Abstract
Objective
To correlate MRI findings of patients with posterior cruciate ligament (PCL) injury and surgical management.
Materials and methods
A retrospective search yielded 79 acute PCL injuries (36 ± 16 years old, 21 F, 58 M). Two independent readers graded PCL tear location (proximal, middle, or distal third) and severity (low-grade or high-grade partial/complete) and evaluated injury of other knee structures. When available, operative reports were examined and the performed surgical procedure was compared with injury grade, location, and presence of associated injuries.
Results
The most commonly injured knee structures in acute PCL tears were posterolateral corner (58/79, 73%) and anterior cruciate ligament (ACL) (48/79, 61%). Of the 64 patients with treatment information, 31/64 (48%) were managed surgically: 12/31 (39%) had PCL reconstruction, 13/31 (42%) had ACL reconstruction, 10/31 (32%) had posterolateral corner reconstruction, 9/31 (29%) had LCL reconstruction, 8/31 (26%) had meniscectomy, and 8/31 (26%) had fixation of a fracture. Proximal third PCL tear and multiligamentous injury were more commonly associated with surgical management (P < 0.05). Posterolateral and posteromedial corner, ACL, collateral ligament, meniscus, patellar retinaculum, and gastrocnemius muscle injury, and fracture were more likely to result in surgical management (P < 0.05). Patients with high-grade partial/complete PCL tear were more likely to have PCL reconstruction as a portion of surgical management (P < 0.05).
Conclusions
Location of PCL tear and presence of other knee injuries were associated with surgical management while high-grade/complete PCL tear grade was associated with PCL reconstruction. MRI reporting of PCL tear location, severity, and of other knee structure injuries is important for guiding clinical management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The posterior cruciate ligament (PCL) is the major mechanical restraint to posterior translation of the tibia relative to the femur [1]. PCL tear has been reported to occur in 79% of multiligamentous knee injuries, 38% of traumatic knee hemarthroses, 7.8% of patients with periarticular knee fractures, and to constitute 2.4% of all knee injuries in high school athletes in the United States [2,3,4]. The most common etiologies of acute PCL injury are motor vehicle accidents and athletic trauma, and PCL tears are seen more frequently in men [2, 5, 6]. MRI examination is effective in defining the extent of ligamentous, soft tissue, and osseous abnormalities in acute knee injuries [1, 7,8,9].
PCL injury can be treated with surgical PCL reconstruction or by non-operative conservative management [1, 2, 10,11,12,13,14,15,16]. Surgical literature supports operative management of acute PCL injuries with knee instability and multiligamentous injuries [1, 12]. Alternatively, chronic PCL injuries with acceptable function as well as isolated PCL tear without knee instability can be managed non-operatively [1, 11, 13, 15,16,17]. We have found no studies in the existing radiology literature which examine whether grade and location of PCL injuries determines surgical versus conservative management of acute PCL tears. Additionally, existing radiology literature contains five studies that have examined the frequency of associated knee structure injuries by MRI in the setting of acute PCL injury. The largest cohort has 54 patients, and there are no studies which examine the correlation between PCL tear, associated injuries, and surgical management [18,19,20,21,22].
The objective of this study was to correlate PCL MRI findings, including severity, location, and associated injuries, with surgical management to determine the injuries that guide clinical management.
Materials and methods
Subject selection
This study was approved by the Institutional Review Board (IRB) and complied with the Health Insurance Portability and Accountability Act (HIPAA) guidelines. Subject informed consent was not required because of the retrospective study design.
A retrospective search among knee MRI examinations was performed at our institution between 1995 and 2016 using the search terms “PCL tear”, “tear of the PCL”, “tear of PCL”, “PCL rupture”, “rupture of the PCL”, “rupture of PCL”, “PCL repair”, and “PCL reconstruction”, which yielded 322 results. Exclusion criteria were (1) inadequate, absent, or duplicate imaging (N = 151), (2) skeletal immaturity defined by the presence of open physes (N = 3), and (3) findings consistent with chronic rather than acute PCL injury defined by the absence of soft tissue edema, joint effusion, or osseous contusion based on review of MR images, and those with prior knee surgery (N = 89). Seventy-nine acute PCL injuries were included (Fig. 1).
