Abstract
Objectives
To correlate the cross-sectional area (CSA) and elasticity of the median nerve (MN) measured at carpal tunnel inlet between healthy controls and various degrees of carpal tunnel syndrome (CTS) graded as per nerve conduction studies (NCS).
Materials and methods
A total of 53 patients (with 81 wrists) presenting with clinical symptoms characteristic of CTS, having their diagnosis confirmed and severity graded by NCS, and 48 healthy controls (with 96 wrists) were included in the study. All the study participants underwent wrist ultrasound which included initial Grey-scale USG followed by strain and shear wave elastography. The CSA and elasticity (in terms of strain ratio and shear modulus) of MN were measured at the carpal tunnel inlet. Statistical analysis was performed using the Mann–Whitney U test to compare between the two groups and for subgroup analysis of cases. The diagnostic performance of each variable was evaluated using the receiver operating characteristic curves.
Results
The mean CSA was 9.20 ± 1.64, 11.48 ± 1.05, 14.83 ± 1.19 and 19.87 ± 2.68 mm2, the mean shear modulus was 17.93 ± 2.81, 23.59 ± 2.63, 32.99 ± 4.14 and 54.26 ± 9.24 kPa and the mean strain ratio was 5.26 ± 0.68, 5.56 ± 0.70, 7.03 ± 0.47 and 8.81 ± 0.94 in control, mild, moderate and severe grades of CTS, respectively (p < 0.001).
Conclusion
The combined utility of Grey-scale USG and Elastography may serve as a painless and cost-effective alternative to NCS in grading the severity of CTS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Carpal tunnel syndrome (CTS) is a common prevalent entrapment neuropathy caused by median nerve compression at the wrist. Symptoms include pain and paresthesia worsening at night, affecting the distribution of the median nerve distal to the carpal tunnel. CTS is bilateral in up to 50% of cases, predominantly affecting women between the third and sixth decades, with an estimated prevalence of 0.6 to 5.8% in the general population. However, most affected cases usually go undiagnosed [1, 2].
Currently, the diagnosis of CTS involves clinical evaluation of history and physical examination followed by NCS to confirm the diagnosis and grade the severity.
Grading the severity of carpal tunnel syndrome (CTS) is clinically relevant as it aids clinicians in determining the most appropriate treatment for each patient. Conservative measures such as wrist splinting, activity modification, and corticosteroid injections often effectively manage mild cases. However, severe cases may necessitate surgical intervention, thus facilitating prognostication and optimizing patient outcomes.
NCS is currently considered the gold standard for grading CTS severity. However, it is time-consuming, relatively expensive, uncomfortable, and has a false-negative rate of 16 to 34% [3].
In the past two decades, numerous studies have been conducted evaluating the efficacy of various ultrasound imaging parameters [4,5,6,7,8,9,10,11,12,13,14] in diagnosing CTS accurately, among which measurement of CSA of MN at carpal tunnel inlet has proven to be the most reliable parameter [15].
Sono-elastography was initially reported as an imaging technique to assess tissue stiffness in the 1990s [16]. Since then, its role in the evaluation of breast, liver, thyroid, and prostate has been extensively studied and used in clinical practice. However, there is limited available literature regarding its role in the evaluation of peripheral nerves.
The current study aimed to independently evaluate the efficacy of Grey-scale USG, Strain Elastography (SE), and Shear Wave Elastography (SWE) in classifying the severity of CTS and to determine their reliability as crucial diagnostic tools, with the potential to replace NCS.
