Abstract
Purpose
Positron emission tomography-computed tomography (PET-CT) is a resource-demanding imaging modality with increasing popularity in the workup of patients with suspected or proven lung cancer.
Methods
To review the clinical usefulness of this imaging modality in the diagnosis, staging, and pre-operative evaluation, we conducted a systematic literature search, review, and quality assessment using the rapid evidence assessment toolkit and the Oxford Centre for Evidence-Based Medicine methodology. The literature search resulted in 4,208 records including 918 reviews, of which 139 met the predefined criteria and were read in full to identify relevant original articles on F-18 FDG PET-CT (1) in the evaluation of solitary pulmonary nodules (n = 14), (2) in curative-intent treatment trials (n = 9), and (3) in planning of invasive procedures (n = 18).
Results
We found the following important results from the literature review:
-
1)
PET-CT can rule out malignancy in most solitary pulmonary nodules due to high sensitivity (recommendation level A).
-
2)
PET-CT reduces the number of futile treatment trials (recommendation level A).
-
3)
The sensitivity of PET-CT in general is insufficient to rule out mediastinal lymph node metastasis (recommendation level A).
Conclusions
ᅟ
-
1)
With few exceptions, solitary pulmonary nodules can safely be considered benign if the PET-CT scan is negative. Exceptions consist of small (<1 cm) and non-solid, solitary pulmonary nodules. These abnormalities should be followed up by CT in a structured programme.
-
2)
No curative-intent treatment should be commenced until a PET-CT scan has excluded occult distant metastases.
-
3)
In general, lymph node metastasis in the mediastinum cannot be ruled out on the basis of a negative PET-CT, and confirmative invasive staging should be performed in most patients before mediastinal metastasis is confirmed or ruled out.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the introduction of positron emission tomography (PET) in the 1970s and of PET-computed tomography (PET-CT) in clinical practice since the turn of the millennium, the use of molecular PET imaging has increased substantially, and so have the associated costs [1, 2]. There is at present no indication that a plateau in the use of PET-CT rise has been reached, and therefore a review of the clinical utility of PET-CT should be of interest to clinicians involved in the use of PET-CT [3, 4].
In addition to the national Danish Lung Cancer Group (DLCG, DK) [5], many major international thoracic and oncology societies and organizations, such as the National Institute for Health and Care Excellence (NICE, UK) [6], National Comprehensive Cancer Network (NCCN, USA, adapted by the European Respiratory Society, ERS) [7, 8], American College of Chest Physicians (ACCP, USA) [9–12], European Society of Thoracic Surgeons (ESTS) [13], and European Society for Medical Oncology (ESMO) [14, 15], have published recommendations for the use of F-18 FDG PET-CT in lung cancer. These are, however, only moderately consistent.
Numerous review articles on PET-CT in lung cancer have been published during the last decade. The vast majority of these, however, focus on the diagnostic accuracy of PET-CT and only to a lesser extent on the clinical value that PET-CT potentially offers in the diagnostic workup. Thus, such contributions do not provide a significant clinical value to the diagnostic process in lung cancer, as illustrated in Fig. 1. If a diagnostic modality can aid the process from A to B to C, its use appears to be clinically justified if no other argument (like complications, expenses, or availability) contradicts this. If a diagnostic modality does not facilitate getting from A to B to C, then the clinical utility is not present, or is at best limited. Three examples to illustrate this are given below:
-
1)
One study has provided evidence that PET-CT has a sensitivity to detect a certain condition (like mediastinal involvement of lung cancer) of 75 % compared to 50 % for CT; while this is interesting from an academic point of view, these findings have limited clinical importance, as these percentages mean that neither PET-CT nor CT can rule out the disease in question.
-
2)
If PET-CT is able to prevent a futile thoracotomy (as reported in some papers), this is highly relevant clinical information, but if PET-CT was “only” able to change the staging of the patient, but no immediate treatment differences resulted (e.g. detection of N1 disease in a patient thought to have NO disease), this would be less relevant clinically, although interesting academically.
-
3)
It is not important for the workup if the patient has six metastatic lesions in the liver detected by CT, or eight detected by PET-CT; although PET-CT is more sensitive in detecting liver metastases than CT in this example, it will have no therapeutic consequences.
This particular focus on the clinical relevance is where our paper differs from many other reviews on PET-CT in lung cancer evaluation. The increasing use of PET-CT poses a significant challenge to the health care system due to its ever-increasing expenses. While health care systems internationally face financial constraints, the incidence and prevalence of lung cancer is not equally decreasing, adding great demand to the health care systems with regard to providing safe and efficient health services to all patients [16]. Accordingly, the health care directorate of the Region of Southern Denmark had experienced a steady rise in the use of PET-CT during recent years with a trend towards a continuous increase. Thus, the capacity of the current PET-CT scanners in the region is under pressure. As a basis for planning the future capacity and clinical use of PET-CT in the region, the regional health directorate commissioned a review on the evidence of the clinical value of PET-CT in diagnosis, staging, and follow-up in six types of cancer, which occupied about 2/3 of the PET-CT scanning capacity in the region in 2012. The time frame for the review was limited to eight months.
The objective of this study was to identify and describe the clinically relevant evidence for the use of F-18 FDG PET-CT in the initial diagnostic process of lung cancer, related to the following items:
-
1)
Can PET-CT reliably discriminate a benign from a malignant solitary pulmonary nodule (SPN) on CT and thereby prevent potentially dangerous lung biopsy?
-
2)
Can PET-CT prevent futile curative-intent treatment trials, for instance by revealing occult metastases?
-
3)
Can PET-CT reliably detect or exclude mediastinal lymph node metastasis and thereby obviate surgical or endoscopic mediastinal staging?
Other potential uses of PET-CT in lung cancer management (like screening and follow-up) are not covered in this article, which focuses on the use of PET-CT in initial lung cancer evaluation.
Material and methods
The review comprised a systematic literature search, an article selection procedure with predefined in- and exclusion criteria, and a summation of the results. The methods and designs of the included studies were so heterogeneous that it was deemed not applicable to perform statistical analysis (e.g., creating forest plots) of the results. Instead, it was deemed more worthwhile to describe the important findings of the included papers. The review is, therefore, not a straightforward systematic review, but a combination of a systematic search and a more narrative summation [17].
Initially, three search questions were formulated using the population, intervention, comparator, outcome (PICO) strategy [18]. Each question addressed different PICO-domains, as described in the results section.
Systematic literature search
An overall search strategy was designed to answer these three PICO-questions. Relevant search terms were identified by clinicians (a nuclear medicine specialist (PCH) and a respiratory medicine specialist (PHM)) and validated by the Medical Research Library of Odense University Hospital. Search terms included the combination of multiple synonyms for PET, PET-CT, and lung cancer, as displayed in Appendix 1. The search covered the PubMed, Embase, and Cochrane databases from January 2003 to the search date and was limited to papers in English, Danish, Swedish, and Norwegian. The Medical Research Library of Odense University Hospital performed the searches for all articles and all reviews on October 23, 2013, and the results were exported to an EndNote database (version 7).
