Abstract
Purpose
The aim of this study was to assess the value of dual-time point imaging in PET/CT for detection of biochemically recurrent or persistent prostate cancer, using the prostate-specific membrane antigen (PSMA) ligand [68Ga]PSMA I&T.
Methods
240 patients who underwent a [68Ga]PSMA I&T PET/CT in the context of biochemical relapse of prostate cancer were included in this retrospective analysis. Imaging consisted of a standard whole-body PET/CT (1 h p.i.), followed by delayed (3 h p.i.) imaging of the abdomen. PSA-stratified proportions of positive PET/CT results, standardized uptake values and target-to-background ratios were analyzed, and compared between standard and delayed imaging.
Results
The overall detection rates of [68Ga]PSMA I&T PET/CT were 94.2, 71.8, 58.6, 55.9 and 38.9% for PSA levels of ≥2, 1 to <2, 0.5 to <1, >0.2 to <0.5, and 0.01 to 0.2 ng/mL, respectively. Although the target-to-background ratio improved significantly over time (P < 0.0001), the majority (96.6%) of all lesions suggestive of recurrent disease could already be detected in standard imaging. Delayed imaging at 3 h p.i. exclusively identified pathologic findings in 5.4% (10/184) of abnormal [68Ga]PSMA I&T PET/CT scans, and exclusively detected 3.4% (38/1134) of all lesions suggestive of recurrent disease.
Conclusions
[68Ga]PSMA I&T PET/CT shows high detection rates in patients with prostate-specific antigen persistence or biochemical recurrence of prostate cancer. Delayed imaging can detect lesions with improved contrast compared to standard imaging. However, the impact on detection rates was limited in this study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the most common malignancy in men and a major cause of cancer deaths worldwide [1, 2]. After primary therapy for prostate cancer, a substantial number of patients will ultimately suffer from biochemical recurrence. In a recent study, the 5-year biochemical recurrence-free survival rates following radical prostatectomy or high-dose rate brachytherapy with external beam radiation therapy were 82.1% vs. 80.3%, respectively [3]. Monitoring of prostate specific antigen (PSA) is a reliable and cost-effective way to detect disease relapse. However, it is crucial for further treatment planning to detect and differentiate local, regional, or systemic recurrent prostate cancer. Previously applied imaging methods such as bone scintigraphy and PET with radiolabelled choline derivatives exhibit considerable limitations, particularly in the setting of PSA <10 ng/mL [4, 5].
The prostate-specific membrane antigen (PSMA) has therefore recently gained prominence as a molecular target for both clinical imaging and radionuclide therapy of prostate cancer [6–10]. [68Ga]PSMA ligand PET/CT represents a highly sensitive clinical imaging procedure for image-based restaging of prostate cancer in the context of biochemical recurrence, as well as for evaluation of PSMA-targeted radionuclide therapy [7, 8]. As such, several PSMA-targeting PET radiopharmaceuticals have become available for clinical imaging, including [68Ga]PSMA HBED-CC and [68Ga]-DOTAGA-(3-iodo-y)fk(Sub-KuE)—[68Ga]PSMA I&T [6, 10]. [68Ga]PSMA I&T has recently been introduced as an alternative to [68Ga]PSMA HBED-CC which is a pure PET radiopharmaceutical that cannot be labelled with therapeutic radionuclides [10]. In contrast to other ligands, PSMA I&T can be labelled alternatively with lutetium ([177Lu]PSMA I&T) without significant changes in affinity, which may allow for treatment of prostate cancer [9]. The introduction of this theranostic PSMA ligand offers new opportunities for diagnosis and therapy of recurrent prostate cancer [11, 12]. In a recent study, the detection rate of PET/CT using [68Ga]PSMA I&T has been evaluated in a first rather small cohort of patients with biochemical relapse of prostate cancer, demonstrating high detection rates that were comparable to [68Ga]PSMA HBED-CC [13].
In other malignancies, tracer uptake in malignant lesions has been shown to increase over time, and delayed imaging may contribute to a significantly higher detection rate of metastases [14, 15]. [68Ga]PSMA ligand PET/CT conducted at 60 min after tracer injection is the most widely used protocol [7, 8], and reported data for [68Ga]PSMA I&T were acquired at about 80 min p.i. [13]. Additional benefit from delayed imaging has been suggested for other ligands such as [68Ga]PSMA-HBED-CC, demonstrating increasing standardized uptake values (SUVs) over time and improving target-to-background (T/B) ratios [6, 16]. However, data are limited, and delayed imaging using [68Ga]PSMA I&T has not been evaluated systematically before.
