Abstract
Objective
Although radiofrequency ablation is well validated for treatment of osteoid osteoma, newer technologies, namely cryoablation, have been less thoroughly studied. The purpose is to perform a systematic review and pooled analysis of percutaneous ablation technologies for treatment of osteoid osteoma with subset analysis of intra-articular and spinal tumors.
Material and methods
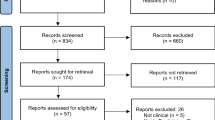
A total of 36 of 79 identified manuscripts met inclusion criteria, comprising 1863 ablations in 1798 patients. Inclusion criteria were (1) retrospective or prospective analysis of thermal ablation of osteoid osteomas in any location, (2) at least 6 months of clinical follow-up, (3) 10 or more patients, (4) patients not included in a second study included in this review, and (5) English language or English translation available. Success rate was defined as all ablations minus technical failures, clinical failures, and recurrences. Subset analysis of intra-articular and spinal tumors was performed.
Results
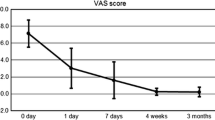
Overall success rate was 91.9% (95% CI 91–93%). Technical failure, clinical failure, and recurrence rates were 0.3%, 2.1%, and 5.6% respectively. Complications were seen in 2.5% (95% CI 1.9–3.3%) patients. There was no significant difference when comparing radiofrequency ablation and cryoablation (p = 0.92). Success rates for intra-articular (radiofrequency ablation) and spinal tumors (radiofrequency and cryoablation) were 97% and 91.6% respectively.
Conclusion
Percutaneous ablation of osteoid osteomas was highly successful with low complication rates. Efficacy of radiofrequency ablation and cryoablation is similar, which is consequential because cryoablation is associated with decreased pain, predictable nerve regeneration, and theoretical immunotherapy benefits. Treatment of more challenging intra-articular and spinal lesions demonstrated similarly high success and low complication rates.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoid osteoma (OO) is a benign bone tumor that represents 5% of all bone tumors [1,2,3]. They usually present in the second decade of life, most commonly before the age of 20 [1]. OOs typically occur in the long bones, particularly in the lower extremities, but less frequently can occur in the axial skeleton. Although most OOs are extra-articular, some can be intra-articular, most commonly affecting the hip joint. The most frequent presenting symptom is chronic nocturnal pain which improves with non-steroidal anti-inflammatory medications [1].
For patients with chronic pain refractory to medical management, percutaneous ablation is the treatment of choice due to its high success rate and favorable side effect profile compared with surgical resection [1]. This procedure involves percutaneous placement of an ablation probe in the center of, or adjacent to, the nidus under imaging guidance (typically CT, cone beam CT, or in some cases MRI) and using either rapid heating or freezing and thawing to treat the lesion.
The first ablation technology used for the treatment of OOs was radiofrequency ablation (RFA), first described in the early 1990s [4,5,6]. This technology uses radiofrequency waves to induce coagulation necrosis of all tissue in a defined ablation zone surrounding the probe. Many retrospective and prospective trials have been performed since then, with a systematic review reporting successful resolution of symptoms in 95% of patients treated with RFA [7].
More recently, new ablation technologies have been used to treat OOs. Cryoablation, first described for the treatment of OOs in 2010, uses argon gas or carbon dioxide to induce cell death with cycles of rapid freezing and thawing with a temperature below – 40 °C [8]. This has the theoretical benefits of decreased pain during and after the procedure, which may limit the need for post-procedure pain medication. Additionally, the proceduralist has the ability to monitor the ablation zone by using CT during the procedure. Recent studies have also suggested that cryoablation, by causing the tissue necrosis without causing destruction of the intracellular contents, can promote an immune response to tumor cells outside the ablation zone, known as an abscopal effect [9]. Finally, there is evidence that nerves regenerate at a predictable rate when inadvertently or intentionally cryoablated, potentially rendering cryoablation a safer option for tumors in close proximity to nerves [10].