Study selection
Study selection was performed using the Rapid Evidence Assessment (REA) methodology, which is particularly recommended when a comprehensive, transparent, and timely input is needed to inform health policy decision makers [19]. Despite the lack of consensus on and consistency in REA methodology [20] REA is widely used by Health Technology Assessment (HTA) producers worldwide to address the informational needs for health care decision makers in a timely manner [21]. REA can provide a rapid synthesis of the evidence on a defined and specific topic by shortening the process of the traditional systematic review, which typically takes 8–12 months to perform, but without compromising the inherent logic behind the full systematic review. REA provides a balanced assessment of a clinical problem by using the methodology for systematic reviews to search, sort, and evaluate the available evidence of a defined topic while limiting the comprehensiveness in each process—for instance, by focusing on a few or only a single research question, by assessing literature from a limited time period (like 10 years), or by including only data from existing evidence summaries and reviews articles rather than primary studies. In this way the entire process may be shortened to 2–6 months depending on the nature of the limits [22, 23].
As suggested by the REA methodology, the review articles were sorted by their titles and abstracts according to the pre-planned in- and exclusion criteria. Inclusion criterion consisted of articles that described the use of F-18 FDG PET-CT in the clinical situations that were covered by PICO-questions. For all excluded papers, a record was kept to document why the paper was excluded in case this would later become relevant. This sorting was conducted by one of the authors (PHM).
If no, or sparse, relevant evidence could be found regarding PET-CT, we included papers on PET alone, assuming that PET–CT would provide a comparable or better result [24].
The included review articles (n = 139) were read in toto by one of the authors (PHM) to identify relevant original articles, and the quality of the original studies was assessed according to the Oxford Centre for Evidence-Based Medicine (CEBM) and assigned an evidence level from 1 to 5, where 1 represents the highest quality of evidence [25]. As supported by the REA methodology, we did not use a systematic quality appraisal tool in addition to the CEBM assessment [19].
Summation of results
Finally, the results of the included articles were summarized in evidence tables consisting of: Purpose of study, study design, study period, study population, number of patients in the study, results, comments, and evidence level according to the Oxford CEBM [25]. From these evidence tables, recommendations for the use of PET-CT in lung cancer were given, using the recommendation grading scale from A to D, where A represents the strongest recommendation [25]. This grading was also conducted by one of the authors (PHM).
Results
This search resulted in 4,208 articles, of which 981 were classified as reviews in the databases (Fig. 2). Articles excluded from the review (n = 842) were distributed on the following exclusion criteria: not a relevant type of paper (e.g. editorial) (n = 71), non-English or Scandinavian language (n = 2), articles on non-lung cancer (n = 66), articles on PET-CT in other forms of workup (not primary diagnosis) (n = 102), articles on PET-CT in treatment decisions (such as treatment response evaluation after radiotherapy) (n = 232), and articles not related to the asked PICO-question (e.g. basic research, technical issues, and animal experiments) (n = 369). As shown in Fig. 2 and Table 1, the selection process resulted in 14 original papers on PET or PET-CT in the evaluation of SPNs (of which three described bronchoalveolar carcinoma (BAC) and carcinoids), nine original articles on PET or PET-CT in curative-intent treatment trials, and 18 original papers on PET or PET-CT in planning of invasive procedures. Of the latter 18 papers, nine focused on the clinical value of PET-CT for the characterisation of intrathoracic lymph nodes. The main clinically important findings reported in these articles are summarised in Table 1 and mentioned briefly in the text.
Article selection. Of 981 articles classified as review articles by the databases, 842 were excluded. The remaining 139 review articles were sorted according to which PICO question the article answered, distributed as follows: 60 review articles dealt with PICO 1 (evaluation of pulmonary nodules), 124 articles addressed PICO 2 (futile curative-intent treatment), and 41 articles covered PICO 3 (planning of invasive procedures). As several articles dealt with more than one of the PICO questions, the combined number is not 139. aAs seen in the distribution of excluded articles, not all articles classified as reviews by the databases were, in fact, reviews. bReasons for exclusion of articles from the review (n = 842) were: not a relevant type of paper (e.g. editorial) (n = 71), non English or Scandinavian language (n = 2), articles on non-lung cancer (n = 66), articles on PET-CT in other forms of workup (not primary diagnosis) (n = 102), articles on PET-CT in treatment decisions (such as treatment response evaluation after radiotherapy) (n = 232), and articles not related to the asked PICO-question (e.g. basic research, technical issues, and animal experiments) (n = 369). cIn total, 139 review articles were included and read. As several review articles dealt with more than one of the PICO questions, the combined number of relevant review articles from each PICO question (60 + 124 + 41) does not equal 139. dOf these 18 original articles, nine dealt with mediastinal staging. Only these nine are considered in the text
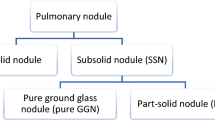
Can PET-CT reliably discriminate a benign from a malignant lesion on CT and thereby prevent potentially dangerous lung biopsy?
To answer this, the following PICO question was initially posed: “What is the effect on the use of invasive tests and possibly overlooked malignancy (O) of PET-CT (I) in evaluation of SPNs, in which other imaging modalities have raised suspicion of lung cancer (P) compared with an evaluation without PET-CT (C)?
As described, we identified 14 original papers addressing this issue, of which three had evidence level 1b [26–28] and 11 had evidence level 2b [29–39]) for various types of SPN. The materials were not directly comparable, but the studies provided a broader picture of the applicability of PET and PET-CT in different types of SPN (including varying size, risk profile, and density).
Situations in which PET-CT was found useful
When excluding patients with small or non-solid SPNs, all studies included in the review demonstrated that PET and PET-CT had a sensitivity of 88 % to 100 %. The retrospective study of Jeong et al. [38] reported a sensitivity of 88 % of PET-CT for the detection of malignancy, but further analysis revealed that the false-negative findings in this study (that resulted in a sensitivity of “only” 88 %) were often due to non-solid SPNs or bronchoalveolar carcinoma (BAC). An example was a retrospective investigation by Yi et al. [29] that analysed 119 patients who underwent PET-CT to classify an unclarified SPN. This paper reported a sensitivity of 96 %, which is in line with the majority of studies published and is higher than the sensitivity of 81 % they found for CT.