Therefore, the aim of this study was to assess the incremental value of abdominal [68Ga]PSMA I&T PET delayed images. For this purpose, we compared the detection rates, SUVs and T/B ratios in a large cohort of prostate cancer patients using a standard protocol with whole-body imaging at 1 h p.i. and delayed abdominal imaging at 3 h p.i.
Materials and methods
Study population
The study population of this retrospective study consisted of 240 men (69.8 ± 7.5 years; range, 46.4–89.8 years) who were referred for a [68Ga]PSMA I&T PET/CT for detection of biochemical recurrence or PSA persistence after primary therapy for prostate cancer between November 2014 and March 2016. Biochemical failure is usually defined as presence of a PSA greater than 0.2 ng/mL after prostatectomy or as three successive rises above nadir following radiation therapy according to the American Society for Therapeutic Radiation and Oncology (ASTRO) definition of failure [17, 18]. We also included patients with a PSA level < 0.2 ng/ml to explore the prevalence of metastases in this subgroup. Patients were included if they had a history of prostate cancer, verified by histopathological evaluation, and presented with biochemical recurrence/persistence as determined by PSA levels. Exclusion criteria were: salvage radical prostatectomy, transurethral resection of the prostate (TURP), cryosurgical ablation of the prostate, high-intensity focused ultrasound (HIFU), irreversible electroporation (IRE), chemotherapy, radiation therapy for metastatic disease, bone-targeted therapy with radium-223, and PSMA-targeted radionuclide therapy. Some (n = 23) patients have been included in a previous manuscript evaluating diuretic PSMA imaging, but without analysis of detection rates [19].
Details on patient characteristics are summarized in Table 1. 209 (87%) patients had undergone radical surgery, and 31 (13%) patients external beam radiation therapy (EBRT) or (combined) brachytherapy for primary treatment. 36 (15%) patients had received androgen deprivation therapy (ADT) within the last 6 months prior to the examination. All studies were performed in the course of clinical diagnostic work-up of patients and [68Ga]PSMA I&T was administered in compliance with the Declaration of Helsinki, §37 and the German Medicinal Products Act, AMG §13.2b. Written informed consent was obtained from all patients according to institutional guidelines. The data analysis was presented to the local institutional review board, and the need for a formal review was waived.
Preparation of the PSMA-targeting ligand
[68Ga]PSMA I&T [9] was synthesized by a fully automated, good manufacturing practice/compliant procedure [20] using a GRP module (SCINTOMICS GmbH, Fürstenfeldbruck, Germany) connected to a [68Ge]/[68Ga] generator (30 mCi Obninsk Generator, Eckert & Ziegler EUROTOPE GmbH, Berlin, Germany) and equipped with a disposable single-use cassette kit (ABX, Radeberg, Germany). A standardized labeling sequence with 22.5 μg (15 nmol) of unlabeled PSMA I&T (SCINTOMICS GmbH, Fürstenfeldbruck, Germany) was used. Before application, the radiopharmaceuticals were analyzed according to the monographs 2462 (gallium chloride) and 2482 (gallium edotreotide) of the European Pharmacopoeia by analytic high-performance liquid chromatography. Radioanalytic high-performance liquid chromatography was performed on a Varian ProStar high-pressure gradient system equipped with an utraviolet/visible light (UV/Vis) detector (Varian ProStar 335) and a radiodetector (Berthold LB 3800-20 with LB 6657 probe) using an RP-18 column (Gemini C18 5μ 110A, 250 ×; Phenomenex, Torrance, CA, USA). The eluent had a linear gradient from 100% solvent A (phosphate buffer/acetonitrile, 85:15) to 100% solvent B (phosphate buffer/acetonitrile, 65:35) over 25 min at a flow of 0.6 ml/min.
PET/CT acquisition and image reconstruction
All studies were obtained on a dedicated PET/CT system (Siemens Biograph mCT 128 Flow; Siemens, Knoxville, TN, USA), equipped with an extended field-of-view LSO PET component, a 128-slice spiral CT component, and a magnetically driven table optimized for continuous scanning. The patients received an intravenous injection of 98 ± 26 MBq of the [68Ga]PSMA ligand. Imaging started with a low-dose non-enhanced helical CT (120kV, mA modulated, pitch 1.2, reconstructed axial slice thickness 5.0 mm) performed for attenuation correction of PET acquisitions. Whole-body PET images were then acquired in all patients using continuous bed motion (CBM) at a speed of 0.9 mm/s for chest and abdomen and 2.1 mm/s for legs at 1 h p.i. (about 25 min of acquisition time for an average patient). After completion of the first scan, each patient received 0.5 mg of furosemide per kilogram of body weight (maximum, 40 mg) followed by oral hydration with 1.5 L of water. Patients were advised to void the bladder frequently to favour urinary excretion and minimize exposure to radiation. PET images were acquired directly after the last voiding of the bladder. At 3 h p.i., delayed PET imaging of the abdomen was performed at a table speed of 0.5 mm/s (about 15 min for an average patient). All studies were reconstructed identically, using time-of-flight and point spread function (PSF) information combined with an iterative algorithm (Ultra HD®, Siemens Healthcare; 2 iterations, 21 subsets, matrix 200; zoom 1.0; Gaussian filter of 5.0). Intravenous contrast material was not administered.
