Abstract
Purpose
The role of the central serotonin (5-hydroxytryptamine, 5-HT) system in feeding has been extensively studied in animals with the 5-HT family of transporters (5-HTT) being identified as key molecules in the regulation of satiety and body weight. Aberrant 5-HT transmission has been implicated in the pathogenesis of human obesity by in vivo positron emission tomography (PET) and single-photon emission computed tomography (SPECT) imaging techniques. However, results obtained thus far from studies of central 5-HTT availability have been inconsistent, which is thought to be brought about mainly by the low number of individuals with a high body mass index (BMI) previously used. The aim of this study was therefore to assess 5-HTT availability in the brains of highly obese otherwise healthy individuals compared with non-obese healthy controls.
Methods
We performed PET using the 5-HTT selective radiotracer [11C] DASB on 30 highly obese (BMI range between 35 and 55 kg/m2) and 15 age- and sex-matched non-obese volunteers (BMI range between 19 and 27 kg/m2) in a cross-sectional study design. The 5-HTT binding potential (BPND) was used as the outcome parameter.
Results
On a group level, there was no significant difference in 5-HTT BPND in various cortical and subcortical regions in individuals with the highest BMI compared with non-obese controls, while statistical models showed minor effects of age, sex, and the degree of depression on 5-HTT BPND.
Conclusion
The overall finding of a lack of significantly altered 5-HTT availability together with its high variance in obese individuals justifies the investigation of individual behavioral responses to external and internal cues which may further define distinct phenotypes and subgroups in human obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity rates are currently at pandemic levels and if not curbed, the disease is on course to becoming the major preventable public health threat of the 21st century. A better understanding of the causative biological factors of obesity undoubtedly would aid both to prevent the development and the perpetuation of the disease and to identify potential treatment targets.
Studies in rodents have for decades implicated the central monoamine system in the regulation of energy homeostasis [1]. Only relatively recently this system has been suggested to play a role in the pathogenesis of human obesity. Focus has predominantly been placed so far on brain dopamine signaling and much less is known about the function of serotonin (5-HT) in the development of overweight and obese phenotypes. Central serotonergic mechanisms are prime candidates since there are numerous drugs that target 5-HT transmission, in particular 5-HT transporter (5-HTT) inhibitors such as sibutramine and fenfluramine, with proven clinical efficacy [2]. This includes the novel US Food and Drug Administration (FDA)-approved appetite-suppressing drug lorcaserin which is a 5-HT2c receptor agonist [3].
The use of mouse and rat strains that are resistant or prone to diet-induced obesity when placed on a high fat diet has provided insight into the role of central 5-HT transmission in body weight regulation. Diet-induced obese mice have higher levels of 5-HTTs in the nucleus accumbens, a brain region involved in the motivational aspects of feeding, compared to diet resistant mice [4]. Additionally, diet-induced obese rats have higher levels of 5-HT2A and 5-HT4 receptors [5], which is in general agreement with in vivo human PET studies [6–8].
To date, there have been several in vivo human PET studies using the highly selective 5-HT radioligand [11C] DASB examining the association between brain 5-HTT levels with obesity; however, findings so far have been inconsistent. Our preliminary data hinted at a positive correlation between BMI (range between 18 and 32 kg/m2) and 5-HTT availability in the insula, the ventral striatum, and the hypothalamus [9]. A subsequent PET study showed a negative correlation between subcortical (caudate-putamen-thalamus) [11C] DASB binding potential with BMI. These results were likely skewed by the low number of participants with higher BMI (>30 kg/m2) used. Thus, correlation curves may have been driven by outliers in the upper range. Recently it was shown that there is no difference in subcortical 5-HTT availability in obese patients before and after gastric bypass surgery or compared to lean controls, although no detailed correlation analysis was performed [10].
To more comprehensively assess central 5-HTT availability in human obesity, we aimed to investigate highly obese (BMI >35 kg/m2), otherwise healthy, non-depressed individuals compared with non-obese (BMI <30 kg/m2), healthy controls in various cortical, subcortical, and limbic regions using PET and [11C] DASB. Based on rodent andour own preliminary data, we hypothesized that higher BMI is associated with higher 5-HTT availability in brain areas involved in feeding.
