Abstract
Objective
To determine if diagnostic ultrasound can reliably distinguish between synovial patterns of prosthetic joint infection and polymeric wear in total knee replacements.
Methods and methods
This retrospective study was approved by our hospital IRB. Using the radiology report database, MR examinations performed within a week of diagnostic ultrasound and/or ultrasound-guided aspiration were identified. This yielded (1) 24 cases with MR and ultrasound comparisons; (2) 44 cases with MR, ultrasound, and aspiration comparisons; and (3) 92 cases with ultrasound and aspiration comparisons. The MR studies were reviewed by a musculoskeletal radiologist. The ultrasound studies were each reviewed by 2 other musculoskeletal radiologists. Each study was graded for synovial pattern indicating infection, polymeric wear, or normal/nonspecific. Agreement between the MR grader and the ultrasound graders as well as ultrasound inter-rater agreement were assessed using k statistics. Sensitivity, specificity, positive predictive value, and negative predictive value of ultrasound were calculated.
Results
Agreement between ultrasound and MR imaging was fair to moderate: k of 0.27 (95% CI: 0.04, 0.50) and 0.44 (95% CI: 0.23, 0.65) for ultrasound raters 1 and 2, respectively. Inter-rater agreement between ultrasound graders 1 and 2 was moderate, with k of 0.56 (95% CI: 0.42, 0.70). Ultrasound sensitivities for infection were 0.13 and 0.09, while specificities were 0.94 and 0.98. Ultrasound sensitivities for polymeric wear were 0.38 and 0.62 with specificities of 0.90 and 0.76.
Conclusion
Ultrasound does not perform well in distinguishing patterns of synovitis either compared to MRI or a reference standard of aspiration/clinical follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Knee arthroplasties are the most commonly performed joint replacement in the USA, with an estimated incidence of over one million per year [1].
Two common causes of total knee replacement (TKR) failure are prosthetic joint infection (PJI) and polyethylene wear, accounting for 27.4% and 3.5% of TKR revisions, respectively, as reported by Sharkey et al. in 2014 [2]. Thiele et al. reported similar findings in 2015, with infection accounting for the greatest number of early TKR failures while polyethylene wear was a common cause of late failure [3].
Imaging evaluation is indicated for evaluation of the symptomatic TKR, consisting primarily of plain radiographs and magnetic resonance (MR) imaging [4]. MR imaging has been validated as a diagnostic tool for both infection and polyethylene wear. Lamellated and hyperintense synovitis, with associated extracapsular soft tissue edema, extracapsular fluid collections, and reactive adenopathy, has been correlated with a high likelihood of an infected implant [5,6,7]. Polyethylene wear is demonstrated by frond-like synovial thickening with intermediate signal-intensity intra-articular debris [5, 6, 8]. At our institution, we perform diagnostic ultrasound prior to ultrasound-guide aspiration of painful TKRs. The purpose of this study is to determine if ultrasound (US) can also accurately differentiate patterns of synovitis associated with infection and polymeric wear in total knee replacements.
Materials and methods
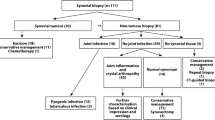
Institutional Review Board approval was obtained for this study consisting of 3 cohorts of patients with painful TKR referred by their orthopedic surgeons for imaging evaluation in the period from January 2018 through September 2020. One cohort had MR imaging and US; another cohort had MR imaging, US, and US-guided aspiration; and the last cohort had US and US-guided aspiration. MR and US studies were performed no more than 7 days apart.
The first cohort comprised 20 patients who underwent both MR and US imaging, 4 of whom were imaged bilaterally, for a total of 24 MR and US comparisons. Some of these patients had been prospectively recruited by phone prior to their scheduled MR study for a same-day research US. Others had been requested for both MRI and diagnostic US by the referring clinician—these cases were identified retrospectively using our institutional radiology report database (mPower, Nuance, Burlington, MA, USA).
