prospective, blinded cohort study based on paired data was performed according to the “Strengthening the Reporting of OBservational studies in Epidemiology” (STROBE) statement [22].
Setting and participants
The study design, setting, and methods have been described previously [23]. Consecutive patients referred to the Head and Neck Cancer Center, Odense University Hospital, from 1st September 2013 to 29th February 2016 for suspected HNSCC, were invited to participate in the study. Exclusion criteria were allergy or intolerance to iodine contrast medium, treatment with high doses of systemic steroids (>50 mg/day), reduced kidney function (defined as increased S-creatinine or diagnosed kidney disease) or considered unable to cooperate.Patients who accepted participation underwent CXR/MRI and PET/CT on the same day and prior to biopsy, i.e. upfront, to improve the quality of staging and diagnostic interpretation. Acquiring imaging before biopsy is the standard procedure in the Danish head and neck cancer fast-track program. The final study population comprised patients with histologically verified HNSCC, and their data were used for detailed analysis to compare the overall treatment conclusion reached by the MDTC based on either PET/CT or CXR/MRI.
The multidisciplinary team conference
MDTC was a collaborative effort among the Departments of ORL (Head & Neck Surgery), Plastic Surgery, Oncology, Nuclear Medicine, and Radiology, who were all represented by experienced specialists participating in MDTC conferences as part of their daily clinical practice. Pathologists and neurosurgeons were available, but did not routinely participate in the MDTC.
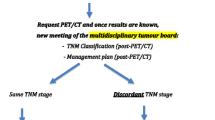
All patients participated in an ordinary MDTC that included all available imaging, to ensure that patients had full benefit of the examinations performed as part of their primary workup for HNSCC and subsequent treatment (Fig. 1). As part of the study, a project MDTC based on CXR/MRI or PET/CT was undertaken after at least three months (100–120 days). The delay was introduced to eliminate recall bias in the tumor board of evaluators. After at least three more months (100–120 days), a second project MDTC was carried out with access to the complementary imaging modality only. All patients were thus evaluated twice in a blinded standard setup, in which the only difference was the available imaging modality and the corresponding imaging team.
The PET/CT imaging team included nuclear medicine specialists and radiologists, while the CXR/MRI team consisted of radiologists only. All experienced chief physicians. The individual imaging team member was allocated to only one team, and no overlap or interchange between teams was allowed. Project MDTC sessions were held once a week and included approximately 15 patients each time. A representative from the PET/CT team joined the MDTC every other week, and equivalently, one from the CXR/MRI team the other week. At each project session, the pre-diagnostic patient history was briefly presented by the author MR (who was not a member of the tumor board), and the patient’s scans were evaluated and discussed. All imaging studies were evaluated by the tumor board, and registration forms comprising variables about treatment strategy, intent, and modality were completed and filed in separate, sealed envelopes.
Imaging techniques
PET/CT data were acquired on a hybrid PET/CT scanner (GE Discovery 690, 710, VCT, or RX). After a fasting period of at least 4 h, 4 MBq/kg of 18F–FDG was injected intravenously. The PET scan was performed using a standard whole-body acquisition protocol extending from the vertex to the thigh and an acquisition time of 2½ min per bed position. The head was fixed to prevent movement. PET data were reconstructed into transaxial slices with a matrix size of 128 × 128 (pixel size 5.47 mm) or 256 × 256 (pixel size 2.73 mm), depending on the scanner type. Images from all four PET/CT systems had a slice thickness of 3.27 mm, and reconstruction was done by iterative 3D OS-EM.