Material and methods
Subjects
Thirty obese individuals with a BMI >35 kg/m2 and aged over 18 years were included. After obtaining informed consent, screening for inclusion/exclusion criteria, a general physical examination (including weight and height measures for BMI calculation) and magnetic resonance (MR) imaging, eligible study participants underwent PET with [11C] DASB as well as a comprehensive psychiatric and neuropsychological assessment. This included validated German language versions of the Beck depression inventory (BDI) [11]. Exclusion criteria were current or past neurological or psychiatric illness, i.e., depression (as assessed by a psychiatrist at the first visit), head trauma or vascular encephalopathy, resistant hypertension, insulin-dependent diabetes, or other medical conditions that may alter brain function, the use of anorectic medication or other interventions for weight loss, centrally acting medication, over-the-counter-medication or nutrition supplements over the last 8 weeks, past or present history of alcohol misuse and/or illicit drug abuse, pregnancy, and breast-feeding. Fifteen non-obese subjects, carefully matched for age and sex and free of any medication or illicit drugs, participated as controls. The study participants were Caucasians; none of the subjects fulfilled the criteria for binge-eating disorder nor were there participants with reported glucose intolerance. The amount of alcohol and/or nicotine consumption was recorded for both cohorts. One normal-weight control was excluded due to insufficient PET data statistics (less counts). Additionally, we investigated a length polymorphism of the 5-HTT coding gene (5-HTTLPR) as the potential influencing factor on in vivo 5-HTT PET signal [12].
Magnetic resonance (MR) imaging
Structural MR images were acquired using a 3T Siemens scanner and a T1-weighted 3D magnetization prepared rapid gradient echo (MP-RAGE) sequence (repetition time 2,300 ms, echo time 2.98 ms, 176 slices, field of view (FOV) 256 × 240 mm, voxel size 1 × 1 × 1 mm) for PET-MRI co-registration and (with other sequences based on the Alzheimer’s Disease Neuroimaging Initiative protocol) for exclusion of brain pathologies such as diffuse or confluent white matter hyperintensities in T2-weighted images, tumors, and stroke but not malformation without functional impairment.
Positron emission tomography (PET) imaging
[11C]DASB was synthesized according to a previous publication [13]. Dynamic PET was performed for 90 min after intravenous bolus injection (90 s) of (mean ± SD) 484 ± 10 MBq [11C]DASB using the ECAT EXACT HR+ scanner (Siemens, Erlangen, Germany; intrinsic resolution at the centre: 4.3 mm, axial resolution: 5–6 mm FOV 5.5 cm, 3–4 mm full width at half maximum) in three-dimensional (3D) acquisition mode. Emission scan acquired 23 frames (4 × 0.25, 4 × 1, 5 × 2, 5 × and 5, 5 × 10 min). We used a 10-min transmission scan (from 3 68Ge sources), which was performed prior to the emission scan, for attenuation correction and iterative reconstruction (ten iterations, 16 subsets) in transverse image series (63 slices, 128 × 128 matrix, voxel size 2.6 × 2.6 × 2.4 mm3) with a Hann filter (cutoff 4.9 mm) for image reconstruction. PET data were corrected for head motion artifacts using SPM2 (Statistical Parametric Mapping, Wellcome Department of Cognitive Neurology, London, UK) implemented in Matlab 7.3.0 (The MathWorks Inc., Natick, MA, USA). Then a summed image was built of the first 13 frames and co-registered with the individual 3D MRI data using PMOD software (Version 3.4) for re-alignment and stereo-tactical normalization (according to the anterior commissure-posterior commissure line). The same transformation was applied to the dynamic PET data. Parametric images of 5-HTT binding potential (BPND) were generated from the PET data by the multi-linear reference tissue model with two parameters (MRTM2) and the cerebellar cortex as the reference tissue [14, 15].