Materials and methods
Patient selection
Following approval and clearance from the Institutional Ethics Review Committee, we conducted a hospital-based prospective case–control study from March 2021 to February 2023 at a tertiary care center in South India. A total of 107 participants were enrolled in the study and were divided into two groups — Group A consisted of 57 patients with 91 wrists clinically diagnosed with CTS and underwent NCS. Group B consisted of 50 controls with 100 wrists who did not have any clinical symptoms or signs of CTS. Controls were recruited from either the patient’s accompanying healthy relatives or individuals referred to the Department of Radiodiagnosis for Ultrasound imaging of unrelated indications, such as abdomen and pelvis scans. These control participants were clinically assessed and those who exhibited no clinical symptoms suggestive of CTS and had no comorbidities or systemic illnesses that might affect peripheral nerves were recruited into the study. The study excluded patients with a history of trauma or surgical interventions involving the symptomatic wrist, and those with rheumatoid arthritis, diabetes mellitus, acromegaly, neurological, thyroid, and other endocrine disorders. Additionally, patients showing anatomical variations of the MN, such as bifid nerve or persistent median artery, were excluded as well.
Fourteen wrists from both groups were excluded from the study. Among them, nine wrists had bifid median nerve, one had a history of surgery, and four wrists of two patients with a history of hypothyroidism were excluded.
All participants enrolled in the study were explained about the procedure in detail in a language understandable to them, and written and informed consent was taken from both groups. Structured, pre-prepared templates were employed to systematically document participant details, including name, age, gender, clinical history, results of physical examination, and findings from investigations such as ultrasound (including Color Doppler), elastography, and nerve conduction studies.
USG technique
Grey-scale USG, Color Doppler, and elastography examination were performed on both groups using a SAMSUNG RS80 EVO Ultrasound machine with a 2–9 Mega Hertz linear transducer. All ultrasound examinations were performed by two radiologists with an experience of 4 years and 11 years in musculoskeletal radiology. Both radiologists were blinded to the severity of symptoms and NCS results of the Carpal Tunnel Syndrome group. They independently conducted ultrasound and elastography within an interval of less than 24 h. However, they were aware of the participant’s demographic data, including name, age, sex, and whether the participant belonged to the CTS group or the control group.
The study participants were comfortably seated on the USG couch facing the examiner with the arm adducted, elbow flexed at 90°, forearm supinated, wrist resting on the participant’s lap, and fingers held in a relaxed semi-flexed position (Fig. 1). The median nerve was assessed along its entire course in the wrist to look for any anatomical variations or other anomalies. However, the measurements were specifically obtained only at the carpal tunnel inlet. After application of adequate amount of acoustic coupler (AC), the transducer was gently placed on the volar aspect at the distal palmar crease. A transverse grey scale image of the MN was recorded. The CSA of MN was obtained by tracing a continuous line at the hyperechoic boundary of the MN, including its epineurium. Each measurement was taken five times. The highest and lowest values were discarded, and the remaining three values were averaged to obtain representative values, in an attempt to remove intra-observer variations.
Color Doppler ultrasound was performed with adequate PRF and color gain settings suitable for detecting low flow within the vessels. If color uptake was not visualized with these settings, images were assessed in Power Doppler mode to look for intra/perineural hypervascularity.
Sono-elastography technique
The transducer was again placed on the volar aspect of the wrist after applying an ample amount of AC to avoid the compression effect of the transducer. MN was identified at the carpal tunnel inlet in the transverse imaging plane. After obtaining adequate compression for SE as suggested by the strain indicator (on the upper right corner of the ultrasound monitor screen), the paired Grey-scale and color-coded strain elastogram images were used to calculate the strain ratio (SR). The target Region of Interest (ROI) was placed within the MN to cover as much CSA as possible. A similar-sized reference ROI was placed at the overlying AC, and the SR of reference ROI to the target ROI (AC/MN) was obtained. With the same settings, SWE was performed to obtain shear modulus (SM) with the help of pre-installed software in the USG machine, which automatically displayed the stiffness of MN in terms of Kilo Pascals (kPa) on the ultrasound monitor. The procedure was repeated to obtain the SR and SM five times. The highest and lowest values were discarded, and the remaining three values were averaged to obtain representative values, in an attempt to remove intra-observer variations.
Technique and interpretation of NCS
All patients with clinically suspected CTS underwent NCS. The examination was performed according to the protocol recommended by the American Association of Electrodiagnostic Medicine [17] by a single neurophysiologist with 8 years of experience using an EBN Galileo machine with two channels. Patients were made to lie supine with both upper limbs positioned at rest alongside the body.