Image analysis and quantification of tracer uptake
All PET/CT images were analyzed by one board-certified nuclear medicine physician and one board-certified radiologist in consensus using a dedicated workstation equipped with a commercial software package (syngo.via; Siemens Healthcare), which allowed the review of PET, CT and fused imaging data. All lesions suggestive for recurrent prostate cancer were noted and grouped with respect to their localization into local recurrence, lymph node metastases, bone metastases, and other metastases (e.g. lung) [8].
In PET, any focal uptake of [68Ga]PSMA I&T higher than background and not associated with physiologic uptake was judged as tissue suspicious of malignancy. Criteria for interpretation of hybrid [68Ga]PSMA ligand PET/CT have been recently published [21]. The numbers of detected metastases per patient was recorded. In case of multiple metastases, only the five metastases with the highest SUV were further analyzed in each suggestive anatomical field (i.e. lymph nodes, bone, other organs). To calculate SUVs, an isocontour volume of interest including all voxels above 45% of the maximum was created, covering the whole lesion volume, as performed recently in a similar way [22]. Within all volumes of interest, mean and maximum SUVs were measured. Measurements were performed in images at 1 and 3 h p.i. Background activity was determined by drawing circular ROIs in gluteal muscle tissue sparing intramuscular vessels (= background SUVmean), and T/B ratios were calculated for each lesion [13, 23]. For the quantitative comparison of tracer uptake in metastases in imaging at 1 and 3 h p.i., only abdominal metastases visualized on both acquisitions were analyzed, i.e. metastases outside the scan volume of the delayed scan were not included in that comparison.
Validation criteria
Imaging findings were validated in 46.7% (112/240) of patients by at least one of the following procedures: (a) histological analysis after salvage radical lymph node dissection, CT-guided biopsy of metastases or transrectal ultrasound-guided biopsy (n = 16); (b) clinical follow-up including contrast enhanced-CT, magnetic resonance imaging (MRI), bone scintigraphy (BS) and repeated [68Ga]PSMA ligand PET/CT confirming the initial suspicious lesion(s) or showing disappearance of suspected metastatic sites after local/systemic treatment and corresponding PSA decline (n = 99).
Statistical analysis
Categorical variables are presented with absolute and relative frequencies. Continuous variables are expressed as mean ± SD and range. PSA-stratified detection rates were calculated as the rate of [68Ga]PSMA I&T PET-positive results for five pooled subgroups (0.01 to 0.2 ng/mL, >0.2 to <0.5, 0.5 to <1.0 ng/mL, 1.0 to <2.0 ng/mL, and ≥2.0 ng/mL), as described previously [8]. We added a subgroup with a lower limit for PSA of 0.01 to include also patients with very low PSA levels. PSA-stratified detection rates were calculated with 95% confidence intervals. The D’Agostino–Pearson omnibus normality test was used to test if the values come from a Gaussian distribution. SUV and T/B ratio measurements at different imaging time points were compared using a paired two-sided t test. Fisher’s exact test was used to compare differences in detection rates on PET/CT. Statistical significance was established for p values of ≤0.05. Statistical analysis was performed using GraphPad Prism 6.0® for Windows.