Imaging data analysis
Regional analyses of BPND values were consecutively performed atlas-based [16] by manual delineation of the volumes of interest (VOIs) for cortical, subcortical, and limbic areas including the amygdala, the hippocampus, the striatal subregions the head of the caudate and putamen, the nucleus accumbens (Acb), the thalamus, the hypothalamus, and the midbrain including the substantia nigra (SN) and ventral tegmental area (VTA) (Fig. 1). A voxelwise statistical analysis was performed using SPM8 (Statistical Parametric Mapping, Wellcome Department of Cognitive Neurology, London, UK) also implemented in Matlab 7.3.0 (MathWorks Inc., Natick, MA, USA). BPND maps were spatially normalized on the SPM8 integrated PET template and smoothed with 8 mm full-width-at-half-maximum (FWHM) on a Gaussian Filter. Group comparisons (two-sample t-test, obese vs. normal-weight controls) were considered significant for p < 0.005, unadjusted for multiple comparisons (T > 3.5) and a minimum of 30 voxels / cluster.
Parametric maps of binding potentials (BPND) and co-registered magnetic resonance images (MRIs) at two different levels, the striatum/thalamus (upper row) and the brainstem (bottom row). Arrows indicate (A) anterior cingulate cortex, (B) head of the caudate, (C) amygdala, (D) substantia nigra, and (E) periaqueductal grey
Statistical analysis
The data were tested for normal distribution using the Shapiro-Wilks test and the Levene test for homogeneity of variance. After thorough review and tests excluding asymmetries between corresponding left and right brain regions, VOIs were averaged side-by-side to reduce the number of dependent variables within the models. To estimate the difference in variance between and within the groups, an analysis of variance (ANOVA) was performed. For correlative analysis the Pearson product–moment correlation was applied (two-sided) and partial analysis if univariate analysis of covariance (ANCOVA) indicated a significant covariate effect by comparing the groups of obese and non-obese subjects regarding differences between the measured BPND within all brain VOIs and epidemiological factors (age, sex, and smoking habits), seasonal data (day length and sunshine duration), BDI, and 5-HTTLPR genotypes as covariates (complete data set for n = 44). Additionally, a mixed linear modeling analysis was performed including the regions with high BPND (e.g., grouping the subcortical and the limbic regions in two separate analyses) to test whether there is a significant difference in subcortical or limbic regions between obese and non-obese subjects. If many relationships were tested, correction for multiple comparisons using a false discovery rate was applied to adjust the significance level.
Results
Subject characteristics and epidemiological data are summarized in Table 1. Obese and non-obese study participants not only differed in BMI but also in BDI and the length of the scanning day. All other parameters (sex, smoking habits, and 5-HTTLPR) were well matched.
Serotonin transporter (5-HTT) binding potential (BPND) in obese versus non-obese individuals
The BPND values in selected regions relevant for appetite control are shown in Fig. 2. Overall, no significant group differences in mean BPND were found (ANOVA); the entire BPND data are summarized in Table 2. Mean between-subject variability was 12.1 % in obese and 9.5 % in non-obese individuals, respectively, but this was not significantly different (for region-specific variability see Table 3). Results also indicate no significant differences in the test for homogeneity of variances between the groups. In the analyses of each sub-cohort, BMI and BPND did not correlate (voxel-wise and VOI-based analyses), ranging from r = 0.27 (p = 0.14) for the thalamus to r = 0.03 (p = 0.89) for the hippocampus in the obese study group, and from r = 0.28 (p = 0.33) for the head of the caudate to r = −0.33 (p = 0.24) for the insula in the non-obese study group (Table 3). Neither did we find a significant difference between obese and non-obese subjects by grouping either the subcortical or the limbic regions in a mixed linear model analysis (p = 0.53, and p = 0.51, vs. BMI p = 0.51, and p = 0.25, respectively). Inter-regional correlation analyses of BPND revealed more robust associations in obese compared with non-obese controls as this mainly included the insula and the ACC (Fig. 3).