The CTS protocol included — median nerve motor study recording the abductor pollicis brevis, stimulating at wrist and antecubital fossa; ulnar nerve motor study recording the abductor digiti minimi, stimulating at wrist, below and above the ulnar groove; median and ulnar F responses; median sensory response obtained from recording digit 3, stimulating at wrist; ulnar sensory response obtained from recording digit 5, stimulating at wrist and radial sensory response, recording anatomical snuffbox, stimulating over the lateral radius.
The diagnosis of isolated CTS was made if the median studies were abnormal, showing marked prolongation of distal motor (> 4.4 ms) and sensory latencies (> 3.5 ms), and prolonged minimum F wave latencies (> 31 ms). Diminished median CMAP (< 4 mV) and SNAP (< 20 µV) amplitudes indicating secondary axonal loss or demyelination leading to conduction block at the wrist along with normal ulnar motor, sensory, and F wave studies and normal radial sensory response.
If the median nerve studies were completely normal or showed equivocal results, the median-versus-ulnar comparison tests were done which included:
Comparison of the median and ulnar mixed palm-to-wrist peak latencies, stimulating the median and ulnar palm one at a time 8 cm from the recording electrodes placed over the median and ulnar wrist, respectively (abnormal if the difference is > 0.4 ms); comparison of the median lumbrical and ulnar interossei distal motor latencies, stimulating the median and ulnar nerve at wrist one at a time at identical distance of ~ 8–10 cm, recording with the same electrode over the second lumbrical/interossei (abnormal if the difference is > 0.5 ms); and comparison of the median and ulnar digit 4 sensory latencies, stimulating the median and ulnar nerve at wrist one at a time at identical distances of ~ 11–13 cm and recording digit 4 (abnormal if the difference is > 0.5 ms).
Based on the NCS results, CTS severity was graded into mild, moderate, and severe as per the classification suggested by Stevens et al. [18].
-
Mild CTS — prolonged (relative or absolute) sensory or mixed nerve actional potential (NAP) distal latency ± sensory nerve action potential (SNAP) amplitude below the lower limit of normal.
-
Moderate CTS — abnormal median nerve sensory latencies as described above, and (absolute or relative) prolongation of median motor distal latency.
-
Severe CTS — prolonged median motor and sensory distal latencies, with either an absent SNAP or mixed NAP or low amplitude or absent thenar compound muscle action potential (CMAP).
Statistical analysis
The data collected was stored in the form of Microsoft Excel spreadsheets for analysis. Mann–Whitney U test was used for comparison between Group A and B and subgroup analysis of Group A, Spearman’s correlation coefficient was used to determine the relationship between variables of interest, Intra Class correlation coefficient to assess the extent of agreement between observers, receiver operating characteristic curve (ROC) to assess cut-off values for each parameter in question and Youden’s index to assess the sensitivity and specificity. All the above analysis was done using STATA 18 MP software.
Results
The final study group consisted of Group A with 53 patients (34 female, 19 male with mean age of 43.9 years) and 81 wrists (13 right, 12 left, and bilateral wrists in 28 cases), and Group B with 48 controls (29 female, 19 male with mean age of 45.1 years) and 96 wrists (bilateral wrists of 48 controls). The 81 wrists in Group A were classified according to NCS as Mild (n = 36), moderate (n = 33) and severe (n = 12) grades. All three ultrasound parameters, including CSA, SR, and shear modulus, exhibited statistically significant differences (p < 0.001) between Group A and Group B, as well as among subgroups within Group A (viz, mild vs. moderate; moderate vs. severe; mild vs. severe). The mean CSA, SR, and shear modulus of Group B and all three subgroups of Group A are summarized in Table 1 and the comparison of measurement parameters between subgroups of Group A is presented in Table 2.