Microwave (MW) ablation, first described for OO treatment in 2014, uses microwaves to thermally ablate tumors [11, 12]. Microwave ablation can propagate further through tissues and is less affected by the type of tissue or tissue impedance than RFA [13].
Two subtypes of OOs warrant separate attention due to their challenging anatomical locations: 1) intra-articular OOs and 2) spinal OOs. Intra-articular lesions occur in approximately 13% of patients and present particular therapeutic challenges [14, 15]. Surgical excision is especially morbid, sometimes requiring prophylactic internal fixation of the bone [14]. Additionally, there are theoretical complications associated with the ablation of intra-articular lesions such as joint damage and injury to cartilage. Nevertheless, studies have shown high success rates in treatment of intra-articular lesions with RFA [14, 16].
Spinal OOs occur in approximately 10% of patients with OO [2, 3]. Ablation of spinal osteoid osteomas presents additional risk for nerve injury, especially in cases located close to nerve roots or the thecal sac. Surgical excision also presents increased risks, and some studies have shown high success and low complication rates with RFA of spinal osteoid osteomas [17,18,19].
Although RFA has a well-validated modality for the treatment of OO, the efficacy of other ablative technologies, such as cryoablation and MW ablation, has been less thoroughly studied. Because of the previously mentioned potential advantages of cryoablation and MW ablation (as compared with RFA), comparison of different ablative modalities is warranted. As the literature studying MW ablation of OO is currently very limited, a scientifically valid comparison can only be pursued between RFA and cryoablation. Additionally, the efficacy of percutaneous ablation for OOs in intra-articular and spinal locations has similarly only been evaluated with small, retrospective case series. Thus, the primary purpose of this manuscript is to perform a systematic review of the literature comparing the efficacy and safety of RFA and cryoablation in the treatment of OO. A secondary purpose of this systematic review is to analyze the efficacy of percutaneous ablation of OOs in intra-articular and spinal locations.
An associated abstract entitled Percutaneous thermal ablation for treatment of osteoid osteoma: a systematic review and analysis was presented at the 2019 annual meeting for the Cardiovascular and Interventional Radiological Society of Europe [20].
Materials and methods
This retrospective study was determined to be exempted by the Institutional Review Board and was performed in compliance with the Health Insurance Portability and Accountability Act. A search for published manuscripts was performed using PubMed, the Cochrane Library, Embase, and ClinicalTrials. The keywords “osteoid osteoma,” “ablation,” “thermocoagulation,” “radiofrequency,” “cryoablation,” and “microwave” were used in different combinations. Additionally, references from identified manuscripts were screened for further studies. A total of 79 studies were initially identified.
Studies were included if they met the following criteria: (1) retrospective or prospective analysis of RFA, cryoablation, or MW ablation of osteoid osteomas; (2) at least 6 months of clinical follow-up after treatment; (3) included at least 10 patients, including initial treatment as well as patients previously treated with ablation or surgery; (4) no patients also evaluated in a second study included in this review; and (5) English language or English translation available. Additionally, studies were excluded if they performed some other type of treatment, such as alcohol or laser ablation, in combination with RFA, cryoablations, or MW ablation.
Studies in which some but not all patients were followed for 6 months were included only if the outcomes were reported separately for those patients. Only the patients that were followed clinically for 6 months were included in the analysis. The search was performed using a predetermined search strategy, and the data extraction was based on a predefined data form. The Quality Appraisal Checklist for Case Series Studies was applied to each included study to assess its quality [21, 22].
Success was defined as a resolution to the patient’s pain without recurrence through the entire follow-up period. “Success rate” refers to the percentage of cases without technical failures (i.e., the ablation probe could not be successfully placed in or near the OO nidus or the procedure could not be completed), clinical failures (i.e., patients in whom the pain never resolved following treatment), or recurrences (i.e., patients in whom pain resolved for a period of time but then recurred). Patients who had a failure or recurrence but received a second successful treatment were counted twice, once as a failure/recurrence and once as a success (if adequate clinical follow-up was documented).