Cohort 2 comprised 42 patients, also retrospectively identified using the radiology report database, who had been referred for both MRI and US-guided aspiration, 2 of whom were evaluated bilaterally. Diagnostic US imaging was performed in conjunction with all US-guided aspirations, yielding a total of 44 cases with MR, US, and aspiration comparisons.
An additional retrospectively identified 91 patients had US-guided aspiration without MRI, of whom 1 underwent same-day bilateral knee joint aspirations. This yielded a total of 92 US-guided knee aspirations with concurrent diagnostic US imaging, comprising cohort 3.
A summary of the distribution of examinations in the 3 cohorts is provided in Table 1. Altogether, the 3 cohorts included 153 individuals, of whom 84 were women and 69 were men. The women ranged in age from 36 to 88, with a mean age of 67.0 ± 8.8 (standard deviation) years. The men ranged in age from 31 to 83, with a mean age of 65.8 ± 9.8 years. The combined mean age was 66.4 ± 9.3 years.
The diagnostic US in all cohorts consisted of grey scale cine clips and static images of the entire suprapatellar recess and parapatellar gutters in short and long axis, in order to evaluate the entire synovium in planes analogous to axial and sagittal MR imaging. Power Doppler imaging was also used in 132 of the 149 US studies. The images were obtained by any of 8 musculoskeletal sonographers who underwent practice scanning of the technique prior to patient enrollment. Imaging was performed on a GE Logiq E9 unit (GE Healthcare, Chicago, IL, USA) with either a 6–15 MHz or 9 MHz linear probe or a Samsung R85 unit (Boston Imaging, Danvers, MA, USA) using a 3–12 MHz linear probe.
MR imaging was performed with 1.5-T clinical imaging units (GE Healthcare, Waukesha, WI, USA) using eight-channel phased-array transmit-receive knee coils (In Vivo, Orlando, FL, USA). The MR protocols utilized are the standard of care at our institution, including fast spin echo (FSE) pulse sequences optimized for metal (with a high receiver bandwidth of 488 Hz/pixel) in the axial, sagittal, and coronal planes, as well as 3-dimensional multi-spectral imaging (3D MSI) techniques to minimize metal artifact. The 3D MSI techniques used were either multi-acquisition variable resonance image combination selective (MAVRIC SL, GE Healthcare) in the sagittal and (optionally) axial planes or HyperMAVRIC SL (GE Healthcare) in the sagittal plane enabled by the acquisition of a HyperMAVRIC SL spectral calibration sequence. The studies that were performed earlier in our patient sample used the non-isotropic MAVRIC SL technique, while the studies performed later used the isotropic HyperMAVRIC SL technique. This reflects the evolution of GE Healthcare technology used at our institution. Each study also included a sagittal fluid-sensitive sequence utilizing the MAVRIC SL inversion recovery (IR) technique. A representative summary of the MR pulse sequence protocol used is provided in Table 2.
The MR examinations were reviewed by a fellowship-trained musculoskeletal radiologist with 10 years of experience in MRI of arthroplasty, using a synovial pattern grading system consisting of 3 categories: lamellated, polymeric, or normal/nonspecific. A similar grading system has been previously used in the literature to assess MR imaging patterns of synovitis [6].
The US studies were independently reviewed by 2 fellowship-trained musculoskeletal radiologists with 8 and 25 years of experience in both musculoskeletal ultrasound and MRI, who were blinded to the MR appearance and the clinical outcome. The synovial patterns were also graded as lamellated, polymeric, or normal/nonspecific, in order to correlate with similar appearances of synovium on MRI. The lamellated appearance, indicating infection, consisted of multilayered synovial thickening, while polymeric wear consisted of bulky and frondular synovial thickening, with or without punctate echogenic foci of polyethylene debris. If the synovial pattern appeared to be neither lamellated nor polymeric, a grading of normal/nonspecific was used. Each US study was also assessed for degree of power doppler hyperemia, with grades of none, mild (one or two scattered foci of hyperemia within the synovium), moderate (three or four foci), and marked (diffuse hyperemia throughout the synovium).