Special tumours
In 2002, Heynemann et al. [30] and Yap et al. [31] did retrospective reviews of PET scans in a total of 56 patients with proven BAC, today classified as a subtype of adenocarcinoma. They found that PET had a low sensitivity for both BAC and ground glass opacities (GGO) (sensitivity of 38 % and 33 %, respectively). In 2004, Nomori et al. [28] demonstrated a very low sensitivity of PET to detect malignancy of around 20 % for GGOs in a prospective study involving a total of 131 patients. In the same manner, in 2007 Daniels et al. [34] did a retrospective review of 16 patients with pulmonary carcinoid tumour and found a sensitivity of 75 % for PET to detect malignancy.
Small SPNs
There are vast differences between reported findings in small SPNs (typically defined as <1 cm). The study by Nomori et al. [28] described above demonstrated a sensitivity of 0 % using PET, in contrast to a study by Herder et al., who in a retrospective analysis of 35 patients with small tumours (<1 cm) found a sensitivity of 93 % [35]. The two studies differ in the way that an SPN is defined as PET-positive, which could explain some of the different findings. Herder et al. visually compared the SPN uptake with mediastinal blood pool (as we do in our PET centres) while Nomori et al. calculated a contrast ratio comparing highest activity in the SPN (T = tumour) with the contralateral lung (N = normal). They considered the SPN to be FDG-positive if (T-N)/(T + N) ≥ 0.,4 or in other words, if the SPN’s FDG uptake was more than ∼2.3 times higher than the contralateral lung.
Can PET-CT prevent futile curative-intent treatment trials by revealing occult metastasis?
To answer this, we asked the following PICO-question: “What is the effect of the routine use of PET-CT (I) in patients with lung cancer, in whom curative-intent treatment is planned (P), on the number of futile curative-intent treatment trials (O), compared to an evaluation without PET-CT (C)?”
Our review identified nine original papers on this issue (eight with evidence level 1b [40–47], one with evidence level 2b [48]). These papers typically examined the value of adding PET-CT to standard investigations before treatment, when no obvious metastasis was detected. However, study designs were heterogeneous, focusing primarily on the use of PET-CT before surgery and to a lesser extent before curative-intent oncological treatment.
The studies used different control arms including different “standard investigations”. Some studies demonstrated a reduced number of futile or non-curative thoracotomies. In 2008, Kozower et al. [41] demonstrated this in 122 patients in a prospective design. PET prevented more non-therapeutic thoracotomies in stage IA, compared to standard testing with CT of the chest and upper abdomen, bone scintigraphy, and brain imaging. This reduction was even greater in prospective studies of Reed et al. [46] and Fischer et al. [44] from 2003 and 2009, respectively. They enrolled a total of 492 patients and compared PET and PET-CT with standard investigation (CT of chest and upper abdomen, bone scintigraphy, and brain imaging in the study by Reed et al., and CT of the chest and abdomen, and bronchoscopy in the study by Fischer et al.) before surgery. They found a significantly lower rate of futile thoracotomies in the PET-CT group and that one in five thoracotomies could be avoided.
In 2001, MacManus et al. [45] did a prospective investigation of 167 patients in whom curative-intent chemo- and radiotherapy were planned. By adding PET they uncovered distant metastasis not found by CT of the chest and abdomen or by bone scintigraphy in 32 of these patients, which altered their management.
A large prospective study by Herder et al. [40] from 2006 did not show any reduction in the number of futile thoracotomies. This group studied 465 patients (of whom half were randomized to PET), who were evaluated on suspicion of lung cancer. The primary aim was not to show reduction in futile thoracotomies, but to test if PET could reduce the total number of tests and procedures used for staging and definition of operability. They did not find a significant reduction in the total number of diagnostic tests with PET, but a significant reduction in the need of surgical staging and need of general anaesthesia.
The study by Viney et al. [42] was a prospective, randomized study of 184 patients with presumed stage I and II lung cancer, who did not undergo routine invasive mediastinal staging before treatment. In this study, no significant reduction in futile thoracotomies was demonstrated, but PET changed the presumed clinical stage in 20 % of cases.
Can PET-CT reliably detect or exclude mediastinal and hilar lymph node metastasis and thereby prevent surgical or endoscopic mediastinal staging?
To answer this, a third PICO-question was constructed: “What is the effect of adding PET-CT (I) as compared to CT alone (C) on the number of inappropriate/unnecessary invasive tests (O) in patients with suspected or confirmed lung cancer, who are undergoing invasive examination for diagnosis or staging (P)?”
Our review identified 18 original works on this subject (nine with evidence level 1b [27, 40, 49–55], eight with evidence level 2b [56–63], and one with evidence level 2c [64]). These were primarily papers in two categories: studies dealing with PET and PET-CT in the evaluation of the mediastinum (nine articles) and for categorization of changes in the adrenal glands (five articles). Below, and in Table 1, we primarily considered articles on mediastinal staging.
The results of these studies were very homogenous. They all provided evidence that the sensitivity of PET and PET-CT for the detection of mediastinal dissemination was insufficient with regard to ruling this out. As an example, in 2011 Darling et al. [50] reported a prospective study analyzing 149 patients with proven non-small-cell lung cancer that was presumed to be operable. However, with mediastinoscopy and/or surgery as reference, they found a sensitivity of 70 % with PET-CT for the detection of N2/N3 disease.
However, even though it is evident from the literature that PET-CT is in general insufficient with regard to ruling out mediastinal dissemination, there were a number of papers suggesting that small tumours, without evidence of lymph node dissemination on CT or PET-CT, can reasonably undergo surgery without invasive staging. This was, for instance, demonstrated by Lee et al. [64] in their paper from 2007, in which they reported a retrospective analysis of 224 patients who underwent CT of the chest and abdomen and PET. With mediastinoscopy and surgery as reference, they found occult N2 disease in only three of 103 (2.9 %) patients with small, peripherally located tumours as opposed to five of 20 (25 %) patients with large, centrally located tumours.
Discussion
Lung cancer is one of the most frequent cancers in the industrialized world, with an overall 5-year survival of only 17 %. When diagnosed in early stages, surgical/oncological curative-intent treatment may increase this rate to >50 % [16]. It is likely that prolonged evaluation time is critical, especially in low-stage disease [65]. In our experience, the diagnosis is confirmed in one of three patients referred for suspected lung cancer, a rate that is probably highly dependent on local referral practices.
Considerations like these have in Denmark lead to national integrated cancer pathways for a number of cancers, to reduce referral time and obtain faster diagnosis and more rapid onset of treatment in agreement with national guidelines. The lung cancer pathway typically lasts two weeks from referral until pathology results and a multidisciplinary team decision are available. The program typically consists of clinical examination, pulmonary function testing (ventilation- and diffusion capacity), chest and abdominal CT (day 1), PET-CT (day 2), endobronchial ultrasonography (EBUS), and endoscopic oesophageal ultrasound (EUS) to stage the mediastinum (days 3–5), regional lung scintigraphy to estimate post-operative lung function (day 6), and CT-guided biopsy (day 7).