Data analysis
To compare different technologies (RFA vs cryoablation), logistic regression models were fitted for each outcome of interest (success, technical failures, clinical failures, recurrences, and complications) on the pooled data. Probabilities with 95% confidence intervals for overall sample and each technology groups were determined. Due to the small sample size, the MW ablation group (n = 1) was not included in this analysis. The group-specific probability of technical failures was not estimable because the number of observed events was too small. Multinomial regression analysis were also conducted to take into account that all outcomes sum up to the total sample size. All analyses were performed with SAS v9.4 (SAS Institute, Cary, NC).
Results
A total of 79 studies were identified, and 36 studies met the inclusion criteria, published between 2003 and 2018 (Table 1). A total of 1863 ablations in 1798 patients were included in this review. Of the included studies, 32 (88.9%) evaluated RFA, 3 (8.3%) evaluated cryoablation, and 1 (2.8%) evaluated MW ablation. Three studies (8.3%) included only adult patients, 4 (11.1%) included only children, and 29 (80.6%) included both. The mean age at time of procedure was 18.7 years (range 2 to 68 years). The mean ages for RFA, cryoablation, and MW ablation were 18.7, 17.5, and 28 years respectively. In 13 (36%) studies, biopsy was performed on all lesions. In 23 (64%) studies, biopsy was not performed on some or all lesions prior to ablation.
Successes, failures, and recurrences for each study are detailed in Table 2. Results of the pooled analysis are reported in Table 3. Overall success rate was 91.9% (95% confidence interval 91–93%). Success rates were 91.9%, 91.6%, and 100% for RFA, cryoablation, and MW respectively, without significant difference when comparing cryoablation and RFA (p = 0.92). Technical failure, clinical failure, and recurrence rates were 0.3%, 2.1%, and 5.6% respectively.
Technical failures, occurring in 0.3% (95% confidence interval 0.2%–0.7%), included shortened ablation time due to concern for developing hyperthermia in one case and concern about close proximity to the neurovascular bundle in another, failure to localize the lesion due to heavy sclerosis in one patient, inability to penetrate the sclerotic rim in one patient, and damage to the machine cable in one case.
Complications were seen in 2.5% (95% confidence interval 1.9–3.3%) of procedures. Major complications reported in studies evaluating RFA included one bone infarction requiring surgery, one soft-tissue infection severe enough to require surgical debridement, one skin burn requiring skin graft, one case of flash pulmonary edema resulting in 15 days of intubation, and one patient who developed complex regional pain syndrome 2 years following treatment. The access needle broke in three cases, one of which required surgical removal. Transient self-resolving paresthesias, the longest-lasting 30 days, were seen in three patients. Two patients developed contractures (finger and ankle) successfully treated with physical therapy. The remainder of complications were minor skin burns, skin and soft-tissue infections treated with antibiotics, a self-resolving hematoma, and a case of superficial thrombophlebitis. Studies evaluating cryoablation reported two patients with overnight admissions for pain, two cases of transient soft-tissue swelling, and one minor skin burn. No complications were reported in the study evaluating MW ablation.
In 13 (36.1%) studies, some or all patients were treated for intra-articular lesions (Table 4). A total of 157 ablations were performed on intra-articular lesions. For many treated lesions, based on the data provided, the success rate could not be determined; however, for the seven studies in which these patients could be analyzed separately based on the previously stated inclusion criteria, the success rate was 97.0%.
In 12 studies (33.3%), some or all patients were treated for spinal OOs (Table 5). A total of 142 ablations were performed on spinal lesions. As with intra-articular lesions, for many spinal lesions, the success rate could not be determined; however, for the nine studies in which these patients could be analyzed separately, the overall success rate was 91.6%.
