Abstract
Objective
To demonstrate the degrees of occult intertrochanteric extension on MRI in patients with a greater trochanteric fracture on radiography or computer tomography (CT) and whether these patients undergo conservative or surgical management with hardware.
Materials and methods
Retrospective review was performed of 146 patients (104 females, 42 males, ages 33–102) who had follow-up MRI after identification of a greater trochanteric fracture without intertrochanteric extension on radiography or CT. Extent of intertrochanteric extension was recorded. Subsequently, EMR review was performed to see if patients underwent surgery. Specific note was made of hardware type. Analysis was performed to determine if there is a correlation with fracture type and surgical management as well as fracture type and age and gender.
Results
Nineteen patients had horizontal greater trochanter fractures without intertrochanteric extension; none underwent surgery. Seventeen patients had a vertical fracture along the lateral femoral cortex; one underwent surgery. Thirty-three patients had a fracture with intertrochanteric extension less than 50% in the mid coronal plane; 21 underwent surgery. Forty patients had intertrochanteric extension greater than 50% in the midcoronal plane not contacting the medial cortex; 28 underwent surgery. Thirty-seven patients had fractures contacting the medial cortex; 28 underwent surgery. There was significant difference with fractures extending 50% or greater of the midline of the intertrochanteric region undergoing surgical management compared with fractures less than 50% (p < 0.0001).
Conclusion
MRI identifies the presence and extent of occult intertrochanteric fractures in patients with greater trochanteric fractures. Description of intertrochanteric fractures on MRI helps determine the patient’s treatment course and influence surgical decisions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
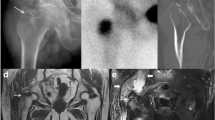
More than 300,000 people in the USA each year sustain a hip fracture [1]. Intertrochanteric fractures account for approximately 38–50% of all hip fractures with an overall annual cost of $2.63 billion to the US Healthcare system (Fig. 1). This corresponds to 44% of all hip fracture costs [2, 3]. As previously described in the literature, intertrochanteric fractures can be occult, presenting as isolated greater trochanteric fractures without evidence of obvious intertrochanteric extension on radiography and computed tomography (CT) but with some degree of intertrochanteric extension present on magnetic resonance imaging (MRI) [4,5,6,7,8] (Fig. 2). MRI is frequently used to assess for occult intertrochanteric extension as a decision-making tool in clinical management. Few studies cite a fracture line crossing greater than 50% of the intertrochanteric region, a finding that may influence the clinical team to pursue surgical management rather than conservative management [5, 9]. Fixation of intertrochanteric fractures improves pain and decreased time of immobilization [10,11,12].
84-year-old-male status post fall with left hip radiograph (a) showing subtle cortical disruption of the greater trochanter (white arrow) and lucency through the intertrochanteric region (white dashed arrow). Subsequently performed coronal CT images (b, c) show the greater trochanter fracture (white arrow) and intertrochanteric extension (white dashed arrow)
83-year-old-female status post fall with left hip radiograph (a) and Coronal CT image (b) demonstrating a greater trochanteric fracture without evidence of intertrochanteric extension. Subsequently performed coronal T1 MRI (c) through the posterior aspect of the intertrochanteric region shows greater trochanteric fracture and intertrochanteric extension
Nondisplaced intertrochanteric fractures are considered stable fractures [13, 14]. In cases of complete two-part intertrochanteric fractures (AO 31-A1.2), the fracture line extends to the medial cortex and calcar femorale, which are connected [13, 15]. The calcar femorale is a vertically oriented dense portion of bone that extends laterally from the posterior medial femoral neck cortex at about the mid-level of the lesser trochanter (Fig. 3) [15]. The calcar femorale is an important weight bearing and stabilizing component of the hip [16,17,18]. Comminution of the posteromedial cortex or calcar femorale advances an intertrochanteric fracture to unstable [13, 14]. Several classification methods exist for different types of intertrochanteric fractures including but not limited to Evans, Jensen Modification of Evans, Kyle, Boyd and Griffin and AO Foundation/Orthopedic Trauma Association (AO/OTA) (Table 1) [19,20,21,22].
When surgery is indicated, hardware options most commonly include dynamic hip screws, short intramedullary nails, and long intramedullary nails. Arthroplasty has been used in specific scenarios, such as if the patient simultaneously has arthrosis and would be indicated for an arthroplasty regardless. Several articles in the orthopedic literature have attempted to establish whether intramedullary or extramedullary fixation is superior. At this juncture, surgeon preference and case specifics guide technique and hardware selection [10, 18].