The MR studies were anonymized prior to grading. The US studies, however, contained patient identifiers which were embedded into both the still and cine images and were unable to be anonymized. Nonetheless, each reader was blinded to the interpretations of the other readers and blinded to the appearances on the other imaging modality, and the grades were collected and compiled by a 4th musculoskeletal radiologist.
Data, including patient age, gender, date of examination, and synovial pattern determined by each reader, were recorded. A review of the electronic medical record was performed for all the patients to determine the results of culture, whether from US aspiration or subsequent surgical sampling, as well as the pathology for which the patient was ultimately treated. Statistical analysis was performed by a dedicated biostatistician. The data from cohorts 1 and 2 were analyzed to determine agreement between the MR grader and the US graders using kappa coefficient (k) statistics. The data from cohorts 2 and 3 were analyzed to determine (1) inter-rater agreement between the US graders using k statistics and (2) sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of US relative to aspirate results/clinical follow-up using epiR package. Fisher’s exact test was used to assess for association between degree of hyperemia and US aspiration/clinical determination of infection or polymeric wear. Continuous variables were represented using means and standard deviations, and categorical variables were expressed as proportions. All statistical analyses were performed using R (version 4.0.3, R Foundation for Statistical Computing, Vienna, Austria).
Results
Cohorts 1 and 2, numbering a total of 68 cases that underwent both MR and US imaging, had 6 knees which were graded as having lamellated synovium on MRI, of which only 1 was identified as lamellated on US, with both US graders concurring on a lamellated synovial appearance in this patient (Fig. 1). No case was called lamellated by US that was determined to be normal/nonspecific on MRI.
Fifty-five-year-old man status post left TKR with draining anterior wound. a Axial intermediate-weighted FSE image through the suprapatellar joint recess demonstrates hyperintense and lamellated synovium (arrows), reflecting infection. b US image from a cine clip through the lateral suprapatellar recess in the axial plane, obtained on the same day as the MR examination, demonstrating a synovial appearance interpreted by both US graders as lamellated (arrows). This patient underwent both MRI and US-guided joint aspiration, yielding cultures positive for Staphylococcus epidermidis
Twelve knees were graded as having a polymeric synovial appearance on MRI, of which 4 were judged to be polymeric by US grader 1 and 8 were judged to be polymeric by US grader 2. Four cases were concordant across all 3 graders as having a polymeric pattern (one of these is shown in Fig. 2). Of note, 9 cases that were judged by at least one US grader to be polymeric were deemed normal/nonspecific by MRI. Examples of discordant grading are provided in Figs. 3 and 4.
Seventy-six-year-old man status post right TKR with knee pain. a Axial intermediate-weighted FSE image through the suprapatellar joint recess demonstrates frondlike synovial thickening (arrows) in the lateral suprapatellar recess, reflecting synovitis from polymeric wear. b Image from a same-day US cine clip in the axial plane through the lateral suprapatellar recess shows the US correlate with bulky and nodular synovium (arrows), interpreted as polymeric wear by both US graders
Eighty-three-year-old woman status post right TKR with lateral-sided pain. a Axial intermediate-weighted FSE image through the suprapatellar recess demonstrates synovial thickening (arrow) which was determined to be nonspecific by the MR grader. b Axial US image from the study acquired the prior day was judged to be polymeric by both ultrasound graders
Sixty-seven-year-old man status post right TKR with knee pain. a, b Axial intermediate-weighted FSE image through the suprapatellar joint recess (a) demonstrates marked synovitis judged as hyperintense and lamellated (arrows) on MR imaging, but with US (b) acquired 6 days prior showing synovitis characterized as nonspecific by US grader 1 and polymeric by US grader 2
Agreement between US and MRI was fair to moderate: for US grader 1, k was 0.27 (95% CI: 0.04, 0.50), and for US grader 2, k was 0.44 (95% CI: 0.23, 0.65).