Multislice, diagnostic quality CT scan with intravenous contrast medium (Ultravist® 370 mg/mL) was acquired after the PET scan. The CT scan was obtained with continuous shallow breathing. Data were reconstructed with a standard filter into transaxial slices with a field of view of 50 cm, matrix size of 512 × 512 (pixel size 0.98 mm), and a slice thickness of 3.75 mm. The scan field of view was 70 cm for both PET and CT scans. Analysis of PET/CT was done on a GE Advantage Workstation v. 4.4 or 4.3 or GE AW Server v 3.1 or 3.2. MRI was performed on Philips Achieva, Achieva dStream or Ingenia 1.5 T (Philips Medical Systems, Best, Netherlands) hardware using 20 channel (dStream) head-neck coil. The exam protocol was kept unchanged for the duration of the study and consisted of STIR, TSE-T2 and -T1 with and without contrast enhancement, in axial or coronal planes with coverage from skull base to aortic arch using 5 mm slices. Diffusion weighted imaging with spectral fat saturation and apparent diffusion coefficient-maps derived from b-values 0 and 1000 mm2/s were done in axial 6 mm slices. Images were read on a GE Centricity RA1000 PACS workstation. The acquisition parameters of the MRI sequences are displayed in Supplemental Table 1.
CXR was performed to departmental standards in full inspiration anteroposterior and lateral projections with 130–145 kV and automatic exposure control. FD-X hardware systems (Siemens Healthineers, Erlangen, Germany) were used, and studies were read using GE Centricity RA1000 PACS workstation with dual 3MP medical grade monitors.
Image interpretation
Interpretation of primary tumors was based on anatomic pattern recognition, including morphologic changes, altered signal intensity, contrast enhancement, and changes in diffusivity, and metabolic information on FDG avidity for PET. Malignant lesions were suspected when deemed more probable than benign lesions.
Characteristics considered for lymph nodes were enlargement, shape (round or not), hilum (fatty/non-fatty), necrosis, center (dense or not), topography of node distribution, and FDG avidity for PET. A fixed threshold of standard uptake value was not used to determine whether a lesion was malignant or not.
Lung lesions were considered distant metastases if one or more FDG avid nodules were present on PET and CT, respectively. Small subpleural nodules (especially when calcified) were not considered metastases on CT unless multiple were present, or FDG-avid on PET. Distant metastases were suspected on CXR, when opacification was not consistent with infectious pattern. Lung lesions in the field of view of the MRI was considered suspicious, when the configuration was nodulary and/or spiculary and not consistent with infectious pattern.
For PET, bone lesions were regarded metastases, when FDG-avid osteolytic (or osteosclerotic) lesions were present. Significantly increased FDG uptake in the bone marrow even without the lytic or sclerotic changes were also regarded metastases. Lesions close to the joints were rarely considered metastases. Regarding MRI, focal signal changes on T2, STIR and presence of enhancement was observed, but as these may vary, only lesions appearing with low signal of T1 were considered suspicious for metastasis.
For PET, liver metastases and malignant pleural effusion were suspected only in lesions with significantly increased FDG uptake as compared to the surroundings. Muscle metastases were suspected in patients with randomly distributed focal areas of increased FDG uptake in the muscles and corresponding morphological changes. Longitudinal muscular FDG uptake was considered to be physiological.
Synchronous cancers were suspected if tumors were present in organs, atypical of nesting metastases. Other parameters were also weighted, for instance the size and the FDG intensity (i.e. for PET) of the primary compared to the suspected synchronous tumor. Likewise, the pattern of spread and possible gaps between lymph node stations were taken into consideration. Regarding lung lesions, the presence of spicules and hilar lymph nodes by CT, helped determine whether representing a metastasis or a synchronous cancer.
Outcomes
The primary endpoint was change of treatment intent (i.e. curative versus palliative) decided by the tumor board, based on either PET/CT or CXR/MRI. All-cause mortality was considered as event for the net reclassification improvement (NRI) (see Statistics section). Mortality was assessed through linkage to the Danish Cause of Death register at least 6 months (August 31, 2016) after termination of inclusion.
Statistics
Continuous variables are presented as means and standard deviations (normally distributed variables) or medians and ranges. Categorical variables are presented as counts and corresponding percentages.
We made a head-to-head comparison of MDTC decisions on patients assigned to curative or palliative treatment based on either PET/CT or CXR/MRI, using 2 × 2 tables and McNemar’s test. The sample size was based on the assumptions that (a) 7% of patients are assigned to curative treatment according to SCI, but to palliative treatment based on PET/CT and (b) 2% of patients are assigned to curative treatment by PET/CT, but palliative treatment by CXR/MRI. Then, with a type I error probability of 5% and a power of 80%, 281 patients were sufficient to indicate a statistically significant difference. Assuming a drop-out rate of 10%, 312 patients were to be included.