The purpose of this study is to categorize the degree of intertrochanteric extension on MRI in patients diagnosed with isolated greater trochanteric fractures without evidence of intertrochanteric extension on radiography or CT. The objective is to determine if the categories predict which patients undergo conservative management versus surgical fixation.
Materials and methods
Patient cohort
IRB approved retrospective analysis was performed. A search was conducted of patients who underwent MRI for assessment of occult intertrochanteric extension of an isolated greater trochanter fracture identified on radiography or CT, within 4 weeks of initial presentation, over a 5-year period from 2013 to 2018. Patients were excluded if an incomplete or incorrect protocol was performed, if hardware was present in the injured femur or if follow-up was not available as to whether the patient underwent conservative versus operative management. Patients were excluded if intertrochanteric extension was evident on previously performed radiography or computer tomography (CT). A total of 185 patients were identified through the search. Thirty-nine patients were excluded and 146 patients were included.
Imaging
Exams were identified in multiple hospitals and few outpatient imaging centers within our health system on either a 1.5 T or a 3 T MRI scanner. Patients underwent a standard institutional trauma protocol MRI, which consists of a coronal T1 and axial T1 (TR/TE range, 400–800/minimum) as well as coronal and axial T2 Fat Saturated (TR/TE range, > 2000/80–120) or STIR (TR/TE range, > 2000/20–60, IR 150–180) sequences. Additional parameters included 140–440 FOV, 256–512 × 256–512 matrix range, and 4- to 5-mm slice thickness. Whole pelvic imaging was performed; some cases included additional unilateral hip sequences with a smaller field of view.
Image analysis
Two musculoskeletal trained radiologists reviewed the MRIs in consensus and categorized the degree of intertrochanteric (IT) extension. Categories included the following: (1) isolated greater trochanteric fracture-horizontal line through the greater trochanter (Fig. 4); (2) vertically oriented fracture-vertical fracture line that parallels the lateral greater trochanter and femoral cortex (Fig. 5); (3) IT extension less than 50% of the midline of the femur in the coronal plane (Fig. 6); (4) IT extension equal to or greater than 50% of the midline of the femur in the coronal plane, not contacting the calcar or medial cortex (Fig. 7); (5) IT extension greater than 50% of the midline of the femur in the coronal plane, contacting the calcar or medial cortex (Fig. 8). The center of the femoral shaft was determined with a line extending proximally into the intertrochanteric region to establish the midline. T1 and fluid sensitive sequences were both assessed with definition of fracture as linear or curvilinear T1 hypointensity with adjacent marrow edema. Radiologists were blinded to what type of management the patient underwent during this process.
Subsequently, chart review was performed to identify whether patients underwent non-surgical versus surgical management and if rationale was documented as to why, including contraindications to surgery. Of the patients who underwent surgery, the type of hardware fixation was documented.
Statistical analysis
Demographic patient data and imaging locations were recorded. Mean and median calculations were performed for ages within each fracture category. Using the data obtained from the two interpreting radiologists, frequency analysis of each fracture category was performed. Frequency percentages were calculated for (1) if the patient underwent surgery, (2) if the patient was indicated for surgery but did not undergo surgery (whether due to patient refusal, comorbidities or delayed diagnosis), and (3) what type of hardware the patient was treated with (dynamic hip screw, short intramedullary rod, long intramedullary rod or hip arthroplasty). Statistical significance utilizing chi-square test was performed to analyze the relationship between intertrochanteric fractures less than 50% versus 50% or greater with regards to age, gender and if patient underwent surgical management. An observed p-value less than 0.05 was considered statistically significant. All analyses were conducted using SAS, release 3.8 enterprise edition. Copyright 2012–2018, SAS Institute Inc., Cary. NC.