Results
Detection rate
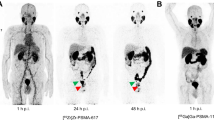
Of the 240 patients, 184 (76.7%) showed at least 1 localized area suggestive for recurrent prostate cancer on PET images. [68Ga]PSMA I&T PET/CT revealed lymph node metastases in 115 (62.5%) of these patients, bone metastases in 62 (33.7%) patients, and local recurrences in 49 (26.6%) patients. In addition, we noted pulmonary metastases in 8 (4%) patients, hepatic metastases in 3 (2%) patients, adrenal metastases in 2 (1%) patients, a peritoneal metastasis in 1 (0.5%) patient, a muscular metastasis in 1 (0.5%) patient and a testicular metastasis in 1 (0.5%) patient. The overall detection rates of [68Ga]PSMA I&T PET/CT were 94.2% (113/120) for a PSA value of ≥2 ng/mL, 71.8% (28/39) for a PSA value of 1 to <2 ng/mL, 58.6% (17/29) for a PSA value of 0.5 to <1 ng/mL, 55.9% (19/34) for a PSA value of >0.2 to <0.5, and 38.9% (7/18) for a PSA value of 0.01 to 0.2 ng/mL. When analysing detection rates of [68Ga]PSMA I&T PET/CT in the subgroup of patients after radical prostatectomy [PSA, 13.2 ± 60.5 ng/mL (range, 0.02–700 ng/mL)], detection rates were 95.7% (89/93) for a PSA value of ≥2 ng/mL, 69.4% (25/36) for a PSA value of 1 to <2 ng/mL, 60.7% (17/28) for a PSA value of 0.5 to <1 ng/mL, 55.9% (19/34) for a PSA value of >0.2 to <0.5, and 38.9% (7/18) for a PSA value of 0.01 to ≤0.2 ng/mL. When analysing detection rates of [68Ga]PSMA I&T PET/CT in the subgroup of patients after radiation therapy [PSA, 8.4 ± 9.9 ng/mL (range, 0.8–47.5 ng/mL); nadir PSA 2.7 ± 4.3 ng/mL (range, 0.05–21.9)], detection rates were 88.9% (24/27) for a PSA value of ≥2 ng/mL, 100% (3/3) for a PSA value of 1 to <2 ng/mL, and 0% (0/1) for a PSA value of 0.5 to <1 ng/mL. Mean PSA was significantly lower in patients with negative [68Ga]PSMA l&T PET/CT results than in patients with positive results (1.1 ± 1.3 vs. 16.6 ± 64.8, P = 0.001). The detection rate of [68Ga]PSMA I&T PET/CT increased with increasing PSA levels. The contribution of standard and delayed imaging in [68Ga]PSMA I&T in biochemical relapse of prostate cancer is illustrated in Fig. 1.
Impact of delayed abdominal imaging on detection rates
A total of 1134 lesions suggestive of recurrent disease [646 lymph node metastases, 410 bone metastases, 49 local recurrences and 29 other metastases (e.g. hepatic or adrenal)] were detected in abdominal imaging at 1 and 3 h p.i. when combining information from both scans. When analyzing the additional impact of delayed abdominal imaging, lesions suggestive of recurrent disease were exclusively detected in delayed imaging at 3 h p.i. in 10 (5.4%) patients (local recurrences in 9 patients, and lymph node metastases in 1 patient). The difference in detection rates between 1 h (174 positive PET/CT scans) and 3 h p.i. (184 positive PET/CT scans) was not statistically significant (P = 0.35). The relative PSA-stratified performance of [68Ga]PSMA I&T PET/CT at 1 and 3 h p.i. is illustrated in Fig. 2. In total, 20 additional lymph node metastases, 15 local recurrences, and 3 additional bone metastases were exclusively detected in delayed abdominal imaging. Conversely, 1096 (96.6%) of 1134 abdominal lesions suggestive of recurrent disease could be detected in imaging at 1 h p.i. When comparing [68]Ga-PSMA I&T uptake in malignant lesions at 1 and 3 h p.i., tracer uptake remained stable over time when analysing the entire study population (Fig. 3). However, we also observed declining tracer intensity in metastases over time. Tracer uptake (SUVmax) declined by 28.6 ± 17.2% in 249 (22.0%) tumor lesions (163 lymph node metastases, 65 bone metastases, 13 local recurrences, and 8 other metastases) in 106 (57.6%) patients over time [SUVmax, 24.8 ± 22.2 (range, 2.1 to 160.5) at 1 h p.i. vs. 18.3 ± 17.8 (range, 1.1–149.6) at 3 h p.i].
Detection rates of [68Ga]PSMA I&T PET/CT scans in patients with biochemical relapse divided in five subgroups in relation to PSA levels. (a) Histograms of absolute numbers of [68Ga]PSMA I&T PET/CT-positive and PET/CT-negative patients in relation to PSA levels at 1 and 3 h p.i. (b) [68Ga]PSMA I&T detection rates with 95% confidence intervals divided in relation to PSA levels. The difference in detection rates between 1 h (174 positive PET/CT scans) and 3 h p.i. (184 positive PET/CT scans) was not statistically significant (P = 0.35). PSA = prostate-specific antigen
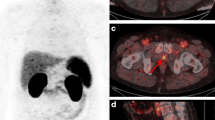
The background activity decreased significantly over time (0.36 ± 0.08 vs. 0.23 ± 0.07, P < 0.0001). Consequently, the T/B ratio improved significantly in lymph node metastases, bone metastases and local recurrences (P < 0.0001). Detailed data on the different regions involved by recurrent disease, intensity of tracer uptake and T/B ratios at 1 and 3 h p.i. are listed in Table 2. Example images of metastases at 1 and 3 h p.i. in [68Ga]PSMA I&T PET/CT are shown in Figs. 4 and 5.