Moreover, the ability of PET/CT to improve the MDTC decision regarding treatment intent, in terms of survival, was tested using NRI [24, 25]. NRI quantifies the improvement in risk prediction offered by a new model (as compared to an older one) by assessing the ability of the new model to reclassify subjects (i.e., into a higher or lower risk category) either appropriately or inappropriately. NRI is a somewhat novel statistical method of risk prediction that has attracted extensive interest in recent years. C-statistics, such as area under the curve (AUC), have been the standard metric for quantifying improvements for several decades, but can lack clinical relevance and be difficult to interpret, particularly in the case of small magnitude changes [26]. Two-sided P-values below 0.05 were considered statistically significant.
All analyses were performed with Stata/IC 14 (StataCorp LP, College Station, TX, USA).
Ethics and disclosures
The study was conducted in accordance with good clinical practice and the Declaration of Helsinki. Permission was granted from the local ethics committee (Project ID: S_20120217), and informed consent was obtained from all included patients. The project was implemented without the involvement of private organizations or companies.
Results
Of 1109 patients referred to our institution during the study period, 307 were histologically verified with primary HNSCC and participated in the study, i.e. 227 (74%) men and 80 (26%) women with a median age of 64 years (range 22–89) (Table 1). A flowchart of patient inclusion is shown in Fig. 2. The most frequent primary tumor site was the oral cavity (48%) followed by pharynx (34%) and larynx (18%). The median follow-up time was 461 days (range 21 to 1092 days, interquartile range 271 days–722 days). Localization of verified distant metastasis and the synchronous cancers found in the 307 HNSCC patients is listed in Supplemental Tables 2 and 3. Furthermore, Supplemental Table 4 displays the applied reference standard for verification of distant metastasis and synchronous cancers.
MDTC decisions
Based on CXR/MRI, the MDTC concluded that 303 (99%) patients were suitable for curative treatment, and only four (1%) patients should have palliative treatment. Based on PET/CT, the MDTC concluded that 278 (91%) patients should be treated with curative intent, and 29 (9%) patients should receive palliative treatment (Tables 2 and 3). The absolute difference in treatment intent of 8% was statistically significant (95% CI: 4.8% – 11.5%, p < 0.001).
Reclassification
NRI analysis showed that PET/CT significantly improved the ability to determine the appropriate treatment intent compared to CXR/MRI (NRI = 24.1%, 95% CI: 13.7% to 34.5%, p < 0.001).
This net reclassification was derived from 17/62 (27.4%) patients in the event group who, based on PET/CT, were correctly reclassified from curative to palliative treatment, and 8/245 (3.3%) patients in the non-event group who were apparently incorrectly reclassified to palliative treatment (Table 4).
The factual MDTC decision (based on the full set of imaging for each patient) for the 17 patients who were correctly reclassified by PET/CT was accessed through review of the patient journals. This showed that in only 9/17 cases, the palliative treatment intent, based on PET/CT alone, was delivered.
Discussion
Our results demonstrated that a clinical imaging strategy based on PET/CT significantly changed the overall MDTC decision regarding treatment intent when compared with a strategy with CXR/MRI (p < 0.001) and that these changes, reflecting survival prognosis, were associated with a significant reclassification of patients to palliative treatment (NRI = 24.1%, p < 0.001). PET/CT thus resulted in more appropriate decision-making and ensured that more patients instantly received relevant management in terms of overall treatment intent, and type and extent of therapeutic intervention.