In our setting, PET-CT serves as a gatekeeper. Firstly, if PET-CT is negative, invasive testing is omitted, and the patient is enrolled in a follow-up program. Secondly, if PET-CT does not reveal extra-thoracic metastasis the patient will undergo surgery or other curative-intent treatments after invasive staging of the mediastinum. Except in cases of overwhelming metastatic disease, we confirm PET-CT-positive findings by biopsy before the patient is considered incurable.
This multi-modality programme is demanding for fragile patients, expenses are high, and logistics challenging. Based on this background, the health care directorate of the region wanted to know if the extensive use of diagnostic modalities, including PET-CT, was well-founded.
The SPN issue
The present literature review supports the extensive use of PET-CT, as a considerable number of percutaneous biopsies can be avoided in the case of PET-CT-negative SPN. This has three important clinical implications. Firstly, percutaneous lung biopsy has a high complication rate with a risk of pneumothorax of 20 % [66, 67]. Not all these patients require chest tube insertion, but a pneumothorax delays further investigation. Therefore, at our institution all other examinations are normally performed before percutaneous biopsy. Secondly, biopsy and other diagnostic procedures performed before malignant SPN has been ruled out represent superfluous risks and incremental costs, which can be omitted with a negative PET-CT. Thirdly, the patient is spared a lot of anxiety if up-front PET-CT has ruled out malignancy.
Small SPNs remain a diagnostic challenge due to the physical characteristic of PET-CT scanners. Both the studies [28, 35] looking at small SPNs were older studies from 2004 using PET scanners without CT attenuation correction and a spatial resolution of 7 mm, making it difficult to detect small lesions. Although modern techniques have reduced the problems of partial volume effect and respiratory motion [68–70], they will never completely disappear, and these patients should be recognized by an appropriate follow-up program like the ones suggested by the Fleischner Society [71, 72]. These follow-up programs are also appropriate in cases of GGO nodules and part-solid nodules, in which possible diagnoses such as BAC should be suspected. However, as metastases from some tumours, such as gastrointestinal malignancy, are known to occasionally present as GGO, we tend to biopsy these abnormalities in patients with a history of adenocarcinoma [73].
The issue of futile thoracotomy and other curative-intent treatment trials
It is well-known that a significant number of patients undergoing surgery for lung cancer do in fact have occult disseminated disease. These patients will primarily suffer side effects and complications from curative-intent treatment trials, and since no benefit is obvious, the number of cases of so-called futile treatment trials should be reduced as much as possible.
PET-CT should be considered mandatory before curative-intent treatment trials, as around 20 % will otherwise undergo futile treatments primarily due to unrecognized distant metastases. The reviewed studies have not shown mortality benefit from PET-CT in this regard, but as the in-hospital mortality after pneumonectomy is >5 % (lesser for lobectomy and segmentectomy), a reduction in surgery must rationally bear a mortality benefit [74]. In addition, the patients are spared the morbidity associated with thoracotomy and disadvantages from delay in radio- or chemotherapy that inappropriate surgery inevitably leads to. An example of this is seen in Fig. 3.
The depicted patient was diagnosed with a non-small-cell lung cancer by bronchoscopy and EBUS. No signs of distant metastases were found on CT of the chest and abdomen, or in the biochemical analysis. However, PET-CT detected multiple bone metastases. This changed the treatment from curative-intent to palliative
The issue of mediastinal staging
The outcome measure, i.e., the reduction in invasive mediastinal staging procedures, was chosen based on the assumption that the reduction in the number of invasive tests, such as EBUS, EUS, and mediastinoscopy would shorten the workup time and reduce the morbidity associated with invasive testing and general anaesthesia.
The conclusion in the vast majority of included studies was that PET-CT is in most patients not suitable for verification or exclusion of mediastinal dissemination, although this is a rare finding in patients with a small peripheral primary tumour without enlarged lymph nodes on CT or metabolic active glands on PET-CT. In contrast to the well-documented uses of PET-CT described above, this modality may not be sensitive enough to rule out lymph node dissemination, except in cases of small peripheral tumours. An example of this is seen in Fig. 4.
The patient illustrated presented with refractory hyponatremia, and CT and PET-CT revealed a metabolic active tumour of 2.8 cm in the middle lobe, and on CT enlarged lymph nodes at stations 11R and 4R were found. PET-CT was positive at station 11R in addition to the tumour. No FDG-accumulation was seen in stations 4R and 7, but EBUS and EUS were positive for malignancy in stations 11R, 4R, and 7. The TNM classification based on CT and PET–CT was T1bN1M0, but this was changed to T1bN2M0 after EBUS and EUS. This has significant clinical implications, as the treatment was changed from primary surgery to curative-intent chemo- and radiotherapy
Although not the primary focus of this review, it seems appropriate to recall that a PET-CT image alone is not sufficient to make a diagnosis of malignancy and that all positive PET-CT findings should in general be proven by cytology or histology. A pragmatic exception is the patient with overwhelming dissemination on imaging. No patient should be considered incurable if only one or a few PET-CT-positive foci are present, as many non-malignant conditions (like infection, sarcoidosis, and tuberculosis) are known to be PET-CT-positive. In addition, PET-CT should ideally be performed before any interventions like biopsy, EBUS, and surgery, as these procedures may cause false-positive PET-CT findings [75]. This is another reason why in our setting PET-CT is performed up-front before any invasive testing.
Limitations
This article is not a systematic review in the strictest sense. Our focus was on already known and reviewed knowledge in the clinical practice and its context. The literature search was comprehensive and comprised most large biomedical databases, but non-English and non-Scandinavian articles were excluded, and we did not re-evaluate all background literature for systematic reviews and meta-analyses. Due to time restrictions, we chose the REA methodology for reviewing reviews and extracting relevant articles for our purpose and, thus, cannot exclude that we may have missed some relevant papers. Nonetheless, we feel that it is unlikely that this would significantly have changed the conclusions we have reached.
Our literature search was conducted in late 2013, leaving out potentially important papers from 2014 onwards. However, an additional search conducted shortly before this article was written, did not reveal articles that changed our conclusions. On the contrary, published work supports these [76–79]. The sorting of retrieved papers was undertaken by one author only (PHM) instead of two, and, in accordance with the REA methodology, with only a simple quality appraisal [19]. This may introduce selection bias, because potentially relevant articles may more easily be discarded than when this decision is made by consensus.
Perspective
The review has now served as a basis for the standardization of the use of PET-CT in lung cancer in the Region of Southern Denmark [2].
It would be rational to test the use of up-front PET-CT in the evaluation of lung cancer in a setting where PET-CT is not used routinely. The primary outcomes of the study should be the numbers of (1) avoided invasive testing and associated complications, (2) avoided futile treatment trials, and (3) missed malignant diagnoses.