Imaging studies
All knee MRIs were performed at 1.5 T or 3 T MRI with a dedicated surface coil (Siemens Medical Solutions USA, Inc., Malvern, PA, USA and GE Healthcare, Chicago, IL, USA). Although a variety of MRI scanners were used across the study period, all cases that were included were determined to have diagnostic-quality images on review of MR images. Imaging sequences and parameters were:
-
Coronal T1-weighted: TR 480–620 ms, TE 15–17 ms, flip angle 90, NEX 1, matrix size 448 × 384, FOV 16 cm, slice thickness/gap 4/10
-
Sagittal T2-weighted fat-saturated: TR 3700–4400 ms, TE 35–48 ms, flip angle 90, NEX 1–2, matrix size 320–288, FOV 15–16 cm, slice thickness/gap 3/10
-
Coronal T2-weighted fat-saturated: TR 3300–3800 ms, TE 45–52 ms, flip angle 90, NEX 1, matrix size 320–288, FOV 16 cm, slice thickness/gap 4/10
-
Sagittal proton density: TR 2000–2600 ms, TE 25–27 ms, flip angle 90, NEX 1, matrix size 320–320, FOV 15–16 cm, slice thickness/gap 3/10
-
Axial T2-weighted fat-saturated: TR 3600–4900 ms, TE 50–55 ms, flip angle 90, NEX 2, matrix size 320–256, FOV 15–16 cm, slice thickness/gap 3/10
Image review - evaluation of PCL and associated injuries
Each case was reviewed independently by two musculoskeletal radiologists with 6 and 5 years of experience (CYC and FJS) for injury of the following structures: PCL, ACL, medial and lateral menisci, extensor mechanism, posterolateral corner (lateral collateral ligament (LCL), popliteus muscle and tendon, biceps femoris muscle and tendon, popliteofibular ligament, and posterolateral joint capsule), posteromedial corner (semimembranosus muscle and tendon and posterior oblique ligament/posteromedial joint capsule), medial collateral ligament (MCL), medial and lateral gastrocnemius muscles, medial and lateral patellar retinacula, contusion or fracture, and acute cartilage defects. Although the LCL was included as a posterolateral corner structure for grading presence of injury, some patients had LCL repair without repair of other posterolateral corner structures and other patients had no LCL repair but repair of other posterolateral corner structures. Therefore, the LCL was considered separately during surgical correlation. The term multiligamentous is used to denote complex injuries to multiple ligaments including the PCL, ACL, MCL, and posterolateral corner including the LCL. In contradistinction, the term isolated ligamentous PCL injury is used to denote patients with PCL injury, without injury of the ACL, MCL, and posterolateral corner including the LCL, but possibly with other non-ligamentous injuries such as meniscal tear, cartilage injury, musculotendinous injury, or fracture.
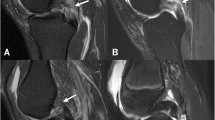
The PCL injuries were divided into two grades: grade 1, sprain or low-grade partial tear, and grade 2, high-grade partial tear or complete tear. Sprain/low-grade partial tear were defined as abnormal thickening (≥ 7 mm) without a fluid gap or attenuation and T2 hyperintense signal to normal ligament involving less than 50% of ligament fibers (Fig. 2) [23]. High-grade partial tear/complete tear were defined as discontinuity of and fluid signal gap between tendon fibers involving 50 to 100% of ligament fibers (Figs. 3 and 4) [23, 24]. The location of the PCL tear (proximal, middle, or distal third) was also recorded [19, 25].