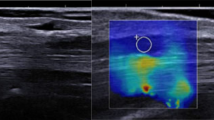
Figures 2, 3, 4 and 5 show representative Grey-scale, Color/Power Doppler, SE, and SWE images of control and CTS subgroups (mild, moderate, and severe). Among 81 symptomatic wrists, Color/Power Doppler revealed intra/perineural hyperemia in approximately 18.5% (15 wrists) of cases. None of the controls showed median nerve hyperemia on Color Doppler. Of the symptomatic wrists showing hyperemia, 2.8% belonged to mild, 24.2% to moderate, and 50.0% to severe category of carpal tunnel syndrome grading. Figure 6 shows representative images of intraneuronal hyperemia demonstrated on Color Doppler with low flow settings. The AUC for each parameter with the best cut-offs for diagnosing CTS is shown in Table 3 and Fig. 7. The AUC of shear modulus showed the maximum value (AUC of 0.974; 95% CI 0.938 to 0.992) followed by CSA (AUC of 0.954; 95% CI 0.912 to 0.980) and SR (AUC of 0.834; 95% CI 0.771 to 0.885). Furthermore, all three parameters demonstrated a positive correlation with NCS grading, with CSA (ρ = 0.903) and shear modulus (ρ = 0.906) exhibiting a stronger positive correlation compared to SR (ρ = 0.885). A cut-off of > 11 mm2 for CSA had the highest validity in differentiating cases and controls with a sensitivity of 80.25%, specificity of 93.75%, PPV of 91.5%, and NPV of 84.9%. A cut-off of > 22.3 kPa for shear modulus had the highest validity in differentiating cases and controls with a sensitivity of 86.42%, specificity of 96.87%, PPV of 95.9% and NPV of 89.4%. A cut-off of > 6.15 for SR had the highest validity in differentiating cases and controls with a sensitivity of 66.67%, specificity of 98.96%, PPV of 98.2%, and NPV of 77.9%. All parameters in both the cases and control groups demonstrated good inter-observer agreement, with ICC values of 0.95, 0.97, and 0.98 for cross-sectional area, strain ratio, and shear modulus, respectively.
Ultrasound images of right wrist in a healthy 42-year-old female with no clinical signs and symptoms of CTS; (a) transverse Grey scale USG image at the level of carpal tunnel inlet shows MN with CSA of 10 mm2; (b) on Color Doppler examination, no intraneural hyperemia seen; (c) on SWE, shear modulus of MN was 14.3 kPa; (d) on SE, AC/MN SR was 4.07
Ultrasound images of left wrist in a 44-year-old male with clinical symptoms of CTS and severity grading of mild on NCS; (a) transverse Grey scale USG image at the level of carpal tunnel inlet showed MN with CSA of 13 mm2; (b) on Color Doppler examination, no intraneural hyperemia was seen; (c) on SWE, shear modulus of MN was 23.7 kPa; (d) on SE, AC/MN SR was 4.84
Ultrasound images of right wrist in a 45-year-old female with clinical symptoms of CTS and severity grading of moderate on NCS; (a) transverse Grey-scale USG image at the level of carpal tunnel inlet showed MN with CSA of 16 mm2; (b) on Color Doppler examination, no intraneural hyperemia was seen; (c) SWE showed shear modulus of MN as 35.2 kPa; (d) on SE, AC/MN SR was 7.66
Ultrasound images of right wrist in a 52-year-old female with clinical symptoms of CTS and severity grading of severe on NCS; (a) transverse Grey scale USG image at the level of carpal tunnel inlet showed MN with CSA of 21 mm2; (b) on Color Doppler examination, intraneural hyperemia was seen; (c) on SWE, shear modulus of MN was 54.2 kPa; (d) on SE, AC/MN SR was 10.96
Discussion
Increased pressure within the carpal tunnel induces venous congestion, leading to nerve edema and swelling, observable as an increase in CSA on Grey scale USG. Chronic ischemia ensues due to vasa nervorum obstruction, resulting in demyelination, axonal degeneration, and fibroblastic proliferation causing nerve stiffening, reflected as increased stiffness on elastography, characterized by elevated strain ratio in strain elastography (SE) and increased shear modulus in SWE. In our study evaluating the median nerve in CTS patients, we incorporated the simplest and most common grey scale parameter: the CSA of the median nerve at the carpal tunnel inlet. Our findings aligned with those of other similar studies, demonstrating the effectiveness of this parameter in assessing CTS. All three parameters assessed—MN-CSA, shear modulus, and SR showed statistically significant differences between CTS cases and controls (p < 0.001). Additionally, their values consistently increased with disease severity among subgroups of cases (p < 0.001). The accuracy of these parameters in distinguishing between cases and controls ranked in descending order as follows: shear modulus > CSA > SR, as deduced from the AUC.