One problem reinforced by the use of PET-CT is the number of false-positive findings, which has at least four negative implications. One is the worry of the patient until malignancy has been ruled out. Another is that a false-positive finding can sometimes remove focus from the actual disease, e.g., if PET-CT raises suspicion of a secondary cancer. Prolongation of the evaluation process is a third drawback, and a fourth is the incremental cost and risk associated with additional testing. However, studies suggest that such unexpected findings do, in fact, in a considerable number of cases represent malignant or premalignant lesions. This has found to be the case in 21 %, 33 %, 45 %, and 65 % of incidental PET or PET-CT findings in head/neck, thyroid, breast, and colon cancers, respectively [80–84]. How this dilemma is best managed clinically is not settled, but in our practice we investigate all incidental findings that are not obviously physiological.
In conclusion
F-18 PET-CT is an appropriate imaging modality in most patients with suspected or proven lung cancer and should be considered a routine investigation in this setting. The present review provides the basis for the following specific statements: (1) SPNs can safely be considered benign if PET-CT is negative, except in SPNs <1 cm and in non-solid SPNs (recommendation A); (2) No curative-intent treatment (e.g. surgery) should be commenced until a PET-CT scan has excluded occult distant metastasis (recommendation A); (3) In general, lymph node metastasis in the mediastinum cannot be ruled out on basis of a negative PET-CT (recommendation A). Therefore, invasive staging by EBUS and/or EUS and/or mediastinoscopy should be performed in most patients before curative-intent treatment trials, regardless of mediastinal PET-CT findings.
References
Han Y, Xiao H, Zhou Z, Yuan M, Zeng Y, Wu H, et al. Cost-effectiveness analysis of strategies introducing integrated 18F-FDG PET/CT into the mediastinal lymph node staging of non-small-cell lung cancer. Nucl Med Commun. 2015;36:234–41.
Region Syddanmark. PET/CT i Region Syddanmark. http://ipaper.ipapercms.dk/RegionSyddanmark/OUH/Stabsafdelinger/Afdelingen_for_Kvalitet_og_Forskning___MTV/140519_PETCT_Undergruppens_afrapportering_Samlet_v4/. Date last updated: April 2014. Date last assessed: February 9 2015.
Stevens AN. Development of PET in Western Europe (abstract OP 104). Eur J Nucl Med Mol Imaging. 2013;40 Suppl 2:S1–477.
Kotzerke J, Oehme L, Grosse J, Hellwig D. Positron emission tomography 2013 in Germany. Results of the query and current status. Nuklearmedizin. 2015;54(2).
Dansk Lunge Cancer Gruppe. Lungecancer: Visitation, diagnose & stadieinddeling. www.lungecancer.dk. Date last updated: January 21 2015. Date last assessed: February 9 2015.
National Institute for Health and Care Excellence. Lung cancer: Diagnosis and treatment. https://www.nice.org.uk/guidance/cg121. Date last updated: April 2011. Date last assessed February 9 1015.
National Comprehensive Cancer Network. Non-small cell lung cancer. http://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Date last updated: April 2014. Date last assessed: February 9 2015.
European Respiratory Society. http://www.ers-education.org/guidelines.aspx. Date last updated: not available. Date last assessed: February 10 2015.
Gould MK, Donington J, Lynch WR, Mazzone PJ, Midthun DE, Naidich DP, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e93S–120.
Colt HG, Murgu SD, Korst RJ, Slatore CG, Unger M, Quadrelli S. Follow-up and surveillance of the patient with lung cancer after curative-intent therapy: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e437S–54.
Silvestri GA, Gonzalez AV, Jantz MA, Margolis ML, Gould MK, Tanoue LT, et al. Methods for staging non-small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e211S–50.
Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e142S–65.
De Leyn P, Dooms C, Kuzdzal J, Lardinois D, Passlick B, Rami-Porta R, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg. 2014;45:787–98.
Peters S, Adjei AA, Gridelli C, Reck M, Kerr K, Felip E, et al. Metastatic non-small-cell lung cancer (NSCLC): ESMO Clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23:vii56–64.
Vansteenkiste J, De Ruysscher D, Eberhardt WE, Lim E, Senan S, Felip E, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24:vi89–98.
American Cancer Society. Cancer facts and figures 2014. www.cancer.org/acs/groups/content/@research/documents/webcontent/acspc-042151.pdf. Date last updated: 2014. Date last assessed: February 9 2015.
Cook DJ, Mulrow CD, Haynes RB. Systematic reviews: synthesis of best evidence for clinical decisions. Ann Intern Med. 1997;126(5):376–80.
Centre for Evidence Based Medicine. Finding the evidence 1 – Using PICO to formulate a search question. http://www.cebm.net/finding-the-evidence-1-using-pico-to-formulate-a-search-question/. Date last updated: 2014. Date last assessed: February 9 2015.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108.
Khangura S, Konnyu K, Cushman R, Grimshaw J, Moher D. Evidence summaries: the evolution of a rapid review approach. Syst Rev. 2012;1:10.
Khangura S, Polisena J, Clifford TJ, Farrah K, Kamel C. Rapid review: an emerging approach to evidence synthesis in health technology assessment. Int J Technol Assess Health Care. 2014;30(1):20–7.
Varker T, Forbes D, Dell L, Weston A, Merlin T, Hodson S, et al. Rapid evidence assessment: increasing the transparency of an emerging methodology. J Eval Clin Pract. 2015 [E-pub ahead of print].
Civil Service. What is a rapid evidence assesement? http://www.civilservice.gov.uk/networks/gsr/resources-and-guidance/rapid-evidence-assessment/what-is. Date last updated: N/A. Date last assessed: July 29 2015.
Facey K, Bradbury I, Laking G, Payne E. Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers. Health Technol Assess. 2007;11(44):iii-iv, xi-267.
Centre for Evidence Based Medicine. Oxford Centre for Evidence-based Medicine – Levels of evidence (March 2009). http://www.cebm.net/index.aspx?o=1025. Date last updated: 2014. Date last assessed: February 9 2015.
Fletcher JW, Kymes SM, Gould M, Alazraki N, Coleman RE, Lowe VJ, et al. A comparison of the diagnostic accuracy of 18F-FDG PET and CT in the characterization of solitary pulmonary nodules. J Nucl Med. 2008;49:179–85.
Harders SW. LUCIS: lung cancer imaging studies. DMJ. 2012;59(11):B4542.
Nomori H, Watanabe K, Ohtsuka T, Naruke T, Suemasu K, Uno K. Evaluation of F-18 fluorodeoxyglucose (FDG) PET scanning for pulmonary nodules less than 3 cm in diameter, with special reference to the CT images. Lung Cancer. 2004;45:19–27.