Spearman rank correlation coefficients matrix of serotonin transporter (5-HTT) binding potentials between every volume of interest for the obese subjects (lower left triangle) and non-obese controls (upper right triangle). Regions are sorted based on the mean correlation coefficient per volume of interest. Ins insula, ACC anterior cingulate cortex, Amg Amygdala, Cd head of the caudate, Hypothal hypothalamus, Pu putamen, DLPFC dorsolateral prefrontal cortex, Acb nucleus accumbens, SN_/_VTA substantia nigra/ventral tegmental area, Th thalamus, OFC orbito-frontal cortex, Hi hippocampus, FC medial prefrontal cortex, Raphe raphe nuclei)
Corrected model of body mass index (BMI)-associated 5-HTT binding potential (BPND)
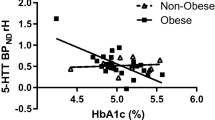
Bivariate correlative analyses indicated an effect of age (in the thalamus r = −0.35; p = 0.02) and of BDI (in the OFC r = 0.30; p = 0.05) on BPND. Considering all covariates in an analysis of covariance, no overall significant effect on obese versus non-obese subjects were detected (Table 4). For distinct VOIs, however, covariates showed significant or borderline-significant effects, e.g., age in the dorsolateral PFC, the ACC, the thalamus, and 5-HTTLPR in the hippocampus, respectively (Table 4). By using these variables as covariates in SPM analyses, however, we found either no additional effect on the relationship between BMI and BPND or small clusters of BPNDversus BMI correlation when considering BDI as covariate (Fig. 4).
Statistical parametric mapping (SPM8) projections superimposed on representative magnetic resonance imaging slices, small clusters with significant decreased values (blue/top; putamen) and increased values (green/bottom; pons) in obese subjects (n = 30) compared with normal-weight (n = 14) controls (using Beck depression inventory as a covariate) (p < 0.005, uncorrected, 30 voxel/cluster minimum)
Discussion
Among the various drugs available that target central biogenic amine pathways, the combined 5-HTT and norepinephrine transporter (NET) inhibitor sibutramine has been demonstrated to be the most effective for both the long-term treatment of obesity and amelioration of obesity-related health risks [2, 17]. Hence, brain 5-HTTs have been implicated in the etiology of obesity; the evidence obtained from in vivo human imaging data thus far, however, are sparse and contradictory [8–10]. This is the first study to comprehensively compare highly obese yet metabolically healthy and non-depressed individuals with non-obese healthy controls using in vivo 5-HTT brain PET. The findings obtained here indicate that there is no significant effect of BMI on regional 5-HTT availability on a group level, in line with a recent PET analysis on patients undergoing bariatric surgery [10]. In particular, there was no indication that in cortical, subcortical, or limbic regions 5-HTT availability is higher in obese subjects. Notably, the group difference was comparatively large and approaching statistical significance in the OFC, a brain region strongly activated by the appetite suppressant and 5-HT1B/2C receptor agonist mCPP [18].
In terms of pathophysiology, a change in serotonergic tone or compensatory up-regulation of 5-HTT may determine the individual variance in response to favorite-food or stress cues, and in appetitive or defensive motivated behavior. In our previous study, the high 5-HTT availability associated with high BMI was hypothesized to lead to or result from low synaptic 5-HT levels underlying hyperphagia and weight gain [9, 19]. The higher 5-HTT availability in the OFC of obese subjects in the present study is in keeping with this theory. In contrast, a SPECT study exclusively focusing on the hypothalamus in human subjects revealed reduced 5-HTT availability that occurred within 6 weeks of consuming a high calorie diet associated with modest weight gain [20]. It is possible that these inconsistencies can be explained by the quadratic relationship between 5-HTT and 5-HT implied by the study of Haahr and colleagues [10]. Thus, expected group differences will be harder to prove and are meaningful only in relation to other parameters such as stress or behavioral responses, similar to that that has been discussed for NET [21]. We surmise that since the 5-HT system is a tonic, modulatory network with widespread serotonergic innervation from the raphe nuclei, 5-HTT availability does not necessarily simply reflect either decreases or increases in synaptic 5-HT concentrations. One can assume rather that input from internal and external sources differentially activate serotonergic tone in obese versus non-obese controls which can be addressed by dedicated challenge studies when probes sensitive for endogenous 5-HT fluctuations become available.