Discussion
With an overall success rate of 91.9% and an overall complication rate of 2.5%, the results of this review reinforce the findings of previous studies that percutaneous thermal ablation of OOs is a safe and effective therapeutic alternative to open surgery [3, 7, 45]. RF and cryoablation demonstrated statistically similar outcomes. This finding is particularly salient, given some additional benefits of cryoablation over heat-based technologies. For example, a study evaluating patient response to different technologies for ablation of bony metastases demonstrated significantly decreased pain, analgesic use, and hospital length of stay with cryoablation compared with RFA, findings which may be applicable to treatment of osteoid osteomas as well [52].
Moreover, emerging evidence suggests that cryoablation may have an abscopal, or immunotherapy benefit, in addition to eliminating the risk of permanent nerve damage [9, 10]. Additionally, further evidence demonstrates that both motor and sensory nerves regenerate following (intentional and unintentional) cryoablation, which may improve the safety of ablations near critical nerves and spinal cord [10]. While additional studies are necessary to prove the merit of these scientifically based claims, the findings of this review confirm at least equal efficacy between the two (RF and cryoablation) modalities for the treatment of OOs. MW ablation, alternatively, while demonstrating promising results, lacks available literature for statistical comparison of efficacy.
The majority of failures were due to recurrent disease (5.6% for all modalities). Clinical failures (i.e., patients who never experienced pain relief following treatment) only occurred following 2.5% of procedures, and there was nearly a 100% technical success rate with all modalities. A total of 74 of the 104 patients (71.2%) with disease recurrence were successfully treated with a second ablation. While most recurrences occurred in the first few months following initial ablation, some occurred years after the initial treatment (median = 7 months, mean = 10.8 months, range = 1 month to 6 years). This highlights the importance of long-term clinical follow-up in this patient population.
Regarding anatomical location of OOs, because of the more challenging location and theoretical complications associated with the treatment of intra-articular lesions (e.g., joint damage and injury to cartilage), special attention was given to ablation of OOs in this location. Because the numbers of intra-articular lesions in studies were often very small, a direct comparison is difficult to make. Nevertheless, in the studies evaluating only intra-articular lesions, success and complication rates were similar to that of all lesions, with no joint-specific complications reported over at least a 6-month clinical follow-up interval [14, 16]. This study is limited, however, because it cannot determine the risk of chondrolysis and subsequent osteoarthritis which would likely take years to develop.
Similar to intra-articular OOs, spinal lesions were analyzed because of the proximity to critical structures such as nerve roots and the spinal cord. Nevertheless, no permanent neurologic complications were reported in the included studies, with only one case of a spontaneously resolving lower limb paresthesia that lasted for 30 days [17]. The success rates were also comparable to that of all lesions.
In 23 (64%) studies, the proceduralist did not biopsy some or all lesions prior to ablation. Because of the high specificity of cross-sectional imaging in the diagnosis of OO and negative or inconclusive biopsy results in many cases, some providers viewed this as an unnecessary step [1, 2]. In the studies included in this review, 766 biopsies were performed with only 59.3% diagnostic for osteoid osteoma. While detailed analysis of the non-diagnostic results is limited by heterogenous methodology and lack of detailed breakdown in most of the included studies, the vast majority were either reported to be non-diagnostic, normal bone tissue, or merely suggestive of OO. Nevertheless, Becce, et al. reported 10 OO mimic lesions out of 65 biopsied (5 chronic osteomyelitis, 3 chondroblastoma, 1 eosinophilic granuloma, 1 fibrous dysplasia) [29]. Consequently, although biopsy may not have a key role in the diagnosis of OO, the authors recommend its use in order to rule out other pathology, especially because it can be performed during the same procedure immediately prior to ablation without a delay in care or additional procedure. This is particularly important as the ablation changes the imaging appearance of the lesion and may confound subsequent evaluation.