Yi CA, Lee KS, Kim BT, Choi JY, Kwon OJ, Kim H, et al. Tissue characterization of solitary pulmonary nodule: comparative study between helical dynamic CT and integrated PET/CT. J Nucl Med. 2006;47:443–50.
Heyneman LE, Patz EF. PET imaging in patients with bronchioloalveolar cell carcinoma. Lung Cancer. 2002;38:261–6.
Yap CS, Schiepers C, Fishbein MC, Phelps ME, Czernin J. FDG-PET imaging in lung cancer: how sensitive is it for bronchioloalveolar carcinoma? Eur J Nucl Med. 2002;29:1166–73.
Christensen JA, Nathan MA, Mullan BP, Hartman TE, Swensen SJ, Lowe VJ. Characterization of the solitary pulmonary nodule: 18F-FDG PET versus nodule-enhancement CT. AJM Am J Roentgenol. 2006;187:1361–7.
Kagna O, Solomonov A, Keidar Z, Bar-Shalom R, Fruchter O, Yigla M, et al. The value of FDG-PET/CT in assessing single pulmonary nodules in patients at high risk of lung cancer. Eur J Nucl Med Mol Imaging. 2009;36:997–1004.
Daniels CE, Lowe VJ, Aubry MC, Allen MS, Jett JR. The utility of fluorodeoxyglucose positron emission tomography in the evaluation of carcinoid tumors presenting as pulmonary nodules. Chest. 2007;131:255–60.
Herder GJ, Golding RP, Hoekstra OS, Comans EF, Teule GJ, Postmus PE, et al. The performance of (18)F-fluorodeoxyglucose positron emission tomography in small solitary pulmonary nodules. Eur J Nucl Med Mol Imaging. 2004;31:1231–6.
Bar-Shalom R, Kagna O, Israel O, Guralnik L. Noninvasive diagnosis of solitary pulmonary lesions in cancer patients based on 2-fluoro-2-deoxy-D-glucose avidity on positron emission tomography/computed tomography. Cancer. 2008;113:3213–21.
Kim SK, Allen-Auerbach M, Goldin J, Fueger BJ, Dahlbom M, Brown M, et al. Accuracy of PET/CT in characterization of solitary pulmonary lesions. J Nucl Med. 2007;48:214–20.
Jeong SY, Lee KS, Shin KM, Bae YA, Kim BT, Choe BK, et al. Efficacy of PET/CT in the characterization of solid or partly solid solitary pulmonary nodules. Lung Cancer. 2008;61:186–94.
Dewan NA, Reeb SD, Gupta NC, Gobar LS, Scott WJ. PET-FDG imaging and transthoracic needle lung aspiration biopsy in evaluation of pulmonary lesions. A comparative risk-benefit analysis. Chest. 1995;108:441–6.
Herder GJ, Kramer H, Hoekstra OS, Smit EF, Pruim J, van Tinteren H, et al. Traditional versus up-front [18F] fluorodeoxyglucose-positron emission tomography staging of non-small-cell lung cancer: a Dutch cooperative randomized study. J Clin Oncol. 2006;24:1800–6.
Kozower BD, Meyers BF, Reed CE, Jones DR, Decker PA, Putnam Jr JB. Does positron emission tomography prevent nontherapeutic pulmonary resections for clinical stage IA lung cancer? Ann Thoracic Surg. 2008;85:1166–70.
Viney RC, Boyer MJ, King MT, Kenny PM, Pollicino CA, McLean JM, et al. Randomized controlled trial of the role of positron emission tomography in the management of stage I and II non-small-cell lung cancer. J Clin Oncol. 2004;22:2357–62.
Maziak DE, Darling GE, Inculet RI, Gulenchyn KY, Driedger AA, Ung YC, et al. Positron emission tomography in staging early lung cancer: a randomized trial. Ann Intern Med. 2009;151:221–8.
Fischer B, Lassen U, Mortensen J, Larsen S, Loft A, Bertelsen A, et al. Preoperative staging of lung cancer with combined PET-CT. New Engl J Med. 2009;361:32–9.
MacManus MP, Hicks RJ, Matthews JP, Hogg A, McKenzie AF, Wirth A, et al. High rate of detection of unsuspected distant metastases by pet in apparent stage III non-small-cell lung cancer: implications for radical radiation therapy. Int J Radiat Oncology Biol Phys. 2001;50:287–93.
Reed CE, Harpole DH, Posther KE, Woolson SL, Downey RJ, Meyers BF, et al. Results of the American College of Surgeons Oncology Group Z0050 trial: the utility of positron emission tomography in staging potentially operable non-small cell lung cancer. J Thoracic Cardiovasc Surg. 2003;126:1943–51.
Lardinois D, Weder W, Hany TF, Kamel EM, Korom S, Seifert B, et al. Staging of non-small-cell lung cancer with integrated positron-emission tomography and computed tomography. New Engl J Med. 2003;348:2500–7.
De Wever W, Ceyssens S, Mortelmans L, Stroobants S, Marchal G, Bogaert J, et al. Additional value of PET-CT in the staging of lung cancer: comparison with CT alone, PET alone and visual correlation of PET and CT. Eur Radiol. 2007;17:23–32.
Lardinois D, Weder W, Roudas M, von Schulthess GK, Tutic M, Moch H, et al. Etiology of solitary extrapulmonary positron emission tomography and computed tomography findings in patients with lung cancer. J Clin Oncol. 2005;23:6846–53.
Darling GE, Maziak DE, Inculet RI, Gulenchyn KY, Driedger AA, Ung YC, et al. Positron emission tomography-computed tomography compared with invasive mediastinal staging in non-small cell lung cancer: results of mediastinal staging in the early lung positron emission tomography trial. J Thorac Oncol. 2011;6:1367–72.
Herth FJ, Eberhardt R, Krasnik M, Ernst A. Endobronchial ultrasound-guided transbronchial needle aspiration of lymph nodes in the radiologically and positron emission tomography-normal mediastinum in patients with lung cancer. Chest. 2008;133:887–91.
Fischer BM, Mortensen J, Hansen H, Vilmann P, Larsen SS, Loft A, et al. Multimodality approach to mediastinal staging in non-small cell lung cancer. Faults and benefits of PET-CT: a randomised trial. Thorax. 2011;66:294–300.
Bryant AS, Cerfolio RJ, Klemm KM, Ojha B. Maximum standard uptake value of mediastinal lymph nodes on integrated FDG-PET-CT predicts pathology in patients with non-small cell lung cancer. Ann Thoracic Surg. 2006;82:417–22.
Cerfolio RJ, Bryant AS, Eloubeidi MA. Routine mediastinoscopy and esophageal ultrasound fine-needle aspiration in patients with non-small cell lung cancer who are clinically N2 negative: a prospective study. Chest. 2006;130(6):1791–5.