Studies on high fat diet-resistant mice have previously shown increased 5-HTTs in the nucleus accumbens compared to diet-induced obese mice [4]. This finding was not reproduced when comparing high fat diet-resistant with diet-induced obese rats or in other brain regions including the hypothalamus [5]. Long-term manipulation of 5-HTT function in knockout (KO) animals has also yielded conflicting findings. Such animals develop paradoxical sex-specific forms of obesity not attributable to changes in feeding and which may be due to changed 5-HT signaling in the periphery [22, 23]. These findings nevertheless suggest that 5-HTTs play redundant roles in the control of feeding behavior. It seems instead that 5-HT receptors are indispensable for normal appetite regulation. For instance, 5-HT2C receptor KO mice are hyperphagic and obese and when 5-HT2C receptors are restored in a subpopulation of hypothalamic neurons, this leads to reversal of obesity and in re-sensitization to the anorectic effect of 5-HTT inhibitors [24]. The importance of 5-HT receptors in body-weight regulation is also supported by the consistent observations of changes in levels of 5-HT2A and 5-HT4 receptors in human obesity [6, 7].
We did not find major effects of potential covariates (sex, age, 5-HTTLPR, or seasonal data) on 5-HTT binding potential within the age range and sample size of our cohort; mainly age interferes with BP in parts of the forebrain. On a voxel-level, depression was demarked by smaller clusters in the brainstem and the striatum (but not amygdala) which requires further validation with clinically depressed participants [24]. Given that the current BDI version includes items for weight loss, body shape, or libido, the validity and performance of the questionnaire for mood disorders (i.e., subsyndromal depression) in obese patients is likely to be modest [25]. Regression analysis was hampered by the fact that weight/BMI is a continuous variable but we did not include here subjects between 30 and 35 kg/m2 due to the intended extreme cohort design of the study; thus BMI appears rather to be dichotomous and correlative analysis needs further prospective validation by including subjects with a BMI range of between 30 and 35 kg/m2.
In order to obtain first insights on connectivity between the regions as an index of obesity beyond regional 5-HTT availability, we further inter-correlated regional BPND. This analysis revealed that there is a higher degree of correlation in the obese cohorts with a larger number of significant associations between regions as compared with non-obese controls (and possibly indicating an altered tone as well). Connectivity within this 5-HTT network seems to be significantly stronger in areas of saliency attribution and interoception with the insula and the ACC demonstrated to be robustly connected in the obese but not in the non-obese. However, we cannot rule out a specific network pattern in either obese individuals or non-obese controls as the correlation matrix was obtained solely from BPND and not from dynamic data. Future studies on network correlates may include covariant information using sparse inverse covariance estimation [26]. It is hence of further interest how the resting-state data of the study participants are modulated by individual 5-HTT availability, both at baseline and with interventions such as testing for food-cue reactivity. From functional MRI (fMRI) data an enhanced reactivity and a more effortful strategy for appetite control in obese individuals [27] corroborates the idea of higher 5-HT-mediated arousal, in particular in areas of affective-cognitive processing, in such persons. It is of further interest that the BPND of the obese group is highly correlated but still exhibits a high degree of variation (although the difference in variance is not significant). Future studies therefore will focus on this variability by entering additional parameters such as obesity-related leptin, ghrelin, and stress-related indicators.
The present findings may have implications in designing optimal treatment strategies for obesity. For instance targeting 5-HTTs may not prevent obesity development per se in susceptible individuals. However, inhibiting 5-HTTs in established obesity still remains an attractive therapeutic option. This is further supported by the recent finding that changes in subcortical 5-HTTs inversely correlate with extent of body weight loss in obese individuals after gastric bypass surgery [10]. The role of the other biogenic amines in this context are also of interest and dedicated studies (e.g., by dual-tracer approaches) warrant consideration. Additionally, serotonergic mechanisms have been implicated in obesity-related medical conditions like depression where resting-state hyperactivity in subcortical core–paracore regions was found to be related to abnormal function of the neuromodulatory systems located in the raphe nucleus and the locus coeruleus with 5-HT and NE (and other transmitters like dopamine and acetylcholine) [28, 29]. In keeping with this, preclinical findings in 5-HTT knock-out mice point to modulation of the limbic cortical-ventral striatopallidal pathway as a consequence of perturbed 5-HTT function. Thus, molecular disruption of 5-HTT that produce behavioral changes alter the functional anatomy of the reward circuitry in which all the monoamine systems are involved [30].