On follow-up of aspiration results and/or clinical course for cohorts 1 and 2, 9 cases were infected, of which 5 had been judged to have a lamellated appearance on MRI, 3 had nonspecific synovial thickening, and 1 had a polymeric pattern. Of the remaining non-infected cases, 22 underwent surgical revision for a variety of abnormalities, most commonly including aseptic loosening, instability, and arthrofibrosis. An additional 6 underwent arthroscopic debridement/lysis for arthrofibrosis.
Cohorts 2 and 3 yielded 136 cases that underwent US-guided aspiration with concurrent diagnostic US imaging. Of these, 18 cases demonstrated positive cultures. The bacteria grown from joint fluid culture for these patients consisted of Staphylococcus epidermidis (8 cases), Staphylococcus aureus (3 cases), Enterococcus faecalis (2 cases), Staphylococcus lugdunensis (1 case), Streptococcus mitis (1 case), and Streptococcus agalactiae (1 case). Cutibacterium acnes (previously Propionibacterium acnes) was cultured in 2 cases, but both of these were clinically felt to be false positive results. Eight cases that were culture negative on US-guided joint aspiration were clinically felt to be infected and treated as such, with 1 of these subsequently growing Staphylococcus aureus on operative wound culture. Thus, there were a total of 26 cases that were considered truly infected following joint aspiration. Only 3 of these truly infected cases were judged to be lamellated in appearance by both US graders, including the case that was concordant for lamellation by MR examination (as described above and in Fig. 1).
Of the 136 knees that underwent US-guided aspiration, 2 were excluded from analysis as they were on chronic antibiotic suppression. Three other knees were excluded from analysis due to having been rated as indeterminate between lamellated and polymeric patterns by one of the US graders. Six knees had no subsequent clinical follow-up or had an unclear clinical picture; these were counted as not infected based on negative cultures and were also assumed to be negative for polymeric wear as they never returned for surgical revision. Eight knees were determined to have polymeric wear by clinical follow-up, of which 5 were judged to have a polymeric pattern by at least one US grader. Inter-rater agreement between US graders 1 and 2 was moderate, with k of 0.56 (95% CI: 0.42, 0.70). Sensitivity and specificity of US for infection were 0.13 and 0.94 for grader 1, with PPV and NPV of 0.30 and 0.83; grader 2 had a sensitivity and specificity of 0.09 and 0.98, with PPV and NPV of 0.50 and 0.83. For polymeric wear, sensitivity and specificity of US were 0.38 and 0.90 for grader 1, with PPV and NPV of 0.20 and 0.96; sensitivity and specificity for US grader 2 were 0.62 and 0.76, with PPV and NPV of 0.14 and 0.97. These results are summarized in Table 3.
Fisher’s exact test yielded no significant association between degree of US hyperemia and aspiration/clinical determination of infection or polymeric wear (p-value of 0.622 for US grader 1 and 0.154 for US grader 2).
Discussion
Due to its multiplanar capabilities, metal artifact suppression techniques, and excellent soft tissue contrast, MRI has become a valuable diagnostic tool in the evaluation of the painful total knee replacement. It has proven to be accurate in the detection of bone loss around implant components, osteolysis, polyethylene wear, infection, and arthrofibrosis [5,6,7,8].
The strengths of US include high spatial resolution and the ability to image the soft tissues close to metal without being confounded by artifact. US evaluation can also be performed more rapidly than MRI and can be performed without concern for contraindications. However, compared to MRI, US does not perform well in assessing infectious or polymeric synovitis, with poor sensitivity and PPV. The fair to moderate agreement on synovial appearance between US grading and MR grading indicates that US cannot be used as an alternative for MRI to differentiate synovial patterns. NPV for both US graders was high for infection and polymeric wear, but this is likely due to the overall low rate of these in the sample population. Specificity was also high for both US graders for infection and polymeric synovitis, suggesting that US may be a useful tool for ruling in these pathologies. However, given its low sensitivity and PPV, US cannot be recommended as a useful modality for the detection of infection or polymeric wear after TKR.