Shim SS, Lee KS, Kim BT, Chung MJ, Lee EJ, Han J, et al. Non-small cell lung cancer: prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology. 2005;236:1011–9.
Gonzalez-Stawinski GV, Lemaire A, Merchant F, O’Halloran E, Coleman RE, Harpole DH, et al. A comparative analysis of positron emission tomography and mediastinoscopy in staging non-small cell lung cancer. J Thoracic Cardiovasc Surg. 2003;126:1900–5.
Stroobants SG, D’Hoore I, Dooms C, De Leyn PR, Dupont PJ, De Wever W, et al. Additional value of whole-body fluorodeoxyglucose positron emission tomography in the detection of distant metastases of non-small-cell lung cancer. Clin Lung Cancer. 2003;4:242–7.
Lu Y, Xie D, Huang W, Gong H, Yu J. 18F-FDG PET/CT in the evaluation of adrenal masses in lung cancer patients. Neoplasma. 2010;57:129–34.
Ozcan Kara P, Kara T, Kara Gedik G, Kara F, Sahin O, Ceylan Gunay E, et al. The role of fluorodeoxyglucose-positron emission tomography/computed tomography in differentiating between benign and malignant adrenal lesions. Nucl Med Commun. 2011;32:106–12.
Al-Sarraf N, Aziz R, Gately K, Lucey J, Wilson L, McGovern E, et al. Pattern and predictors of occult mediastinal lymph node involvement in non-small cell lung cancer patients with negative mediastinal uptake on positron emission tomography. Eur J Cardio Thoracic Surg. 2008;33:104–9.
Kumar R, Xiu Y, Yu JQ, Takalkar A, El-Haddad G, Potenta S, et al. 18F 18F-FDG PET in evaluation of adrenal lesions in patients with lung cancer. J Nucl Med. 2004;45:2058–62.
Metser U, Miller E, Lerman H, Lievshitz G, Avital S, Even-Sapir E. 18F-FDG PET/CT in the evaluation of adrenal masses. J Nucl Med. 2006;47:32–7.
Gupta NC, Graeber GM, Tamim WJ, Rogers JS, Irisari L, Bishop HA. Clinical utility of PET-FDG imaging in differentiation of benign from malignant adrenal masses in lung cancer. Clin Lung Cancer. 2001;3:59–64.
Lee PC, Port JL, Korst RJ, Liss Y, Meherally DN, Altorki NK. Risk factors for occult mediastinal metastases in clinical stage I non-small cell lung cancer. Ann Thorac Surg. 2007;84:177–81.
Salomaa ER, Sallinen S, Hiekkaen H, Liippo K. Delays in the diagnosis and treatment of lung cancer. Chest. 2005;128:2282–8.
Kim JI, Park CM, Lee SM, Goo JM. Rapid needle-out patient-rollover approach after cone beam CT-guided lung biopsy: effect on pneumothorax rate in 1,191 consecutive patients. Eur Radiol. 2015;25:1845–53.
Boskovic T, Stanic J, Pena-Karan S, Zarogoulidis P, Drevelegas K, Katsikogiannis N, et al. Pneumothorax after transthoracic needle biopsy of lung lesions under CT guidance. J Thorac Dis. 2014;6:S99–107.
Soret M, Bacharach SL, Buvat I. Partial-volume effect in PET tumor imaging. J Nucl Med. 2007;48(6):932–45.
Hoetjes NJ, van Velden FHP, Hoekstra OS, Hoekstra CJ, Krak NC, Lammertsma AA, et al. Partial volume correction strategies for quantitative FDG PET in oncology. Eur J Nucl Med Mol Imaging. 2010;37(9):1679–87.
Salavati A, Borofsky S, Boon-Keng TK, Houshmand S, Khiewvan B, Saboury B, et al. Application of partial volume effect correction and 4D PET in the quantification of FDG avid lung lesions. Mol Imaging Biol. 2015;17(1):140–8.
Naidich DP, Bankier AA, MacMahon H, Schaefer-Prokop CM, Pistolesi M, Goo JM, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013;266:304–17.
MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237:395–400.
Gaeta M, Volta S, Scribano E, Loria G, Vallone A, Pandolfo I. Air-space pattern in lung metastasis from adenocarcinoma of the GI tract. J Comput Assist Tomogr. 1996;2:300–4.
Watanabe S, Asamura H, Suzuki K, Tsuchiya R. Recent results of postoperative mortality for surgical resections in lung cancer. Ann Thorac Surg. 2004;7:999–1002.
Truong MT, Pan T, Erasmus JJ. Pitfalls in integrated CT-PET of the thorax: implications in oncologic imaging. J Thorac Imaging. 2006;21:111–22.
Smoragiewicz M, Laskin J, Wilson D, Ramsden K, Yee J, Lam S, et al. Using pet-ct to reduce futile thoracotomy rates in non-small-cell lung cancer: a population-based review. Curr Oncol. 2014;21(6):e768–74.
Halaç M, Özhan M, Yilmaz Aksoy S, Vatankulu B, Aliyev A, Asa S, et al. The role of FDG-PET/CT in detecting unsuspected and unknown distant metastasis in the initial staging of NSCLC. Turk J Med Sci. 2014;44(6):1029–40.
Dalli A, Selimoglu Sen H, Coskunsel M, Komek H, Abakay O, Sergi C, et al. Diagnostic value of PET/CT in differentiating benign from malignant solitary pulmonary nodules. J BUON. 2013;18(4):935–41.
Harders SW, Madsen HH, Hjorthaug K, Arveschoug AK, Rasmussen TR, Meldgaard P, et al. Mediastinal staging in non-small-cell lung carcinoma: computed tomography versus F-18-fluorodeoxyglucose positron-emission tomography and computed tomography. Cancer Imaging. 2014;14:23.
Al-Hakami HA, Makis W, Anand S, Mlynarek A, Black MJ, Stern J, et al. Head and neck incidentalomas on positron emission tomographic scanning: ignore or investigate? J Otolaryngol Head Neck Surg. 2011;40:384–90.
Shie P, Cardarelli R, Sprawls K, Fulda KG, Taur A. Systematic review: prevalence of malignant incidental thyroid nodules identified on fluorine-18 fluorodeoxyglucose positron emission tomography. Nucl Med Commun. 2009;30:742–8.
Chae EY, Cha JH, Kim HH, Shin HJ, Kim HJ, Oh HY, et al. Analysis of incidental focal hypermetabolic uptake in the breast as detected by 18F-FDG PET/CT: clinical significance and differential diagnosis. Acta Radiol. 2012;53:530–5.
Treglia G, Calcagni ML, Rufini V, Leccisotti L, Meduri GM, Spitilli MG, et al. Clinical significance of incidental focal colorectal 18F-fluorodeoxyglucose uptake: our experience and a review of the literature. Colorectal Dis. 2011;14:174–80.