The impact of PET/CT on MDTC treatment decisions is most likely explained by its improved staging accuracy [1, 2, 7] and in particular due to better detection of distant metastasis, which in most cases leads to a palliative treatment strategy. To our knowledge, this is the largest prospective study to assess the impact of PET/CT on patient management in the diagnostic evaluation of patients with HNSCC. Our study design comparing MDTC conclusions based on separate imaging modalities allowed us to analyze the relative contribution of each modality to treatment planning. Whether PET/CT leads to an overall benefit that is clinically significant is a complicated discussion. However, it is remarkable that almost half of the patients in the subgroup, who died and were reclassified from curative to palliative treatment, actually received curatively intended treatment, strengthening the argument for PET/CT as an effective identifier of high risk patients who do not benefit from aggressive curative treatment. Whether those who were apparently incorrectly reclassified from curative to palliative treatment, were truly incorrectly reclassified is also challenging to assess, as the reclassification is strongly correlated with follow-up duration. Under most circumstances, prolonging the follow-up duration would tend to increase the NRI as more patients classified as having advanced disease would have then died. Similarly, if follow-up was shortened enough, the NRI for PET/CT might even become negative as patients assigned to a higher risk category would seemingly have been incorrectly classified, since none of them would have died.
The additive effect of PET/CT to CXR/MRI has not been examined head-to-head before. Previous studies have investigated the influence of PET/CT on management decisions [2, 12,13,14,15,16,17,18,19,20, 27], but various methodological issues arise such as study design (some were retrospective studies), use of different imaging technologies (i.e. PET alone vs. PET/CT), variable use of blinding, and differing reference standards. In addition, these studies often had significant time delays between the imaging modalities being compared.However, recent well-conducted studies performed by Ryu et al. [21] and Cacicedo et al. [4] show results that are more comparable to ours. Both studies investigated the addition of PET/CT (after histopathology) to standard clinical imaging. The studies reported that PET/CT altered patient management with high impact (i.e. change in treatment intent and/or treatment modality) in 4.8% and 16.6% of the patients, respectively. Still, no direct comparison with standard imaging was performed.Our results demonstrate that a PET/CT-based imaging strategy may contribute to a more individualized patient treatment, when compared with the standard strategy recommended by the contemporary European clinical practice guidelines [11]. Knowledge about extent of disease and the related prognosis is valuable to patients with metastatic HNSCC, and PET/CT can also inform decisions about treatment modality and intensity for patients receiving radical treatment. We suggest that clinicians and policy-makers consider to include PET/CT much earlier in the work-up of HNSCC patients, not only because this ensures better treatment triage, but also because PET/CT has been demonstrated to be cost-effective in a number of cancers [28]. PET/CT seems better suited to sustain treatment intent than CXR/MRI. It has the potential to become the single imaging modality in patients with HNSCC, although further head-to-head comparisons of PET/CT with CXR/MRI are needed first.
Methodological considerations
The strengths of our study include its prospective design, consecutive data collection in patients over a 2.5-year period where each patient acted as their own control with respect to imaging modality, the absence of delay between PET/CT and CXR/MRI (both performed on the same day), the state-of-the-art technology used for all imaging studies, and that all scans were read by experienced experts.The strengths and validity of paired diagnostic studies versus randomized (controlled) studies have been well described [29,30,31,32]. In a paired data design, the risk of confounding is eliminated along with the derived need for stratification analysis. Other advantages of a paired design involve the dependence of the sample size on the agreement rate between the modalities, multiple aims of diagnostic accuracy studies, and the possibility of early unblinding of results at the individual level. For this reason, we deliberately chose a paired data design rather than a randomized one.
Limitations of our study were that it was performed at a single institution, which restricts the generalizability of the results, and that our study population was overrepresented by patients with oral cavity cancer. This occurred because patients suspected of oral cavity cancers were referred to us from the entire Region of Southern Denmark, whereas laryngeal and pharyngeal cancer patients were referred only from the region of Funen, which accounts for a little less than half of the region’s population.
Comparing PET/CT, a whole-body scan, with regional radiologic imaging modalities, may also seem unfair. However, the aim of this study was to compare with the contemporary European clinical imaging strategy, which is employed in most head and neck cancer centers.
For all patients included in this study, the factual treatment was decided based on the full set of imaging. Hypothetically, if the 17 patients who were apparently correctly reclassified from curative to palliative treatment by PET/CT did not have advanced disease (i.e., false positive), and incorrectly received palliative treatment, they might have died of progression due to improper treatment, rendering the reclassification correct (self-fulfilling).