Results
A total of 146 patients were included in the study with 104 female (71%) and 42 male (29%) patients. The mean age was 81 years old (range 33–102) (Table 2). All patients were diagnosed with a greater trochanter fracture either on radiography or CT without evidence of intertrochanteric extension. Follow-up MRI was performed on all patients. The majority of these patients, 136, were imaged during an Emergency Department visit or as an inpatient and 10 patients were imaged in the outpatient setting. Nineteen patients (13%) on MRI were shown to have an isolated greater trochanter fracture without intertrochanteric extension. All 19 patients were managed conservatively and none was recommended for surgery. Seventeen patients (12%) had vertically oriented fractures that coursed parallel to the greater trochanter and lateral femoral cortex. Of these cases, one patient underwent surgery with a short intramedullary rod. Two patients were indicated for surgery, but were not operated on secondary to concurrent injuries precluding operative management. The remaining 14 patients were not indicated for surgery. Thirty-three patients (23%) were found to have intertrochanteric extension that did not cross greater than 50% in the coronal plane. Of these cases, 21 underwent surgical management with seven dynamic hip screws, 13 short intramedullary rod, and one long intramedullary rod. Twelve of these patients did not undergo surgery, though one patient was recommended for surgery; however, the family declined. Forty patients (27%) had fracture extension 50% or greater than the midline of the intertrochanteric region in the coronal plane but did not contact the calcar femorale or medial cortex. Of this subgroup, 28 patients underwent surgical management with four dynamic hip screws, 16 short intramedullary rods, and seven long intramedullary rods. One patient underwent a hip arthroplasty as the patient had severe arthrosis. Twelve patients were managed conservatively of which three were indicated for surgery but were not performed due to high operative risk (two patients) or delayed diagnosis (one patient diagnosed 8 days later imaged as an outpatient). The final group where the fracture extends to the calcar or medial cortex had a total of 37 patients (25%) of which 28 underwent surgical management with five dynamic hip screws, 16 short intramedullary rods, and seven long intramedullary rods. Nine patients did not undergo surgery, of which seven did not have surgery secondary to high operative risk (four patients), delayed diagnosis (two patients, 12 and 25 days after initial presentation), or patient refusal (one patient).
Analysis of surgical and non-surgical management was performed with patients grouped into two categories of (1) all fractures which extend less than 50% of the intertrochanteric region (Figs. 4, 5, and 6 described in the “Image analysis” section) and (2) all fractures equal to or greater than 50% of the intertrochanteric region (Figs. 7 and 8 described in the “Image analysis” section). Chi-square test was performed, which demonstrated significant association between surgery status and fracture group (p < 0.0001) among patients who underwent surgery, the proportion of patients with fractures 50% or greater intertrochanteric extension (Figs. 7 and 8) is significantly greater than the proportion of patients with fractures less than 50% of intertrochanteric extension (Figs. 4, 5, and 6) (72.7% versus 31.9%, respectively; p < 0.0001). There is no association of fractures with less than or equal to/greater than 50% of intertrochanteric extension with respect to gender or age utilizing chi-square test (p = 0.7558 and p = 9567 respectively).
Of female gender, 57 patients underwent surgery and 47 did not undergo surgery. Of male gender, 21 underwent surgery and 21 did not undergo surgery. Using the chi-square test, no association was found between gender and whether a patient underwent surgery (p = 0.5981).
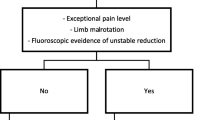
Discussion
Our results show that in the setting of a greater trochanteric fracture, as the fracture line propagates across the intertrochanteric region toward the posteromedial cortex or calcar femorale, the patient is more likely to undergo surgical management. Fracture lines which cross beyond 50% of the intertrochanteric region are typically indicated for surgical management pending no interfering comorbidities, delayed diagnosis, or agreement by the patient or family. Of the fractures that extend toward the midline but do not cross than 50% of the intertrochanteric region, the majority of patients underwent surgical management. Short intramedullary rod was the most chosen hardware for surgical fixation. While more female than males presented with these fractures, there was no statistical significance with regard to gender and undergoing surgical management.
Intertrochanteric fractures are extracapsular and do not disrupt blood supply to the femoral head, and, therefore, are not associated with avascular necrosis [4]. The fractures discussed in our study are zero and two-part nondisplaced fractures, which are considered stable [14]. Intertrochanteric fractures undergo fixation to allow for pain relief and earlier mobilization and weight bearing [11]. No formal algorithm exists for the fixation of stable intertrochanteric fractures; however, several articles from the literature note if the fracture extends beyond 50% in the longitudinal axis of the coronal plane of the intertrochanteric region, then surgery is indicated [5, 9]. In Feldman and Staron, their article noted that the prime criterion for performing surgery was extension of the fracture line beyond the base of the greater trochanter, regardless of propagation pattern [7]. In an article by Park et al., if the fracture did not propagate to the medial third of the intertrochanteric region or medial cortex, conservative management was performed with full weight-bearing permitted after 4–6 weeks, depending on the extent of the fracture [23]. There is a potential risk for a fracture to become displaced if not fixed, such as with another fall.