Histopathology and follow-up
In 16 patients, [68Ga]PSMA I&T PET/CT-positive local recurrences or metastases were histologically confirmed. In 99 patients, follow-up/imaging (PET/CT, CT, MRI, BS) undisputably proved that the positive findings were metastases or local recurrences. In 17 of these patients, radiation therapy or chemotherapy followed by a substantial decrease in PSA and/or decreasing PSMA uptake of suspicious findings in a consecutive [68Ga]PSMA ligand PET/CT scan proved the malignant nature of PSMA-positive lesions.
Discussion
In the present study, we systematically evaluated the incremental value of [68Ga]PSMA I&T PET delayed abdominal images. We confirmed the high detection rate of [68Ga]PSMA I&T PET/CT in the context of biochemical relapse of prostate cancer, enabling lesion detection even in the setting of low PSA levels ≤0.2 ng/mL in 38.9% of cases.
Recently, [68Ga]PSMA Iigand PET/CT has become a powerful tool for localization of disease in patients with elevated PSA levels after primary therapy for prostate cancer. While there are numerous studies on the use of the PSMA ligand [68Ga]PSMA HBED-CC for that purpose [6–8], data on other ligands including PSMA I&T are still limited. Of note, PSMA I&T PSMA is a theranostic ligand, meaning that it may be labelled with lutetium-177 ([177Lu]PSMA I&T) which is convenient for therapeutic concepts in advanced prostate cancer [9, 12].
In a recent pilot study, Berliner and colleagues have reported on the detection rate of [68Ga]PSMA I&T PET/CT in 80 patients with biochemical relapse of prostate cancer. They observed a detection rate of 0.52, 0.55, 0.70 and 0.93 at 0.2 to <0.5 ng/mL, 0.5 to <1.0 ng/mL, 1.0 to <2.0 ng/mL, and ≥2.0 ng/mL, respectively [13]. In that study, [68Ga]PSMA I&T PET/CT yielded similar results compared to other studies using [68Ga]PSMA HBED-CC [7, 8]. The detection rates in our study (0.56, 0.59, 0.72 and 0.94) were very similar, underlining the high sensitivity of [68Ga]PSMA I&T. Interestingly, that group reported very low SUV values of metastases detected on [68Ga]PSMA I&T PET, which were much lower than previously reported values for [68Ga]PSMA HBED-CC [7, 23]. This may in part be explained by the fact that they used a PET/CT scanner with a reconstruction technique without PSF modelling and time-of-flight (TOF) reconstructions. Considerably higher SUVs have been consistently reported when using PSF and TOF reconstructions [24], and a state-of-the art PET system was used in this study.
When looking at the incremental value of delayed imaging at 3 h p.i., we only observed a limited benefit in clinical routine. When looking at the entire study population, SUVs in metastases and local recurrences showed some increase in the intensity of [68Ga]PSMA I&T uptake over time, but that difference was not consistently significant for all localizations of disease or types of SUV measurement. However, due to the significant decrease in background activity, the T/B ratio considerably improved over time (P < 0.0001). Nevertheless, that higher lesion contrast did not translate into significantly higher overall detection rates (P = 0.35), although pathologic [68Ga]PSMA I&T accumulation could be exclusively detected on delayed images in 10 additional patients. 9 of these 10 patients had local recurrences, underlining that these may be particularly difficult to depict on non-diuretic standard images. A recent study has evaluated various diuretic protocols for [68Ga]PSMA I&T PET/CT, and shown that early co-injection of a radiotracer with furosemide may provide good image quality of the prostate bed even in images at 1 h p.i. [19], questioning the need for routine delayed imaging. Early co-injection of radiotracer and furosemide causes a significant reduction of bladder activity at 1 h p.i. which may allow for better detection of local recurrences [19]. Such an approach may be particularly attractive with regard to busy clinical departments. However, one may hypothesize that early co-injection may also cause accelerated excretion of radiotracers, limiting tracer availability and potentially affecting detection rates. In this study, the vast majority (96.6%) of lesions suggestive of recurrent disease could already be detected in imaging at 1 h p.i., showing