Lastly, disease-specific mortality would have been preferable as the clinical endpoint rather than all-cause mortality, but these data were not available. However, given the relatively short follow-up, we would expect the cause of death for most of these patients to be cancer-specific. Thus, it is not very likely that the use of cancer-specific mortality would have changed our results to a significant extent.
Conclusions
A PET/CT-based imaging strategy significantly changed the decisions regarding treatment intent made by a MDTC for patients diagnosed with HNSCC, when compared with the standard imaging strategy in current European clinical guidelines. Furthermore, the conference decisions based on PET/CT improved the allocation of patients to palliative treatment in terms of expected patient survival.
References
Rohde M, Dyrvig AK, Johansen J, Sorensen JA, Gerke O, Nielsen AL, et al. 18F–fluoro-deoxy-glucose-positron emission tomography/computed tomography in diagnosis of head and neck squamous cell carcinoma: a systematic review and meta-analysis. Europe J Cancer (Oxford, England : 1990). 2014;50:2271–9. https://doi.org/10.1016/j.ejca.2014.05.015.
Lonneux M, Hamoir M, Reychler H, Maingon P, Duvillard C, Calais G, et al. Positron emission tomography with [18F]fluorodeoxyglucose improves staging and patient management in patients with head and neck squamous cell carcinoma: a multicenter prospective study. J Clin Oncol : Off J Am Soc Clin Oncol. 2010;28:1190–5. https://doi.org/10.1200/jco.2009.24.6298.
Yoo J, Henderson S, Walker-Dilks C. Evidence-based guideline recommendations on the use of positron emission tomography imaging in head and neck cancer. Clin Oncol (Royal College of Radiologists (Great Britain)). 2013;25:e33–66. https://doi.org/10.1016/j.clon.2012.08.007.
Cacicedo J, Fernandez I, Del Hoyo O, Dolado A, Gomez-Suarez J, Hortelano E, et al. Should PET/CT be implemented in the routine imaging work-up of locally advanced head and neck squamous cell carcinoma? A prospective analysis. Eur J Nucl Med Mol Imaging. 2015;42:1378–89. https://doi.org/10.1007/s00259-015-3071-0.
Senft A, de Bree R, Hoekstra OS, Kuik DJ, Golding RP, Oyen WJ, et al. Screening for distant metastases in head and neck cancer patients by chest CT or whole body FDG-PET: a prospective multicenter trial. Radiother Oncol. 2008;87:221–9. https://doi.org/10.1016/j.radonc.2008.03.008.
Haerle SK, Schmid DT, Ahmad N, Hany TF, Stoeckli SJ. The value of (18)F-FDG PET/CT for the detection of distant metastases in high-risk patients with head and neck squamous cell carcinoma. Oral Oncol. 2011;47:653–9. https://doi.org/10.1016/j.oraloncology.2011.05.011.
Xu GZ, Guan DJ, He ZY. (18)FDG-PET/CT for detecting distant metastases and second primary cancers in patients with head and neck cancer. A meta-analysis. Oral Oncol. 2011;47:560–5. https://doi.org/10.1016/j.oraloncology.2011.04.021.
Johansen J, Petersen H, Godballe C, Loft A, Grau C. FDG-PET/CT for detection of the unknown primary head and neck tumor. Quarter J Nucl Med Molec Imaging. 2011;55:500–8.
Krabbe CA, Pruim J, van der Laan BF, Rodiger LA, Roodenburg JL. FDG-PET and detection of distant metastases and simultaneous tumors in head and neck squamous cell carcinoma: a comparison with chest radiography and chest CT. Oral Oncol. 2009;45:234–40. https://doi.org/10.1016/j.oraloncology.2008.05.024.
Kim SY, Roh JL, Yeo NK, Kim JS, Lee JH, Choi SH, et al. Combined 18F-fluorodeoxyglucose-positron emission tomography and computed tomography as a primary screening method for detecting second primary cancers and distant metastases in patients with head and neck cancer. Ann Oncol. 2007;18:1698–703. https://doi.org/10.1093/annonc/mdm270.