Twenty-four-year-old man with pain and instability after injuring his knee playing basketball. Sagittal T2-weighted fat-saturated image shows high intra-substance signal with an AP diameter ≥ 7 mm of the vertical segment (bracket) excluding the anterior meniscofemoral ligament of Humphrey (arrow), without fluid signal gap, consistent with a distal third low-grade partial tear
Other than the PCL, each ligament, tendon, and muscle was graded as normal or injured. Each structure was defined as injured if it was thickened or attenuated and T2 hyperintense to normal ligament/tendon fibers but hypointense to fluid, partially discontinuous with a fluid signal intensity gap, or completely discontinuous with a fluid signal gap (Fig. 5).
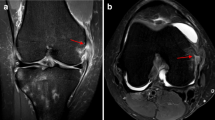
Cartilage and menisci were defined as injured if there was a fluid signal intensity gap in the normal structure (Fig. 6). Bone contusion was defined by increased T2 signal on fluid sensitive sequences with corresponding decreased T1 signal. Fracture was defined by cortical discontinuity or subchondral linear low T1 signal with surrounding increased T2 signal.
Twenty-four-year-old man with pain, instability, and deformity since injuring his knee playing basketball. Axial T2-weighted fat-saturated image (a) and coronal T2-weighted fat-saturated image (b) show complex tear of the lateral meniscus posterior horn with avulsion of the tibial root attachment (arrows)
For statistical analysis, discrepant reads were reconciled by using the more senior radiologist’s interpretation (Reader 1).
Surgical correlation
The electronic medical record for each patient was reviewed for management of PCL injury. If management was surgical, intraoperative findings from the operative report and type of surgical procedure were recorded, including ligament reconstruction, tendon/ligament repair, meniscectomy, chondroplasty, peroneal neurolysis or decompression, popliteal artery repair, fracture fixation, and total knee arthroplasty.
Statistical analysis
All statistics were performed using JMP®, Version 13.0.1 Pro (SAS Institute Inc., Cary, NC, USA). A P value < 0.05 was used as the critical alpha level for statistical significance for all Chi-square, Fisher’s exact, and t tests. All t tests were two-sided. Statistical comparisons included:
-
PCL:
-
Among patients with PCL plus other ligament injury, comparison was made for surgical versus conservative management and for PCL reconstruction versus surgical management other than PCL reconstruction.
-
Comparison was made between PCL only versus multiligamentous injury for surgical versus conservative management and for PCL reconstruction versus surgical management other than PCL reconstruction.
-
Comparison was made between sprain/low-grade PCL tear versus high-grade/complete PCL tear for surgical management versus conservative management and for PCL reconstruction versus surgical management other than PCL reconstruction.
-
Comparison was made between proximal, middle, and distal third PCL tear location for surgical management versus conservative management and for PCL reconstruction versus surgical management other than PCL reconstruction.
-
A likelihood-ratio Chi-square test was used to determine if there was a significant difference between PCL tear grade for proximal, middle, and distal tear locations and between surgical versus conservative management for: PCL tear alone versus PCL tear plus each other ligament injury, isolated ligamentous PCL tear versus multiligamentous injury, low-grade partial PCL tear versus high-grade partial/complete PCL tear, and between location PCL tear. After Chi-square tests for location of PCL tear and tear grade and well as surgical versus conservative management, post-hoc analyses using probabilities of adjusted standardized residuals for each contingency table cell and using Bonferroni correction were calculated to identify the individual tear location comparisons which contributed to statistical significance [26].
Fisher’s exact test was used to determine if there was a significant difference between isolated ligamentous PCL tear versus multiligamentous injuries and between low-grade partial and high-grade partial/complete PCL tears who had PCL reconstruction versus surgical management other than PCL reconstruction [27].
-
Demographics:
An unpaired two-sample t test was used to determine if there was a significant difference between mean age of patients managed surgically versus conservatively and between patients who had PCL reconstruction versus surgical management other than PCL reconstruction.
A likelihood Chi-square test was used to determine if there was a significant difference between gender of patients managed surgically versus conservatively and between patients who had PCL reconstruction versus surgical management other than PCL reconstruction.