that delayed imaging in [68Ga]PSMA I&T PET does not increase the number of detected metastases to a significant extent. Other studies have looked into the additional value of delayed imaging in [68Ga]PSMA-HBED-CC PET, and found that a 3-h delay after injection was optimal timing for [68Ga]PSMA-HBED-CC PET/CT [25]. In that study, only 63% of lesions suggestive of recurrent disease could be detected at 1 h p.i. [25]. However, the examined patient cohort was very small and the optimal imaging timing for [68Ga]PSMA-HBED-CC needs to be also evaluated in larger patient cohorts. In another study evaluating the usefulness of dual-time point (biphasic) [68Ga]PSMA-HBED-CC PET/CT in patients with prostate cancer, an increase in SUVmax was observed between 1 and 3 h p.i. in both lymph node metastases (P = 0.002) and bone metastases (P < 0.001) [23], consistent with findings from this study using a different ligand. Interestingly, we also observed declining tracer activity in a substantial number of metastases (22.0%), even in metastases with very high PSMA ligand uptake at 1 h p.i. We hypothesize that this may in part be explained by the fact that physical half-life of 68Ga is relatively low, and a substantial part of previously bound [68Ga]PSMA I&T will have decayed at 3 h p.i. In addition, only <1.5% of the injected activity is found per liter of blood at 1 h p.i. because of rapid clearance, limiting the available tracer for continued accumulation [10]. Furthermore, given the relatively low injected activities in this study, the residual activity at 3 h p.i. is limited, influencing image noise and the reliability of quantification, which may have contributed to declining SUVs. Given the high detection rates at 3 h p.i., one could speculate that dosage could be further reduced with modern scanners when imaging at 1 h p.i. is performed. However, although robust qualitative assessment of the presence of tumor lesions is possible, quantitative uptake measurements may be less reliable with low activities.
Routine introduction of dual-phase imaging may be difficult in busy clinical environments, and seems to have limited benefit for patients. Based on our data, imaging at 1 h p.i. is sufficient for [68Ga]PSMA I&T, and imaging with one single acquisition with a 3-h delay would only optimize the lesion contrast. Indeed, clinical routine in most institutions for the reasons stated is a 1 h post-injection acquisition. One could argue that a single delayed whole-body acquisition at 3 h p.i. may represent an interesting alternative to early whole-body imaging, because the T/B ratio is higher at 3 h p.i. However, image noise is also higher in delayed images. In addition, given the low residual activity at 3 h p.i., the time needed to acquire PET images with a good diagnostic quality is twice as high compared to early imaging.
In addition to 68Ga-labelled PSMA ligands, 18F-labelled radiotracers such as 2-(3-(1carboxy-5-(6-[18F]fluoro-pyridine-3-carbonyl)amino]-pentyl)-ureido)-pentanedioic acid (18F-DCFPyL) offer some advantages including improved image resolution, longer half-life and increased production yield, and PSA-stratified performance has been shown to be non-inferior to 68Ga-PSMA-HBED-CC [26, 27].
When looking at patients after radiation therapy in this study, it is important to consider that the definition of biochemical recurrence is complex. There is an ongoing discussion about how to define failure following both radical prostatectomy and radiation therapy [17]. Biochemical recurrence has usually been defined as PSA >0.2 ng/mL after prostatectomy. After radiation therapy, recurrence may be defined as three consecutive rises in PSA according to the ASTRO definition, or alternatively as PSA +2 ng/ml above nadir according to the Phoenix criteria [17, 18]. However, the latter results in substantially lower estimates of biochemical recurrence at 5 years [17]. As shown by our data, metastases may now frequently be found at PSA <2 ng/mL above nadir after radiation therapy, or at ≤0.2 ng/mL after prostatectomy (38.9% of cases). This demonstrates that in the era of highly sensitive imaging and highly sensitive PSA testing, many of these patients can now be classified as having metastatic disease, questioning older definitions.