There are some limitations to this review. Because they are relatively new techniques for treatment of osteoid osteoma, fewer papers evaluating the use of cryoablation and MW ablation were available. This limited the comparison between modalities. Additionally, MRI-guided high-intensity focused ultrasound (MgHIFU) has been shown to be effective for treatment for certain OOs with recurrence rates reported at 87% in the largest study [53]. Nevertheless, the indications for percutaneous ablation and MgHIFU are not entirely overlapping, given the exclusion of spinal lesions in the largest study and a separate technical feasibility study reporting that only 50% of OOs are amenable to treatment with MgHIFU alone [53, 54]. Moreover, only one identified study met the inclusion criteria of ten or more patients [53]. Thus, MgHIFU was not analyzed in this study.
Furthermore, only manuscripts with 10 patients or more were included. This small number decreases the power of the statistical analysis. Importantly, this cohort size requirement, albeit small, likely excluded some studies of cryoablation and MW ablation due to their recent emergence for use in treatment of OO. For similar reasons, studies with at least 6 months of follow-up were included, but many recurrences occur much later than that time period. Consequently, recurrent disease is likely underestimated in this review. Finally, patient population, lesion location, procedural practices, and definitions of complications and clinical failures differed across the included studies.
In conclusion, percutaneous ablation of osteoid osteomas was successful in 91.9% of patients with a very low (approximately 2.5%) complication rate. Success and complication rates between RFA and cryoablation were similar, which suggests that cryoablation may be preferential in most circumstances given its additional benefits, namely decreased post-procedure pain, predictable nerve regeneration, and theoretical immunotherapy effects. MW ablation, while demonstrating promising early results, still requires more published data for comparative efficacy. Finally, treatment of more challenging intra-articular and spinal lesions demonstrated success and complication rates similar to OO treated in more traditional anatomic locations.
References
Noordin S, Allana S, Hilal K, Nadeem N, Lakdawala R, Sadruddin A, et al. Osteoid osteoma: contemporary management. Orthop Rev (Pavia). 2018;10(3):7496.
Ghanem I. The management of osteoid osteoma: updates and controversies. Curr Opin Pediatr. 2006;18:36–41.
Rimondi E, Mavrogenis AF, Rossi G, Ciminari R, Malaguti C, Tranfaglia C, et al. Radiofrequency ablation for non-spinal osteoid osteomas in 557 patients. Eur Radiol. 2012;22(1):181–8.
Lindner NJ, Scarborough M, Ciccarelli JM, Enneking WF. CT-controlled thermocoagulation of osteoid osteoma in comparison with traditional methods. Z Orthop Ihre Grenzgeb. 1997;135(6):522–7 German.
Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, Mankin HJ. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am. 1998;80(6):815–21.
Simon MA. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am. 1999;81(3):437–8.
Lanza E, Thouvenin Y, Viala P, Sconfienza LM, Poretti D, Cornalba G, et al. Osteoid osteoma treated by percutaneous thermal ablation: when do we fail? A systematic review and guidelines for future reporting. Cardiovasc Intervent Radiol. 2014;37(6):1530–9.
Liu DM, Kee ST, Loh CT, McWilliams J, Ho SG, Brower JS, et al. Cryoablation of osteoid osteoma: two case reports. J Vasc Interv Radiol. 2010;21(4):586–9.
Aarts BM, Klompenhouwer EG, Rice SL, Imani F, Baetens T, Bex A, et al. Cryoablation and immunotherapy: an overview of evidence on its synergy. Insights Imaging. 2019;10:53.
Johnson C, Mitchell J, Manyapu S, Hawkins C, Singer A, Prologo J. Natural history of motor nerve cryoablation: a retrospective cohort analysis. J Vasc Interv Radiol. 2019;30(3):S176.