One further limitation in the interpretation of our study results is the fact that we did not implement a 1:1 case-cohort design, although we carefully matched obese and non-obese samples on an individual basis. Although large for a PET study, the sample size was relatively small, which may have obscured individual differences (e.g., sex, age, and 5-HTTLPR) that have been linked to important aspects of eating behaviors such as impulse control and obesity.
In conclusion, we showed no significant alterations of 5-HTT availability in obese compared with non-obese individuals but, seemingly, there is high variance of 5-HTT availability. These results may provide a useful platform upon which to further investigate 5-HT functions in human obesity.
References
Leibowitz SF. Hypothalamic neurotransmitters in relation to normal and disturbed eating patterns. Ann N Y Acad Sci. 1987;499:137–43.
Garfield AS, Heisler LK. Pharmacological targeting of the serotonergic system for the treatment of obesity. J Physiol. 2009;587:49–60.
Smith SR, Weissman NJ, Anderson CM, Sanchez M, Chuang E, Stubbe S, et al. Behavioral Modification and Lorcaserin for Overweight and Obesity Management (BLOOM) Study Group. Multicenter, placebo-controlled trial of lorcaserin for weight management. N Engl J Med. 2010;363:245–56.
Huang XF, Huang X, Han M, Chen F, Storlien L, Lawrence AJ. 5-HT2A/2C receptor and 5-HT transporter densities in mice prone or resistant to chronic high-fat diet-induced obesity: a quantitative autoradiography study. Brain Res. 2004;1018:227–35.
Ratner C, Ettrup A, Bueter M, Haahr ME, Compan V, le Roux CW, et al. Cerebral markers of the serotonergic system in rat models of obesity and after Roux-en-Y gastric bypass. Obesity (Silver Spring). 2012;20:2133–41.
Haahr ME, Rasmussen PM, Madsen K, Marner L, Ratner C, Gillings N, et al. Obesity is associated with high serotonin 4 receptor availability in the brain reward circuitry. Neuroimage. 2012;61:884–8.
Erritzoe D, Frokjaer VG, Haugbol S, Marner L, Svarer C, Holst K, et al. Brain serotonin 2A receptor binding: relations to body mass index, tobacco and alcohol use. Neuroimage. 2009;46:23–30.
Erritzoe D, Frokjaer VG, Haahr MT, Kalbitzer J, Svarer C, Holst KK, et al. Cerebral serotonin transporter binding is inversely related to body mass index. Neuroimage. 2010;52:284–9.
Hesse S, Villringer A, Schönknecht P, Becker GA, Patt M, Bresch A, et al. Serotonin transporter (SERT) availability, body mass index (BMI) and depression. J Nucl Med. 2009;50 Suppl 2:1294.
Haahr ME, Hansen DL, Fisher PM, Svarer C, Stenbæk DS, Madsen K, et al. Central 5-HT Neurotransmission modulates weight loss following gastric bypass surgery in obese individuals. J Neurosci. 2015;35:5884–9.
Hautzinger M. Das Beck Depressions-Inventar (BDI) in der Klinik. Nervenarzt. 1991;62:689–6.
Hesse S, Stengler K, Regenthal R, Patt M, Becker GA, Franke A, et al. The serotonin transporter availability in untreated early-onset and late-onset patients with obsessive-compulsive disorder. Int J Neuropsychopharmacol. 2011;14:606–17.
Wilson AA, Ginovart N, Schmidt M, Meyer JH, Threlkeld PG, Houle S. Novel radiotracers for imaging the serotonin transporter by positron emission tomography: synthesis, radiosynthesis, and in vitro and ex vivo evaluation of 11C-labeled 2-(phenylthio)araalkylamines. J Med Chem. 2000;43:3103–10.
Ichise M, Liow JS, Lu JQ, Takano A, Model K, Toyama H, et al. Linearized reference tissue parametric imaging methods: application to [11C]DASB positron emission tomography studies of the serotonin transporter in human brain. J Cereb Blood Flow Metab. 2003;23:1096–112.
Innis RB, Cunningham VJ, Delforge J, Fujita M, Gjedde A, Gunn RN, et al. Consensus nomenclature for in vivo imaging of reversibly binding radioligands. J Cereb Blood Flow Metab. 2007;27:1533–9.
Mai JK, Assheuer J, Paxinos G. Atlas of the human brain. 2nd ed. San Diego: Elsevier Academic; 2004.