Studies evaluating the median nerve in carpal tunnel syndrome (CTS), such as those by Wong et al. [4], Mallouhi et al. [5] and Moran et al. [8], have shown significant differences in Median Nerve Cross-Sectional Area between cases and controls, particularly when measured at or just proximal to the carpal tunnel inlet. These studies recommend cut-off values ranging from 9 to 13 mm2, similar to our study where the cut-off was determined to be 11 mm2. This cut-off demonstrated the highest validity in differentiating cases and controls, with a sensitivity of 80.25% and specificity of 93.75%.
Limited literature exists regarding the role of elastography, an emerging modality in ultrasound imaging, in diagnosing and grading CTS, either independently or in conjunction with Grey scale USG. Numerous studies have investigated the role of CSA of the median nerve in CTS, but there is a paucity of research on elastography’s role. Various parameters, including color diagram, strain, strain ratio (SR), shear wave velocity, and shear modulus, have been utilized to assess elasticity changes in the median nerve.
SE, as an operator-dependent technique, measures tissue deformation/strain in response to mechanical compression by an ultrasound transducer. Our study, akin to research by Miyamoto H et al., Yoshii Y et al., and Asadov R et al. [19,20,21], incorporated semi-quantitative measurement of MN stiffness using SE. The stiffness of the MN was expressed as the AC/MN strain ratio, revealing a statistically significant difference in strain ratio between CTS cases and controls. However, SE exhibited poor performance in identifying the various subgroups of CTS. Interestingly, our study found substantial variations in SR between CTS subgroups, contrary to the earlier findings.
In Miyamoto et al.’s study, which included 31 patients with CTS, both the CSA and SR of the MN were assessed. They found that both parameters exhibited significantly higher values in CTS cases compared to controls. The authors suggested diagnostic cut-off values of 11 mm2 for MN-CSA and 4.3 for SR to aid in the diagnosis of CTS [19].
In contrast to SE, SWE is an operator-independent advanced elastography technique that enables the objective assessment of tissue stiffness, offering quantitative measurements in kilopascals.
Kantarci et al. observed that MN stiffness was significantly increased in the CTS group (66.7 kPa) compared to controls (32.0 kPa), with even higher values noted in the severe grade (101.4 kPa) compared to mild or moderate grades (55.1 kPa). They recommended a cut-off value of 40.4 kPa to distinguish between cases and controls [22]. Similarly, Cingoz et al. found that CTS patients exhibited higher elasticity values of the MN (53.0 kPa) compared to controls (36.8 kPa), with patients having moderate to severe grades showing even higher elasticity values (82 kPa) than those with mild CTS (44 kPa) [23]. Although these studies, akin to ours, demonstrated significant differences in MN stiffness (in kilopascals) between cases and controls, as well as between CTS subgroups, the cut-off values obtained differed from our study. This discrepancy could be attributed to the fixed ROI of 5 × 5 mm in our study, which was large enough to include perineural tissue and might have influenced the results. Conversely, Park et al.’s study revealed significant inter-group and subgroup differences in elasticity, with the severe subgroup (54.92 kPa) showing a notable increase compared to mild (30.60 kPa) and moderate (34.39 kPa) subgroups. They recommended a cut-off of 26.75 kPa to differentiate CTS cases from controls, similar to our study where a cut-off value greater than 22.3 kPa exhibited the highest validity [24].