Kostrzewa M, Diezler P, Michaely H, Rathmann N, Attenberger UI, Schoenberg SO, et al. Microwave ablation of osteoid osteomas using dynamic MR imaging for early treatment assessment: preliminary experience. J Vasc Interv Radiol. 2014;25(1):106–11.
Basile A, Failla G, Reforgiato A, Scavone G, Mundo E, Messina M, et al. The use of microwaves ablation in the treatment of epiphyseal osteoid osteomas. Cardiovasc Intervent Radiol. 2014;37(3):737–42.
Hinshaw JL, Lubner MG, Ziemlewicz TJ, Lee FT, Brace CL. Percutaneous tumor ablation tools: microwave, radiofrequency, or cryoablation—what should you use and why? RadioGraphics. 2014;35:1344–62.
Papagelopoulos PJ, Mavrogenis AF, Kyriakopoulos CK, Benetos IS, Kelekis NL, Andreou J, et al. Radiofrequency ablation of intra-articular osteoid osteoma of the hip. J Int Med Res. 2006;34(5):537–44.
Allen SD, Saiffuddin A. Imaging of intra-articular osteoid osteoma. Clin Radiol. 2003;58:845–52.
Albisinni U, Bazzocchi A, Bettelli G, Facchini G, Castiello E, Cavaciocchi M, et al. Treatment of osteoid osteoma of the elbow by radiofrequency thermal ablation. J Shoulder Elb Surg. 2014;23(1):e1–7.
Albisinni U, Facchini G, Spinnato P, Gasbarrini A, Bazzocchi A. Spinal osteoid osteoma: efficacy and safety of radiofrequency ablation. Skelet Radiol. 2017;46(8):1087–94.
Martel J, Bueno A, Nieto-Morales ML, Ortiz EJ. Osteoid osteoma of the spine: CT-guided monopolar radiofrequency ablation. Eur J Radiol. 2009;71(3):564–9.
Morassi LG, Kokkinis K, Evangelopoulos DS, Karargyris O, Vlachou I, Kalokairinou K, et al. Percutaneous radiofrequency ablation of spinal osteoid osteoma under CT guidance. Br J Radiol. 2014;87(1038):20140003.
Lindquester WS, Crowley JJ, Hawkins CM. Percutaneous thermal ablation for treatment of osteoid osteoma: a systematic review and analysis. Poster session presented at: Cardiovascular and Interventional Radiological Society of Europe Annual Meeting; 7–11 Sept. 2019.
Institute of Health Economics (IHE). Quality appraisal of case series studies checklist. Edmonton (AB): Institute of Health Economics; 2014. Available from: http://ihe.ca/research-programs/rmd/cssqac-about
Moga C, Guo B, Schopflocher D, Harstall C. Development of a quality appraisal tool for case series studies using a modified Delphi technique. Institute of Health Economics: Edmonton; 2012.
Coupal TM, Mallinson PI, Munk PL, Liu D, Clarkson P, Ouellette H. CT-guided percutaneous cryoablation for osteoid osteoma: initial experience in adults. AJR Am J Roentgenol. 2014;202(5):1136–9.
Santiago E, Pauly V, Brun G, Guenoun D, Champsaur P, Le Corroller T. Percutaneous cryoablation for the treatment of osteoid osteoma in the adult population. Eur Radiol. 2018;28(6):2336–44.
Shah J, Gill A, Laporte J, Whitmore M, Bertino F, Prologo JD, et al. Long-term results and durability of cryoablation of osteoid osteoma in the pediatric and adolescent population. Pediatr Radiol. 2019;49(Suppl 1):S75.
Abboud S, Kosmas C, Novak R, Robbin M. Long-term clinical outcomes of dual-cycle radiofrequency ablation technique for treatment of osteoid osteoma. Skelet Radiol. 2016;45(5):599–606.
Akhlaghpoor S, Aziz Ahari A, Arjmand Shabestari A, Alinaghizadeh MR. Radiofrequency ablation of osteoid osteoma in atypical locations: a case series. Clin Orthop Relat Res. 2010;468(7):1963–70.