Some limitations of the present study should be acknowledged. First, we only evaluated one late imaging time point in this study. Additional time points may be included in future studies to further refine protocols. A recent study looked at multiple time points (5 min, and 1, 2, 3, 4 and 5 h after injection) using [68Ga]PSMA-HBED-CC in four patients [25]. However, such an approach would be difficult in larger patient cohorts. In addition, refinement of the CT protocol including full-dose CT and administration of i.v. contrast material may further improve the detection rate. However, the benefit of a full-dose, contrast-enhanced CT protocol has been shown to be limited in this context [8]. Second, due to the retrospective nature of the study, a histopathological reference standard was only available in some patients. Therefore, we may have missed some true lesions, e.g. in poorly differentiated prostatic carcinoma [28]. Also, false positive results cannot be excluded completely. However, any uptake of [68Ga]PSMA ligands above background activity seems to be highly specific for prostate cancer and is, therefore, regarded as true positive, unless otherwise proven [8, 13]. Afshar-Oromieh and colleagues did not observe false positive results in their study including histopatholgical evaluation of 42 patients [7]. Although follow-up was not available in all patients, due to the fact that many patients were examined on an outpatient basis, imaging-based or other validation of the observed metastases was available in a substantial part of patients in this study and undisputably proved that the positive findings were metastases or local recurrences. Moreover, we restricted the delayed imaging to an abdominal scan volume due to time constraints. Therefore, we could not compare tracer uptake in all metastases with delayed [68Ga]PSMA I&T PET scans. However, it is unlikely that the observed results would be different in other anatomical regions. Finally, although delayed imaging did not significantly improve overall detection rates, delayed imaging may nevertheless have clinical value, e.g. improving reader confidence. However, such additional aspects were not assessed in this study.
Conclusion
[68Ga]PSMA I&T PET/CT shows high detection rates in patients with PSA persistence or biochemical recurrence of prostate cancer. Delayed imaging can detect lesions with improved contrast compared to standard imaging. However, the impact on detection rates was limited in this study.
References
Torre LA, Bray F, Siegel RL, et al. Global Cancer Statistics, 2012. Ca – a Cancer J Clin. 2015;65:87–108.
Attard G, Parker C, Eeles RA, Schröder F, Tomlins SA, Tannock I, et al. Prostate cancer. Lancet. 2016;387(10013):70–82.
Boehm K, Schiffmann J, Tian Z, Lesmana H, Larcher A, Mandel P, et al. Five-year biochemical recurrence-free and overall survival following high-dose-rate brachytherapy with additional external beam or radical prostatectomy in patients with clinically localized prostate cancer. Urol Oncol. 2016;34:119.e11–8.
Kane CJ, Amling CL, Johnstone PA, Pak N, Lance RS, Thrasher JB, et al. Limited value of bone scintigraphy and computed tomography in assessing biochemical failure after radical prostatectomy. Urology. 2003;61:607–11.
Giovacchini G, Picchio M, Coradeschi E, Bettinardi V, Gianolli L, Scattoni V, et al. Predictive factors of [(11)C]choline PET/CT in patients with biochemical failure after radical prostatectomy. Eur J Nucl Med Mol Imaging. 2010;37:301–9.
Afshar-Oromieh A, Malcher A, Eder M, Eisenhut M, Linhart HG, Hadaschik BA, et al. PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40:486–95.
Afshar-Oromieh A, Avtzi E, Giesel FL, Holland-Letz T, Linhart HG, Eder M, et al. The diagnostic value of PET/CT imaging with the (68)Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42:197–209.
Eiber M, Maurer T, Souvatzoglou M, Beer AJ, Ruffani A, Haller B, et al. Evaluation of Hybrid 68Ga-PSMA Ligand PET/CT in 248 Patients with Biochemical Recurrence After Radical Prostatectomy. J Nucl Med. 2015;56:668–74.
Weineisen M, Schottelius M, Simecek J, Baum RP, Yildiz A, Beykan S, et al. 68Ga- and 177Lu-Labeled PSMA I&T: Optimization of a PSMA-Targeted Theranostic Concept and First Proof-of-Concept Human Studies. J Nucl Med. 2015;56:1169–76.
Herrmann K, Bluemel C, Weineisen M, Schottelius M, Wester HJ, Czernin J, et al. Biodistribution and radiation dosimetry for a probe targeting prostate-specific membrane antigen for imaging and therapy. J Nucl Med. 2015;56:855–61.
Rauscher I, Maurer T, Souvatzoglou M, Beer AJ, Vag T, Wirtz M, et al. Intrapatient Comparison of 111In-PSMA I&T SPECT/CT and Hybrid 68Ga-HBED-CC PSMA PET in Patients With Early Recurrent Prostate Cancer. Clin Nucl Med. 2016;41(9):e397–402.
Baum RP, Kulkarni HR, Schuchardt C, Singh A, Wirtz M, Wiessalla S, et al. 177Lu-labeled prostate-specific membrane antigen radioligand therapy of metastatic castration-resistant prostate cancer: safety and efficacy. J Nucl Med. 2016;57:1006–13.