-
Inter-rater agreement:
Inter-rater agreement on the presence of injury to each structure and on the mechanisms of injury was assessed by calculating a Kappa agreement coefficient (κ) for each structure. κ value of 0–0.2 indicated slight agreement, 0.21–0.40 indicated fair agreement, 0.41–0.60 indicated moderate agreement, 0.61–0.80 indicated substantial agreement, and 0.81–1.0 indicated almost perfect agreement [28].
Results
Subject clinical information
There were 58/79 (73%) males and 21/79 (27%) females. The average age at injury was 36 ± 16 (range, 15–74) years.
PCL and associated injuries
High-grade partial/complete tears (62/79, 78%) were more common than low-grade partial PCL tear (17/79, 22%). There were no PCL avulsion injuries. PCL tears were located at the proximal third in 32/79 (40%), middle third in 29/79 (37%), and distal third in 18/79 (23%) of patients. There was no statistical relationship between PCL tear location and grade. There were 10/79 (13%) isolated ligamentous PCL injuries and 69/79 (87%) multiligamentous injuries (Table 1).
The associated injuries are detailed in Table 2. The most commonly injured soft tissue structures were the posterolateral corner (58/79, 73%) and ACL (48/79, 61%). All patients with an LCL injury (37/79, 47%) had injury to an additional posterolateral corner structure. Most patients (69/79, 87%) had multiple knee ligament injuries. The medial meniscus (27/79, 34%) was more commonly injured than the lateral meniscus (8/79, 10%).
Osseous contusions were seen in 64/79 (81%) of patients while fractures were seen in 52/79 (66%). Proximal tibial contusions (33/79, 42%) were more common than distal femoral contusions (29/79, 37%). Patellar contusions were rare (2/79, 3%). Proximal tibial fractures (26/79, 33%) were more common than distal femoral fractures (22/79, 28%). Proximal fibular fractures were less common (4/79, 5%). Acute knee cartilage defects occurred in 9%; three at the femoral condyles and two each at the patella and tibial plateau.
Surgical correlation
Sixty-four (64/79, 81%) patients had medical records containing information about treatment following injury (Fig. 7). Thirty-one 31/64 (48%) were managed surgically while 33/64 (52%) were managed conservatively. There were 14 different orthopedic surgeons, specializing in sports medicine (N = 9), trauma (N = 3), and arthroplasty (N = 2).
There were ten patients with isolated ligamentous PCL injury and medical records with treatment information, two of which (2/10, 20%) were managed surgically. These two patients underwent chondroplasty and total knee arthroplasty respectively, without PCL reconstruction. Two patients had isolated PCL reconstruction as their only surgical management, both of whom had multiligamentous injuries; one with ACL and posterolateral corner injury and the other with ACL, posterolateral corner, posteromedial corner, as well as medial and lateral gastrocnemius muscle injuries. There were 54 patients with multiligamentous injury, defined as injury of the PCL and at least one of: ACL, MCL, or posterolateral corner, and with medical records containing treatment information. Twenty-nine (29/54, 54%) multiligamentous injuries were managed surgically. Multiligamentous injuries were more likely than isolated ligamentous PCL injuries to be managed surgically (P value = 0.04), but were no more likely to have PCL reconstruction versus other surgical management (P value = 0.51).
Of the 31 patients managed surgically, 12/31 (39%) patients had PCL reconstruction, while 19/31 (61%) patients had other structures repaired/reconstructed without PCL reconstruction. Other structures which were surgically repaired/reconstructed included 13/31 (42%) ACL, 10/31 (32%) posterolateral corner (posterolateral joint capsule, popliteus muscle/tendon, biceps femoris muscle/tendon, and popliteofibular ligament), and 9/31 (29%) LCL. Of the patients who had surgical repair/reconstruction of the LCL, two had this as the sole surgical management while seven had other posterolateral corner structures repaired as well. In addition, 9/31 (29%) patients had partial or complete meniscectomy, and 8/31 (26%) patients had fixation of a fracture. Less common operations included peroneal nerve decompression/neurolysis in 6/31 (19%), chondroplasty in 3/31 (10%), MCL repair in 2/31 (6%), popliteal artery repair in 2/31 (6%), and total knee arthroplasty in 2/31 (6%).