Al-Omari MH, Ata KJ, Al-Muqbel KM, Mohaidat ZM, Haddad WH, Rousan LA. Radiofrequency ablation of osteoid osteoma using tissue impedance as a parameter of osteonecrosis. J Med Imaging Radiat Oncol. 2012;56(4):384–9.
Becce F, Theumann N, Rochette A, Larousserie F, Campagna R, Cherix S, et al. Osteoid osteoma and osteoid osteoma-mimicking lesions: biopsy findings, distinctive MDCT features and treatment by radiofrequency ablation. Eur Radiol. 2010;20(10):2439–46.
Bourgault C, Vervoort T, Szymanski C, Chastanet P, Maynou C. Percutaneous CT-guided radiofrequency thermocoagulation in the treatment of osteoid osteoma: a 87 patient series. Orthop Traumatol Surg Res. 2014;100(3):323–7.
Cantwell CP, O'Byrne J, Eustace S. Radiofrequency ablation of osteoid osteoma with cooled probes and impedance-control energy delivery. AJR Am J Roentgenol. 2006;186(5 Suppl):S244–8.
Cheng EY, Naranje SM, Ritenour ER. Radiation dosimetry of intraoperative cone-beam compared with conventional CT for radiofrequency ablation of osteoid osteoma. J Bone Joint Surg Am. 2014;96(9):735–42.
Cioni R, Armillotta N, Bargellini I, Zampa V, Cappelli C, Vagli P, et al. CT-guided radiofrequency ablation of osteoid osteoma: long-term results. Eur Radiol. 2004;14(7):1203–8.
Daniilidis K, Martinelli N, Gosheger G, Hoell S, Henrichs M, Vogt B, et al. Percutaneous CT-guided radio-frequency ablation of osteoid osteoma of the foot and ankle. Arch Orthop Trauma Surg. 2012;132(12):1707–10.
Donkol RH, Al-Nammi A, Moghazi K. Efficacy of percutaneous radiofrequency ablation of osteoid osteoma in children. Pediatr Radiol. 2008;38(2):180–5.
Garge S, Keshava SN, Moses V, Chiramel GK, Ahmed M, Mammen S, et al. Radiofrequency ablation of osteoid osteoma in common and technically challenging locations in pediatric population. Indian J Radiol Imaging. 2017;27(1):88–91.
Ghanem I, Collet L-M, Kharrat K, Samaha E, Deramon H, Mertl P, et al. Percutaneous radiofrequency coagulation of osteoid osteoma in children and adolescents. J Pediatr Orthop B. 2003;12(4):244–52.
Hage AN, Chick JFB, Gemmete JJ, Grove JJ, Srinivasa RN. Percutaneous radiofrequency ablation for the treatment of osteoid osteoma in children and adults: a comparative analysis in 92 patients. Cardiovasc Intervent Radiol. 2018;41(9):1384–90.
Hoffmann RT, Jakobs TF, Kubisch CH, Trumm CG, Weber C, Duerr H-R, et al. Radiofrequency ablation in the treatment of osteoid osteoma-5-year experience. Eur J Radiol. 2010;73(2):374–9.
Karagöz E, Özel D, Özkan F, Özel BD, Özer Ö, Coşkun ZÜ. Effectiveness of computed tomography guided percutaneous radiofrequency ablation therapy for osteoid osteoma: initial results and review of the literature. Pol J Radiol. 2016;81:295–300.
Mylona S, Patsoura S, Galani P, Karapostolakis G, Pomoni A, Thanos L. Osteoid osteomas in common and in technically challenging locations treated with computed tomography-guided percutaneous radiofrequency ablation. Skelet Radiol. 2010;39(5):443–9.
Neumann D, Berka H, Dorn U, Neureiter D, Thaler C. Follow-up of thirty-three computed-tomography-guided percutaneous radiofrequency thermoablations of osteoid osteoma. Int Orthop. 2012;36(4):811–5.