Schultz et al. looked at “incomplete intertrochanteric fractures” and management in a similar fashion illustrating the entity that intertrochanteric extension does not always extend to the medial cortex or calcar femorale. Similarly to our study, as the fracture extended further in the mid-coronal plane, more patients underwent surgical fixation [5]. Our study shows in some cases if there is intertrochanteric extension less than 50% of the mid-coronal plane, surgical fixation can be considered a course of management in the appropriate clinical setting, of which 65% of the patients in our group C underwent fixation. No formal algorithm to date is present within the orthopedic literature regarding the fixations of fractures with intertrochanteric extension less than 50% in the mid coronal plane.
Of the patients in the study by Schultz et al., the patients who underwent surgical fixation were all treated with a sliding compression screw [5]. Intramedullary nails, long and short, were more commonly used in our study than dynamic hip screws, which may reflect a change in treatment options over time. Studies in the orthopedic literature discuss these treatment options, but ultimately it is surgeon’s preference [10,11,12, 18, 24]. Similarly, the mean age was 82 in their study and in our study is 81, unsurprisingly with female preponderance. In an article by Feldman and Staron, the fracture patterns described were similar to what we saw with the exception of propagation of the fracture into the femoral neck, which one patient in the study by Craig et al. also demonstrated [7, 9]. Extension of the fracture into the femoral neck is a possibility and is important to document. In our study, category B is propagation of the fracture line in a vertical fashion, which in some cases may be considered to extend beyond the base of the greater trochanter, but does not appear to trend toward the midline. In our experience, 82% of this group were not recommended for surgery and were managed conservatively. In a study by Park et al., the intertrochanteric region was divided into thirds. Their group 1 consisted of patients such as in our groups A and B; their group was managed conservatively. Their group 2 consisted of patients with fractures extending to the middle third of the intertrochanteric region, which would consist of some of our group C and D patients. Their group 2 underwent conservative management, while the majority of our patients underwent surgical fixation. Their group 3 consisted of patients where the fracture extends to the distal third of the intertrochanteric region or to the medial cortex. This is similar to some of our group D and group E patients. Similarly, these patients underwent operative management [23].
In some cases, fixation is performed for isolated greater trochanteric fractures with tension band wiring or trochanteric stabilizing plates [25]. We did not encounter this scenario in our patients. It is important to note that intertrochanteric fractures can occur without an obvious greater trochanter fracture on radiography and CT. This is one of several entities that may warrant an MRI in the setting of a “negative” CT or radiograph.
Limitations of the study include retrospective analysis from 13 institutions across the health system, which resulted in some variability, though exams lacking coronal and axial T1 and fluid sensitive sequences were excluded. Formal measurements were not performed as this can result in variability across observers. Depiction of where the fracture line ends can potentially be subjective. We did not document the long-term outcomes or readmissions. Individual surgeon’s choices for operative versus non-operative management were not recorded. Future research may include assessment of morphology of the greater trochanteric fracture itself identified on radiography and CT, which was not assessed in this study. A study focusing on the short- and long-term outcomes of patients who underwent surgery versus no surgery, especially of fractures with intertrochanteric extension less than 50% would be beneficial in guiding management of these nondisplaced intertrochanteric fractures.
In conclusion, MRI frequently detects occult intertrochanteric extension in patients with isolated greater trochanter fractures on radiography and CT. Given the number of patients who underwent surgical management with intertrochanteric extension, including less than 50% of the intertrochanteric region, MRI in patients with greater trochanteric fractures without evidence of intertrochanteric extension on radiography of computed tomography (CT) is recommended. The extent of intertrochanteric extension can vary. Communication with the surgical team is important to establish what findings and terminology will determine if the patient is indicated for surgery and what type of hardware to use.
References
Hip Fractures Among Older Adults [Internet]. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention; 2016 [cited 2021Feb14]. Available from: https://www.cdc.gov/homeandrecreationalsafety/falls/adulthipfx.html
Simon Mears MD. Fixing Hip Fractures [Internet]. Johns Hopkins Medicine, based in Baltimore, Maryland. 2017 [cited 2021Feb14]. Available from: https://www.hopkinsmedicine.org/gec/series/fixing_hip_fractures#intertrochanteric_fractures
Adeyemi A, Delhougne G. Incidence and economic burden of intertrochanteric fracture: a medicare claims database analysis. JB JS Open Access. 2019;4(1):e0045.