Our study had few limitations: To begin with, the size of the ROI utilized in SWE was larger than the dimension of the MN in the axial plane, which could have influenced the results. This discrepancy arose because the minimum area covered within the square ROI on our ultrasound machine was fixed at 5 × 5 mm, which usually exceeded the CSA of the MN, leading to the inclusion of perineural tissue. This inclusion might have contributed to variations in mean values and cut-off values of shear wave elastography compared to other similar studies. Additionally, all measurements on Grey-scale USG and Elastography were conducted in the axial plane at the CTI. Incorporating measurements of the CSA of the MN at multiple sites could have enhanced confidence in the results. Also, the radiologists performing the USG were not blinded to whether the participant was a CTS patient or a control, which might have influenced the CSA measurements. However, to mitigate this potential bias, an average of multiple measurements was taken. Finally, our study did not encompass patients clinically suspected of CTS who exhibited false negative results on NCS. This particular group could potentially benefit the most from imaging modalities.
Despite its limitations, our study, which primarily aimed at determining the efficacy of elastography combined with grey scale ultrasound in grading the severity of CTS, has yielded promising results. Future research encompassing multi-centric studies with larger sample size involving different ethnic groups and collaborating with various ultrasound elastography vendors are necessary to improve accuracy and reproducibility of elastography techniques as well as to establish standardized protocols for image acquisition and interpretation. Furthermore, longitudinal studies are needed to evaluate the prognostic value of elastography in predicting disease progression and treatment outcomes in CTS patients.
To conclude, the MN demonstrated a significant increase in its CSA and stiffness with increasing disease severity in CTS, indicating that the combination of Grey-scale USG and Sono-elastography (especially SWE) is very helpful in grading the severity of CTS and can be used as a painless and cost-effective alternative for NCS, especially in patients presenting with clinical CTS who have conditions that preclude them from undergoing electrophysiological studies.
References
Peterson JJ, Berquist TH. Hand and Wrist. In: Peterson JJ, editor. Berquist’s Musculoskeletal Imaging Companion. 3rd ed. Philadelphia: Wolters Kluwer; 2018. p. 826–7.
De Krom MC, Knipschild PG, Kester AD, Thijs CT, Boekkooi PF, Spaans F. Carpal tunnel syndrome: prevalence in the general population. J Clin Epidemiol. 1992;45(4):373–6.
Witt JC, Hentz JG, Stevens JC. Carpal tunnel syndrome with normal nerve conduction studies. Muscle Nerve. 2004;29(4):515–22.
Wong SM, Griffith JF, Hui AC, Tang A, Wong KS. Discriminatory sonographic criteria for the diagnosis of carpal tunnel syndrome. Arthritis Rheum. 2002;46(7):1914–21.
Mallouhi A, Pültzl P, Trieb T, Piza H, Bodner G. Predictors of carpal tunnel syndrome: accuracy of gray-scale and color Doppler sonography. Am J Roentgenol. 2006;186(5):1240–5.
Pinilla I, Martin-Hervas C, Sordo G, Santiago S. The usefulness of ultrasonography in the diagnosis of carpal tunnel syndrome. J Hand Surg Eur. 2008;33(4):435–9.
Klauser AS, Halpern EJ, De Zordo T, Feuchtner GM, Arora R, Gruber J, et al. Carpal tunnel syndrome assessment with US: value of additional cross-sectional area measurements of the median nerve in patients versus healthy volunteers. Radiology. 2009;250(1):171–7.
Moran L, Perez M, Esteban A, Bellon J, Arranz B, del Cerro M. Sonographic measurement of cross-sectional area of the median nerve in the diagnosis of carpal tunnel syndrome: correlation with nerve conduction studies. J Clin Ultrasound. 2009;37(3):125–31.
Kang S, Kwon HK, Kim KH, Yun HS. Ultrasonography of median nerve and electrophysiologic severity in carpal tunnel syndrome. Ann Rehabil Med. 2012;36(1):72–9.
Azami A, Maleki N, Anari H, Iranparvar Alamdari M, Kalantarhormozi M, Tavosi Z. The diagnostic value of ultrasound compared with nerve conduction velocity in carpal tunnel syndrome. Int J Rheum Dis. 2014;17(6):612–20.