Peyser A, Applbaum Y, Khoury A, Liebergall M, Atesok K. Osteoid osteoma: CT-guided radiofrequency ablation using a water-cooled probe. Ann Surg Oncol. 2007;14(2):591–6.
Peyser A, Applbaum Y, Simanovsky N, Safran O, Lamdan R. CT-guided radiofrequency ablation of pediatric osteoid osteoma utilizing a water-cooled tip. Ann Surg Oncol. 2009;16(10):2856–61.
Rosenthal DI, Hornicek FJ, Torriani M, Gebhardt MC, Mankin HJ. Osteoid osteoma: percutaneous treatment with radiofrequency energy. Radiology. 2003;229(1):171–5.
Ruiz Santiago F, Castellano García Mdel M, Guzmán Álvarez L, Martínez Montes JL, Ruiz García M, Tristán Fernández JM. Percutaneous treatment of bone tumors by radiofrequency thermal ablation. Eur J Radiol. 2011;77(1):156–63.
Schmidt D, Clasen S, Schaefer JF, Rempp H, Duda S, Trübenbach J, et al. CT-guided radiofrequency (RF) ablation of osteoid osteoma: clinical long-term results. Rofo. 2011;183(4):381–7.
Shields DW, Sohrabi S, Crane EO, Nicholas C, Mahendra A. Radiofrequency ablation for osteoid osteoma-recurrence rates and predictive factors. Surgeon. 2018;16(3):156–62.
Soong M, Jupiter J, Rosenthal D. Radiofrequency ablation of osteoid osteoma in the upper extremity. J Hand Surg [Am]. 2006;31(2):279–83.
Sung K-S, Seo J-G, Shim JS, Lee YS. Computed-tomography-guided percutaneous radiofrequency thermoablation for the treatment of osteoid osteoma-2 to 5 years follow-up. Int Orthop. 2009;33(1):215–8.
Vanderschueren GM, Obermann WR, Dijkstra SPD, Taminiau AHM, Bloem JL, van Erkel AR. Radiofrequency ablation of spinal osteoid osteoma: clinical outcome. Spine. 2009;34(9):901–4.
Thacker PG, Callstrom MR, Curry TB, Mandrekar JN, Atwell TD, Goetz MP, et al. Palliation of painful metastatic disease involving bone with imaging-guided treatment: comparison of patients’ immediate response to radiofrequency ablation and cryoablation. AJR Am J Roentgenol. 2011;197(2):510–5.
Napoli A, Bazzocchi A, Scipione R, Anzidei M, Saba L, Ghanouni P, et al. Noninvasive therapy for osteoid osteoma: a prospective developmental study with MR imaging-guided high-intensity focused ultrasound. Radiology. 2017;285(1):186–96. https://doi.org/10.1148/radiol.2017162680 Epub 2017 Jun 7.
Bing F, Vappou J, de Mathelin M, Gangi A. Targetability of osteoid osteomas and bone metastases by MR-guided high intensity focused ultrasound (MRgHIFU). Int J Hyperth. 2018;35(1):471–9.
Funding
Marnie Bertolet (assistant professor in the department of Epidemiology) and Liwen Wu (graduate student in the department of biostatistics) of the Graduate School of Public Health at the University of Pittsburgh aided in the statistical analysis through funding from the Clinical and Translational Science Institute at the University of Pittsburgh (National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, grant UL1 TR001857).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This retrospective study was determined to be exempted by the Institutional Review Board and was performed in compliance with the Health Insurance Portability and Accountability Act
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lindquester, W.S., Crowley, J. & Hawkins, C.M. Percutaneous thermal ablation for treatment of osteoid osteoma: a systematic review and analysis. Skeletal Radiol 49, 1403–1411 (2020). https://doi.org/10.1007/s00256-020-03435-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03435-7