Alam A, Willett K, Ostlere S. The MRI diagnosis and management of incomplete intertrochanteric fractures of the femur. J Bone Joint Surg Br. 2005;87-B(9):1253–5.
Schultz E, Miller TT, Boruchov SD, Schmell EB, Toledano B. Incomplete intertrochanteric fractures: imaging features and clinical management. Radiology. 1999;211(1):237–40.
Pandey R, Mcnally E, Ali A, Bulstrode C. The role of MRI in the diagnosis of occult hip fractures. Injury. 1998;29(1):61–3.
Feldman F, Staron RB. MRI of seemingly isolated greater trochanteric fractures. Am J Roentgenol. 2004;183(2):323–9.
Noh J, Lee KH, Jung S, Hwang S. The frequency of occult intertrochanteric fractures among individuals with isolated greater trochanteric fractures. Hip Pelvis. 2019;31(1):23.
Craig JG, Moed BR, Eyler WR, Holsbeeck MV. Fractures of the greater trochanter: intertrochanteric extension shown by MR imaging. Skeletal Radiol. 2000;29(10):572–6.
Adam P. Treatment of recent trochanteric fracture in adults. Orthop Traumatol Surg Res. 2014;100(1 Suppl):S75–S83.
Management of Acute Hip Fracture. N Engl J Med. 2018;378(10):971–2.
Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR. Implant options for the treatment of intertrochanteric fractures of the hip. Bone Joint J. 2017;99-B(1):128–33.
Sharma G, Gn KK, Khatri K, Singh R, Gamanagatti S, Sharma V. Morphology of the posteromedial fragment in pertrochanteric fractures: a three-dimensional computed tomography analysis. Injury. 2017;48(2):419–31.
Meinberg E, Agel J, Roberts C, Karam M, Kellam J. Fracture and Dislocation Classification Compendium—2018. J Orthop Trauma. 2018;32:S1–167.
Stiehl JB, Jacobson D, Carrera G. Morphological analysis of the proximal femur using quantitative computed tomography. Int Orthop. 2006;31(3):287–92.
Griffin JB. The calcar femorale redefined. Clin Orthop Relat Res. 1982;(164):211–214.
Sheehan SE, Shyu JY, Weaver MJ, Sodickson AD, Khurana B. Proximal femoral fractures: what the orthopedic surgeon wants to know. Radiographics. 2015;35(5):1563–84.
Zhang Y, Zhang S, Wang S, Zhang H, Zhang W, Liu P, et al. Long and short intramedullary nails for fixation of intertrochanteric femur fractures (OTA 31–A1, A2 and A3): a systematic review and meta-analysis. Orthop Traumatol Surg Res. 2017;103(5):685–90.
Evans EM. the treatment of trochanteric fractures of the femur. J Bone Joint Surg Br. 1949;31-B(2):190–203.
Jensen JS. Classification of Trochanteric Fractures. Acta Orthop Scand. 1980;51(1–6):803–10.
Boyd HB. Classification and treatment of trochanteric fractures. Arch Surg. 1949;58(6):853.
Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg. 1979;61(2):216–21.
Park JH, Shon HC, Chang JS, Kim C-H, Byun S-E, Han BR, et al. How can MRI change the treatment strategy in apparently isolated greater trochanteric fracture? Injury. 2018;49(4):824–8.
Egol KA, Marcano AI, Lewis L, Tejwani NC, Mclaurin TM, Davidovitch RI. Can the use of an evidence-based algorithm for the treatment of intertrochanteric fractures of the hip maintain quality at a reduced cost? Bone Joint J. 2014;96-B(9):1192–7.
Chung PH, Kang S, Kim JP, Kim YS, Lee HM, Back IH, et al. Occult intertrochanteric fracture mimicking the fracture of greater trochanter. Hip & Pelvis. 2016;28(2):112.
Acknowledgements
We would like to thank Dr. Myriam Kline for statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Walsh, P.J., Farooq, M. & Walz, D.M. Occult fracture propagation in patients with isolated greater trochanteric fractures: patterns and management. Skeletal Radiol 51, 1391–1398 (2022). https://doi.org/10.1007/s00256-021-03965-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03965-8