Mourad MA, Kareem HA. Idiopathic carpal tunnel syndrome (ICTS): correlation between nerve conduction studies and dynamic wrist ultrasonography. Egypt J Radiol Nucl Med. 2018;49(4):1060–7.
Pimentel BF, Faloppa F, Tamaoki MJ, Belloti JC. Effectiveness of ultrasonography and nerve conduction studies in the diagnosing of carpal tunnel syndrome: clinical trial on accuracy. BMC Musculoskelet Disord. 2018;19(1):115.
Falsetti P, Conticini E, Baldi C, D’Ignazio E, Al Khayyat SG, Bardelli M, et al. A novel ultrasonographic anthropometric-independent measurement of median nerve swelling in carpal tunnel syndrome: the “nerve/tendon ratio” (NTR). Diagnostics. 2022;12(11):2621.
Zaki HA, Shaban E, Salem W, Bilal F, Fayed M, Hendy M, et al. A comparative analysis between ultrasound and electromyographic and nerve conduction studies in diagnosing carpal tunnel syndrome (CTS): a systematic review and meta-analysis. Cureus. 2022;14(10):e30476.
Tai T-W, Wu C-Y, Su F-C, Chern T-C, Jou I-M. Ultrasonography for diagnosing carpal tunnel syndrome: a meta-analysis of diagnostic test accuracy. Ultrasound Med Biol. 2012;38:1121–8.
Gennisson JL, Deffieux T, Fink M, Tanter M. Ultrasound elastography: principles and techniques. Diagn Interv Imaging. 2013;94(5):487–95.
Jablecki CK, Andary MT, Floeter MK, Miller RG, Quartly CA, Vennix MJ, et al. Practice parameter: electrodiagnostic studies in carpal tunnel syndrome. Neurology. 2002;58(11):1589–92.
Stevens JC. AAEM minimonograph #26: the electrodiagnosis of carpal tunnel syndrome. American Association of Electrodiagnostic Medicine. Muscle Nerve. 1997;20(12):1477–86.
Miyamoto H, Halpern EJ, Kastlunger M, Gabl M, Arora R, Bellmann -Weiler R, et al. Carpal tunnel syndrome: diagnosis by means of median nerve elasticity—improved diagnostic accuracy of US with sonoelastography. Radiology. 2014;270(2):481–6.
Yoshii Y, Ishii T, Tanaka T, Tung WL, Sakai S. Detecting median nerve strain changes with cyclic compression apparatus: a comparison of carpal tunnel syndrome patients and healthy controls. Ultrasound Med Biol. 2015;41(3):669–74.
Asadov R, Erdal A, Buğdaycı O, Gündüz OH, Ekinci G. The effectiveness of ultrasonography and ultrasonographic elastography in the diagnosis of carpal tunnel syndrome and evaluation of treatment response after steroid injection. Eur J Radiol. 2018;108:172–6.
Kantarci F, Ustabasioglu FE, Delil S, Olgun DC, Korkmazer B, Dikici AS, et al. Median nerve stiffness measurement by shear wave elastography: a potential sonographic method in the diagnosis of carpal tunnel syndrome. Eur Radiol. 2014;24(2):434–40.
Cingoz M, Kandemirli SG, Alis DC, Samanci C, Kandemirli GC, Adatepe NU. Evaluation of median nerve by shear wave elastography and diffusion tensor imaging in carpal tunnel syndrome. Eur J Radiol. 2018;101:59–64.
Park EJ, Hahn S, Yi J, Shin KJ, Lee Y, Lee HJ. Comparison of the diagnostic performance of strain elastography and shear wave elastography for the diagnosis of carpal tunnel syndrome. J Med Ultrason. 2021;40(5):1011–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Prakash, A., Vinutha, H., Janardhan, D.C. et al. Diagnostic efficacy of high-frequency Grey-scale ultrasonography and Sono-elastography in grading the severity of carpal tunnel syndrome in comparison to nerve conduction studies. Skeletal Radiol 53, 2399–2408 (2024). https://doi.org/10.1007/s00256-024-04662-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-024-04662-y