Gregoire V, Lefebvre JL, Licitra L, Felip E. Squamous cell carcinoma of the head and neck: EHNS-ESMO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21:v184–v6.
Scott AM, Gunawardana DH, Bartholomeusz D, Ramshaw JE, Lin P. PET changes management and improves prognostic stratification in patients with head and neck cancer: results of a multicenter prospective study. J Nuclear Med : Off Publ, Soc Nucl Med. 2008;49:1593–600. https://doi.org/10.2967/jnumed.108.053660.
Arias F, Chicata V, Garcia-Velloso MJ, Asin G, Uzcanga M, Eito C, et al. Impact of initial FDG PET/CT in the management plan of patients with locally advanced head and neck cancer. Clin Translat Oncol : Off Publ Fed Spanish Oncol Soc National Cancer Instit Mexico. 2015;17:139–44. https://doi.org/10.1007/s12094-014-1204-8.
Abramyuk A, Appold S, Zophel K, Baumann M, Abolmaali N. Modification of staging and treatment of head and neck cancer by FDG-PET/CT prior to radiotherapy. Strahlentherapie und Onkologie : Organ der Deutschen Rontgengesellschaft [et al]. 2013;189:197–201. https://doi.org/10.1007/s00066-012-0283-0.
Prestwich RJ, Bhatnagar P, Chowdhury FU, Patel CN, Dyker KE, Coyle C, et al. The impact of (18)F-FDG PET CT prior to Chemoradiotherapy for stage III/IV head and neck Squamous cell carcinoma. ISRN Oncol. 2012;2012:636379. https://doi.org/10.5402/2012/636379.
Paidpally V, Tahari AK, Lam S, Alluri K, Marur S, Koch W, et al. Addition of 18F–FDG PET/CT to Clinical Assessment Predicts Overall Survival in HNSCC: A Retrospective Analysis with Follow-up for 12 Years. J Nucl Med : Off Publ, Soc Nucl Med. 2013; https://doi.org/10.2967/jnumed.113.121285.
Fleming AJ Jr, Smith SP Jr, Paul CM, Hall NC, Daly BT, Agrawal A, et al. Impact of [18F]-2-fluorodeoxyglucose-positron emission tomography/computed tomography on previously untreated head and neck cancer patients. Laryngoscope. 2007;117:1173–9. https://doi.org/10.1097/MLG.0b013e31805d017b.
Connell CA, Corry J, Milner AD, Hogg A, Hicks RJ, Rischin D, et al. Clinical impact of, and prognostic stratification by, F-18 FDG PET/CT in head and neck mucosal squamous cell carcinoma. Head Neck. 2007;29:986–95. https://doi.org/10.1002/hed.20629.
Zanation AM, Sutton DK, Couch ME, Weissler MC, Shockley WW, Shores CG. Use, accuracy, and implications for patient management of [18F]-2-fluorodeoxyglucose-positron emission/computerized tomography for head and neck tumors. Laryngoscope. 2005;115:1186–90.
Ha PK, Hdeib A, Goldenberg D, Jacene H, Patel P, Koch W, et al. The role of positron emission tomography and computed tomography fusion in the management of early-stage and advanced-stage primary head and neck squamous cell carcinoma. Arch Otolaryngol0--Head Neck Surg. 2006;132:12–6. https://doi.org/10.1001/archotol.132.1.12.
Ryu IS, Roh JL, Kim JS, Lee JH, Cho KJ, Choi SH, et al. Impact of (18)F-FDG PET/CT staging on management and prognostic stratification in head and neck squamous cell carcinoma: A prospective observational study. Europe J Cancer (Oxford, England : 1990). 2016;63:88–96. https://doi.org/10.1016/j.ejca.2016.05.002.
Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg (London, England). 2014;12:1500–24. https://doi.org/10.1016/j.ijsu.2014.07.014.