Hess S, Blomberg BA, Zhu HJ, Høilund-Carlsen PF, Alavi A. The pivotal role of FDG-PET/CT in modern medicine. Acad Radiol. 2014;21:232–49.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
PHM has received personal fees from the Region of Southern Denmark, Intermune, Sandoz and Astra-Zeneca. PHM has received travel grants from Norpharma, Intermune, Olympus, and Sandoz. JBC has received personal fees from the Region of Southern Denmark. PCH and PFHC have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not relevant.
Appendix: search terms
Appendix: search terms
Lung cancer synonyms:
-
Bronchogenic Carcinoma
-
Bronchogenic Carcinomas
-
Bronchial Carcinoma
-
Bronchial Carcinomas
-
Small Cell Lung Cancer
-
Small Cell Lung Cancers
-
Small Cell Lung Neoplasm
-
Small Cell Lung Neoplasms
-
Small Cell Lung Carcinoma
-
Small Cell Lung Carcinomas
-
Small Cell Lung Tumor
-
Small Cell Lung Tumors
-
Small Cell Lung Tumour
-
Small Cell Lung Tumours
-
Small-Cell Lung Cancer
-
Small-Cell Lung Cancers
-
Small-Cell Lung Neoplasm
-
Small-Cell Lung Neoplasms
-
Small-Cell Lung Carcinoma
-
Small-Cell Lung Carcinomas
-
Small-Cell Lung Tumor
-
Small-Cell Lung Tumors
-
Small-Cell Lung Tumour
-
Small-Cell Lung Tumours
-
Oat Cell Lung Cancer
-
Oat Cell Lung Cancers
-
Oat Cell Lung Neoplasm
-
Oat Cell Lung Neoplasms
-
Oat Cell Lung Carcinoma
-
Oat Cell Lung Carcinomas
-
Oat Cell Lung Tumor
-
Oat Cell Lung Tumors
-
Oat Cell Lung Tumors
-
Oat Cell Lung Tumour
-
Oat Cell Lung Tumours
-
Oat-Cell Lung Cancer
-
Oat-Cell Lung Cancers
-
Oat-Cell Lung Neoplasm
-
Oat-Cell Lung Neoplasms
-
Oat-Cell Lung Carcinoma
-
Oat-Cell Lung Carcinomas
-
Oat-Cell Lung Tumor
-
Oat-Cell Lung Tumors
-
Oat-Cell Lung Tumors
-
Oat-Cell Lung Tumour
-
Oat-Cell Lung Tumours
-
SCLC
-
Non Small Cell Lung Carcinoma
-
Non Small Cell Lung Carcinomas
-
Non Small Cell Lung Cancer
-
Non Small Cell Lung Cancers
-
Non Small Cell Lung Neoplasm
-
Non Small Cell Lung Neoplasms
-
Non Small Cell Lung Tumor
-
Non Small Cell Lung Tumors
-
Non Small Cell Lung Tumour
-
Non Small Cell Lung Tumours
-
Non-Small-Cell Lung Carcinoma
-
Non-Small-Cell Lung Carcinomas
-
Non-Small-Cell Lung Cancer
-
Non-Small-Cell Lung Cancers
-
Non-Small-Cell Lung Neoplasm
-
Non-Small-Cell Lung Neoplasms
-
Non-Small-Cell Lung Tumor
-
Non-Small-Cell Lung Tumors
-
Non-Small-Cell Lung Tumour
-
Non-Small-Cell Lung Tumours
-
Nonsmall Cell Lung Cancer
-
Nonsmall Cell Lung Cancers
-
Nonsmall Cell Lung Carcinoma
-
Nonsmall Cell Lung Carcinomas
-
NonSmall Cell Lung Neoplasm
-
NonSmall Cell Lung Neoplasms
-
NonSmall Cell Lung Tumor
-
NonSmall Cell Lung Tumors
-
NonSmall Cell Lung Tumour
-
NonSmall Cell Lung Tumours
-
Non-Small Cell Lung Carcinoma
-
Non-Small Cell Lung Carcinomas
-
Non-Small Cell Lung Cancer
-
Non-Small Cell Lung Cancers
-
Non-Small Cell Lung Neoplasm
-
Non-Small Cell Lung Neoplasms
-
Non-Small Cell Lung Tumor
-
Non-Small Cell Lung Tumors
-
Non-Small Cell Lung Tumour
-
Non-Small Cell Lung Tumours
-
NSCLC
PET synonyms:
-
Positron Emission Tomography and Computed Tomography
-
X-Ray Computed Tomography and Positron-Emission Tomography
-
X Ray Computed Tomography and Positron Emission Tomography
-
PET and CT
-
Hybrid Pet and CT
-
Integrated PET CT
-
Positron Emission Tomography
-
PET Scan
-
PET Scans
-
Positron-Emission Tomography
-
“Positron Emission Tomographies”
-
“Positron Emission Tomographic”
-
“PET” AND “CT”
-
PET/CT
-
PET
-
“petscan”
-
“petscans”
-
“petscanning”
-
“pet scanning”
-
Fluorodeoxyglucose F18
-
Fluorodeoxy Glucose
-
Fludeoxyglucose F18
-
Fluorodeoxyglucose F 18
-
Fludeoxyglucose F 18
-
Fluorine-18-fluorodeoxyglucose
-
Fluorine 18 fluorodeoxyglucose
-
Fluorine-18-Fludeoxyglucose
-
Fluorine 18 Fludeoxyglucose
-
18F Fludeoxyglucose
-
18-F Fludeoxyglucose
-
18F Fluorodeoxyglucose
-
18-F Fluorodeoxyglucose
-
18F-Fluorodeoxyglucose
-
F-18 Fluorodeoxyglucose
-
F-18 Fludeoxyglucose
-
F18 Fludeoxyglucose
-
F18 Fluorodeoxyglucose
-
18FDG
-
18-FDG
-
18 FDG
-
18F FDG
-
18-F-FDG
-
18F-FDG
-
F18 FDG
-
F-18-FDG
-
F-18 FDG
-
F 18 FDG
-
FDG
-
FDG-PET
-
FDG-PET-CT
-
FDG-PET/CT
-
2-Fluoro-2-deoxy-D-glucose
-
2 Fluoro 2 deoxy D glucose
-
2-Fluoro-2-deoxyglucose
-
2 Fluoro 2 deoxyglucoses
Rights and permissions
About this article
Cite this article
Madsen, P.H., Holdgaard, P.C., Christensen, J.B. et al. Clinical utility of F-18 FDG PET-CT in the initial evaluation of lung cancer. Eur J Nucl Med Mol Imaging 43, 2084–2097 (2016). https://doi.org/10.1007/s00259-016-3407-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-016-3407-4