Hainer V, Kabrnova K, Aldhoon B, Kunesova M, Wagenknecht M. Serotonin and norepinephrine reuptake inhibition and eating behavior. Ann N Y Acad Sci. 2006;1083:252–69.
Stark JA, Davies KE, Williams SR, Luckman SM. Functional magnetic resonance imaging and c-Fos mapping in rats following an anorectic dose of m-chlorophenylpiperazine. Neuroimage. 2006;31:1228–37.
Hesse S, van de Giessen E, Zientek F, Petroff D, Winter K, Dickson JC, et al. Association of central serotonin transporter availability and body mass index in healthy Europeans. Eur Neuropsychopharmacol. 2014;24(8):1240–7.
Koopman KE, Booij J, Fliers E, Serlie MJ, la Fleur SE. Diet-induced changes in the Lean Brain: Hypercaloric high-fat-high-sugar snacking decreases serotonin transporters in the human hypothalamic region. Mol Metab. 2013;2:417–22.
Li CS, Potenza MN, Lee DE, Planeta B, Gallezot JD, Labaree D, et al. Decreased norepinephrine transporter availability in obesity: positron emission tomography imaging with (S, S)-[11C]O-methylreboxetine. Neuroimage. 2014;86:306–10.
Uçeyler N, Schütt M, Palm F, Vogel C, Meier M, Schmitt A, et al. Lack of the serotonin transporter in mice reduces locomotor activity and leads to gender-dependent late onset obesity. Int J Obes (Lond). 2010;34:701–11.
Homberg JR, la Fleur SE, Cuppen E. Serotonin transporter deficiency increases abdominal fat in female, but not male rats. Obesity (Silver Spring). 2010;18:137–45.
Gryglewski G, Lanzenberger R, Kranz GS, Cumming P. Meta-analysis of molecular imaging of serotonin transporters in major depression. J Cereb Blood Flow Metab. 2014;34:1096–103.
Udo T, McKee SA, Grilo CM. Factor structure and clinical utility of the Beck depression inventory in patients with binge eating disorder and obesity. Gen Hosp Psychiatry. 2015;37:120–25.
Zou N, Chetelat G, Baydogan MG, Li J, Fischer FU, Titov D, et al. Metabolic connectivity as index of verbal working memory. J Cereb Blood Flow Metab. 2015;35:1122–6.
Scharmüller W, Übel S, Ebner F, Schienle A. Appetite regulation during food cue exposure: a comparison of normal-weight and obese women. Neurosci Lett. 2012;518:106–10.
Drevets WC, Price JL, Furey ML. Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Struct Funct. 2008;213:93–118.
Northoff G, Wiebking C, Feinberg T, Panksepp J. The ‘resting-state hypothesis’ of major depressive disorder-a translational subcortical-cortical framework for a system disorder. Neurosci Biobehav Rev. 2011;35:1929–45.
Bearer EL, Zhang X, Janvelyan D, Boulat B, Jacobs RE. Reward circuitry is perturbed in the absence of the serotonin transporter. Neuroimage. 2009;46:1091–104.
Acknowledgments
We are very grateful to Damian McLeod, School of Biomedical Sciences and Pharmacy, University of Newcastle, Australia, for careful line editing and English proofreading of the first draft of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the German Federal Ministry of Education and Research (FKZ: 01EO1001).
Conflict of interest
The authors report no conflicts of interest relating to the content of this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ICH Guideline for Good Clinical Practice (GCP) and with the 1964 Helsinki declaration and its later amendments. The study was approved by the ethics committee of the Medical Faculty of the University of Leipzig (registered under the number 206-10-08032010) and the German Bundesamt für Strahlenschutz/Federal Office for Radiation Protection (number Z5-22461-2-2011-002), and registered at the European clinical trial database EudraCT 2012-000568-32) and the German Clinical Trials Register (DRKS).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Hesse, S., Rullmann, M., Luthardt, J. et al. Central serotonin transporter availability in highly obese individuals compared with non-obese controls: A [11C] DASB positron emission tomography study. Eur J Nucl Med Mol Imaging 43, 1096–1104 (2016). https://doi.org/10.1007/s00259-015-3243-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-015-3243-y