Rohde M, Nielsen AL, Johansen J, Sorensen JA, Diaz A, Asmussen JT, et al. Head-to-head comparison of chest x-ray/head and neck MRI, chest CT/head and neck MRI, and 18F–FDG-PET/CT for detection of distant metastases and synchronous cancer in oral, pharyngeal, and laryngeal Cancer. J Nucl Med : Off Publ, Soc Nuclear Med. 2017; https://doi.org/10.2967/jnumed.117.189704.
Greenland P. Comments on 'Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond' by M. J. Pencina, R. B. D'Agostino Sr, R. B. D'Agostino Jr, R. S. Vasan, statistics in medicine (DOI: 10.1002/sim.2929). Stat Med. 2008;27:188–90. https://doi.org/10.1002/sim.2976.
Pencina MJ, D'Agostino RB Sr, D'Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–172; discussion 207-12. https://doi.org/10.1002/sim.2929.
Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation. 2007;115:928–35. https://doi.org/10.1161/circulationaha.106.672402.
Gordin A, Golz A, Keidar Z, Daitzchman M, Bar-Shalom R, Israel O. The role of FDG-PET/CT imaging in head and neck malignant conditions: impact on diagnostic accuracy and patient care. Otolaryngol--Head Neck Surg : Off J Am Acad Otolaryngol-Head Neck Surg. 2007;137:130–7. https://doi.org/10.1016/j.otohns.2007.02.001.
Gerke O, Hermansson R, Hess S, Schifter S, Vach W, Hoilund-Carlsen PF. Cost-effectiveness of PET and PET/computed tomography: a systematic review. PET Clin. 2015;10:105–24. https://doi.org/10.1016/j.cpet.2014.09.008.
Gerke O, Hoilund-Carlsen PF, Poulsen MH, Vach W. Interim analyses in diagnostic versus treatment studies: differences and similarities. Am J Nucl Med Mol Imaging. 2012;2:344–52.
Siepe B, Hoilund-Carlsen PF, Gerke O, Weber WA, Motschall E, Vach W. The move from accuracy studies to randomized trials in PET: current status and future directions. J Nucl Med : Off Publ, Soc Nucl Med. 2014;55:1228–34. https://doi.org/10.2967/jnumed.113.127076.
Vach W, Hoilund-Carlsen PF, Gerke O, Weber WA. Generating evidence for clinical benefit of PET/CT in diagnosing cancer patients. J Nucl Med : Off Publ, Soc Nucl Med. 2011;52(Suppl 2):77S–85S. https://doi.org/10.2967/jnumed.110.085704.
Gerke O, Hoilund-Carlsen PF, Vach W. Analyzing paired diagnostic studies by estimating the expected benefit. Biom J. 2015;57:395–409. https://doi.org/10.1002/bimj.201400020.
Acknowledgements
This study was financially supported by the University of Southern Denmark, the Danish Cancer Society, and the Region of Southern Denmark.
Funding
We are grateful for the doctoral research grants given by the University of Southern Denmark, the Danish Cancer Society and the Region of Southern Denmark.
Author information
Authors and Affiliations
Contributions
Conception and design: Max Rohde, Poul Flemming Høilund-Carlsen, Christian Godballe.
Administrative support: Anne L. Nielsen.
Provision of study materials or patients: Max Rohde, Christian Godballe.
Collection and assembly of data: Max Rohde, Jørgen Johansen, Jens A. Sørensen Anne L. Nielsen, Jon T. Asmussen, Anabel Diaz, Anders Thomassen, Niels Gyldenkerne, Helle Døssing, Kristine Bjrøndal, Christian Godballe.
Data analysis and interpretation: Max Rohde, Jørgen Johansen, Jens A. Sørensen, Oke Gerke, Poul Flemming Høilund-Carlsen, Christian Godballe.
Manuscript writing: All authors.
Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Conflict of interest statement
We declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Rohde, M., Nielsen, A.L., Johansen, J. et al. Up-front PET/CT changes treatment intent in patients with head and neck squamous cell carcinoma. Eur J Nucl Med Mol Imaging 45, 613–621 (2018). https://doi.org/10.1007/s00259-017-3873-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3873-3