Berliner C, Tienken M, Frenzel T, Kobayashi Y, Helberg A, Kirchner U, et al. Detection rate of PET/CT in patients with biochemical relapse of prostate cancer using [68Ga]PSMA I&T and comparison with published data of [68Ga]PSMA HBED-CC. Eur J Nucl Med Mol Imaging. 2017;44:670–77.
Zhuang H, Pourdehnad M, Lambright ES, Yamamoto AJ, Lanuti M, Li P, et al. Dual time point 18F-FDG PET imaging for differentiating malignant from inflammatory processes. J Nucl Med. 2001;42:1412–7.
Yen TC, Ng KK, Ma SY, Chou HH, Tsai CS, Hsueh S, et al. Value of dual-phase 2-fluoro-2-deoxy-d-glucose positron emission tomography in cervical cancer. J Clin Oncol. 2003;21:3651–8.
Giesel FL, Hadaschik B, Cardinale J, Radtke J, Vinsensia M, Lehnert W, et al. F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients. Eur J Nucl Med Mol Imaging. 2017;44:678–88.
Paller CJ, Antonarakis ES. Management of biochemically recurrent prostate cancer after local therapy: evolving standards of care and new directions. Clin Adv Hematol Oncol. 2013;11:14–23.
Consensus statement: guidelines for PSA following radiation therapy. American Society for Therapeutic Radiology and Oncology Consensus Panel. Int J Radiat Oncol Biol Phys. 1997;37:1035–41.
Derlin T, Weiberg D, von Klot C, Wester HJ, Henkenberens C, Ross TL, et al. 68Ga-PSMA I&T PET/CT for assessment of prostate cancer: evaluation of image quality after forced diuresis and delayed imaging. Eur Radiol. 2016;26:4345–53.
Martin R, Jüttler S, Müller M, Wester HJ. Cationic eluate pretreatment for automated synthesis of [68Ga]CPCR4.2. Nucl Med Biol. 2014;41:84–9.
Rauscher I, Maurer T, Fendler WP, Sommer WH, Schwaiger M, Eiber M. (68)Ga-PSMA ligand PET/CT in patients with prostate cancer: How we review and report. Cancer Imaging. 2016;16:14.
Rauscher I, Maurer T, Beer AJ, et al. Value of 68Ga-PSMA HBED-CC PET for the assessment of lymph node metastases in prostate cancer patients with biochemical recurrence: comparison with histopathology after salvage lymphadenectomy. J Nucl Med. 2016;57:1713–9.
Sahlmann CO, Meller B, Bouter C, Ritter CO, Ströbel P, Lotz J, et al. Biphasic 68Ga-PSMA-HBED-CC-PET/CT in patients with recurrent and high-risk prostate carcinoma. Eur J Nucl Med Mol Imaging. 2016;43:898–905.
Armstrong IS, Kelly MD, Williams HA, Matthews JC. Impact of point spread function modelling and time of flight on FDG uptake measurements in lung lesions using alternative filtering strategies. EJNMMI Phys. 2014;1:99.
Afshar-Oromieh A, Hetzheim H, Kübler W, Kratochwil C, Giesel FL, Hope TA, et al. Radiation dosimetry of (68)Ga-PSMA-11 (HBED-CC) and preliminary evaluation of optimal imaging timing. Eur J Nucl Med Mol Imaging. 2016;43:1611–20.
Li X, Rowe SP, Leal JP, Gorin MA, Allaf ME, Ross AE, et al. Quantitative Parameters in PSMA-targeted PET Imaging with 18F-DCFPyL: Variability in Normal Organ Uptake. J Nucl Med. 2016. PMID: 27932557.
Dietlein F, Kobe C, Neubauer S, Schmidt M, Stockter S, Fischer T, et al. PSA-stratified performance of 18F- and 68Ga-labeled tracers in PSMA-PET imaging of patients with biochemical recurrence of prostate cancer. J Nucl Med. 2016. PMID: 27908968.
Chakraborty PS, Tripathi M, Agarwal KK, Kumar R, Vijay MK, Bal C. Metastatic Poorly Differentiated Prostatic Carcinoma With Neuroendocrine Differentiation Negative on Ga-68-PSMA PET/CT. Clin Nucl Med. 2015;40:E163–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Prof. Dr. Hans-Jürgen Wester is a shareholder of Scintomics. All other authors have nothing to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Schmuck, S., Nordlohne, S., von Klot, CA. et al. Comparison of standard and delayed imaging to improve the detection rate of [68Ga]PSMA I&T PET/CT in patients with biochemical recurrence or prostate-specific antigen persistence after primary therapy for prostate cancer. Eur J Nucl Med Mol Imaging 44, 960–968 (2017). https://doi.org/10.1007/s00259-017-3669-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3669-5