Although US can identify joint effusions, synovial thickening, and hyperemia, these findings in and of themselves are not indicative of the underlying pathology. Other findings in the joint may render the diagnosis in certain instances, for example, as shown in a 2019 case report wherein sonography demonstrated a displaced polyethylene liner as well as echogenic shadowing debris in the synovium indicating metallosis [9]. However, our study concludes that, in general, PJI and polyethylene wear cannot be reliably discerned based on characteristics of the synovitis, including the morphology of the thickened synovium. The difference in performance between US and MRI is probably related to the poorer contrast resolution of US compared to MRI. Additionally, even though the US diagnostic protocol using cine clips in axial and longitudinal planes was designed to mimic MR imaging planes, US remains operator-dependent to capture the entirety of the synovium. MRI also will of course reveal findings beyond the boundaries of the suprapatellar and parapatellar synovium, including extra-capsular soft tissue edema and sinus tracts which, if present, would suggest infection to the MRI reader but may not be captured on the US cine images. Another factor contributing to the poorer performance of US in this study may be simply misinterpretation by the US readers, as demonstrated in Fig. 4b wherein, retrospectively, the authors are of the opinion that the US appearance should have been interpreted as lamellated rather than nonspecific or polymeric and therefore should have agreed with the MRI.
Limitations of this study include the low numbers of truly infected and truly polymeric cases in our sample (26 and 8 respectively, of 136 cases in cohorts 2 and 3). Another limitation is the lack of anonymization of the US studies, which theoretically could have biased the US grading if the US readers had previously encountered the study patients in their clinical work and recalled their clinical presentation/follow-up. However, grading was performed over 6 months after the last included US study was performed, so the risk of this bias is low.
In summary, MR imaging characteristics of synovitis cannot be transferred to US. While we had hoped that the distinctive MRI morphologic characteristics of synovitis seen in PJI and polyethylene wear would be apparent on US, this was not borne out by our analysis.
References
Singh JA, Yu S, Chen L, Cleveland JD. Rates of total joint replacement in the United States: future projections to 2020-2040 using the national inpatient sample. J Rheumatology. 2019;46:1134–40.
Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today—has anything changed after 10 years? J Arthroplasty. 2014;29:1774–8.
Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R. Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. JBJS. 2015;97:715–20.
Miller TT. Imaging of knee arthroplasty. Eur J Radiol. 2005;54:164–77.
Fritz J, Lurie B, Potter HG. MR imaging of knee arthroplasty implants. Radiographics. 2015;35:1483–501.
Li AE, Sneag DB, Greditzer HG IV, Johnson CC, Miller TT, Potter HG. Total knee arthroplasty: diagnostic accuracy of patterns of synovitis at MR imaging. Radiology. 2016;281:499–506.
Plodkowski AJ, Hayter CL, Miller TT, Nguyen JT, Potter HG. Lamellated hyperintense synovitis: potential MR imaging sign of an infected knee arthroplasty. Radiology. 2013;266:256–60.
Li AE, Johnson CC, Sneag DB, et al. Frondlike synovitis on MRI and correlation with polyethylene surface damage of total knee arthroplasty. AJR. 2017;209(4):231–7.
Mallon S, Bussis K, Beswick Z, North WT, Soliman SB. Ultrasonographic and radiographic findings of polyethylene component displacement with severe metallosis and metal-induced synovitis following total knee arthroplasty. The Knee. 2019;26(4):941–50.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, J., Burge, A., Li, Q. et al. Ultrasound assessment of synovitis in total knee replacements: concordance with MR imaging and joint aspiration. Skeletal Radiol 53, 863–869 (2024). https://doi.org/10.1007/s00256-023-04485-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-023-04485-3