A comparison of patients managed by surgery versus conservative measures is provided in Table 3. Patients with injury of the PCL and presence of concomitant injury of the ACL, MCL, posterolateral corner structures, and meniscus were more likely to be managed surgically (P values = 0.00001–0.02). Patient demographic information and associated knee soft tissue injuries of patients who went to surgery and had PCL reconstruction versus other surgery are listed in Table 4. There were no specific concomitant injuries that resulted in PCL reconstruction more often than other surgical management, among those PCL tears managed surgically.
Patients with high-grade partial or complete PCL tear trended toward but were not statistically significantly more likely to be managed surgically rather than conservatively, compared to patients with sprain/low-grade partial PCL tear (P = 0.06). However, among surgically managed patients, high-grade partial or complete PCL tears were more likely to undergo PCL reconstruction as a portion of surgical management than patients with low-grade partial PCL tear (P = 0.001).
There was an overall significant relationship between PCL tear location and surgical versus conservative management (P value = 0.01), with post hoc analyses showing proximal third tears being more likely managed surgically (P = 0.001) and middle third tears being more likely managed conservatively (P = 0.006).
Statistical analysis
Tables 3 and 4 show the statistical comparisons for age, gender, and presence of other knee structure injuries related to surgical management and PCL reconstruction.
Interobserver agreement κ for injury to associated structures in the setting of PCL injury ranged from 0.85 to 1.0 (average 0.96), showing almost perfect agreement for all structures.
Discussion
We found that proximal third PCL tears and those with concomitant knee injuries, particularly posterolateral corner and ACL, were more likely to be managed surgically. Accurate reporting of PCL tear grade and location and associated injuries is important to guide clinical management.
Males have been reported to make up between 60 and 73% of isolated and combined PCL injuries in large demographic studies of up to 1200 patients [2, 5, 6], consistent with our results, which found that men made up 73% of acute PCL injuries. The majority of PCL injuries have been reported to occur in 30 to 50-year-old patients with an average age at time on PCL injury of 33 years [5, 6], consistent with our population, which had an average age at injury of 36 years.
Existing reports in the radiology and orthopedic literature have reported similar frequency of patient demographics and concomitant injuries in patients with acute PCL tear [1,2,3, 5, 6, 18,19,20, 29]. We found a higher overall rate of injury of other knee structures, although this may be due to our binary grading of each structure as normal or injured and thus the grouping of low-grade injuries with high-grade injuries (Table 2).
Management of PCL injuries can be surgical by PCL reconstruction or non-operative with physical therapy and activity modification, depending on whether the injury is acute or chronic, on associated knee structure injuries, and on the functional goals of the patient [1, 2, 10,11,12,13,14,15,16]. Orthopedic literature supports operative management for patients with acute PCL tear and knee instability or multiligamentous injury [1, 12]. Isolated PCL tear may be managed non-operatively in the absence of knee instability [1, 11, 13, 16, 17]. Acute avulsion fracture of the PCL is treated with open reduction and internal fixation [15]. One study of 25 patients and average follow-up of more than 6 years reported that 80% of patients with isolated PCL tear were satisfied with knee function and able to return to sport after nonoperative management [32]. Another study of 43 patients with an average follow-up of more than 6 years reported successful nonoperative management of isolated PCL tears but significantly higher incidence of fair or poor functional outcomes and osteoarthritic progression for PCL tears with associated ligament injuries managed nonoperatively [33]. Management of the 64 patients (81%) who had information in the medical record on treatment was consistent with the recommendations of existing orthopedic literature, with an approximately equal number of patients being managed surgically (48%) and conservatively (52%).
No patients with isolated ligamentous PCL injury underwent PCL reconstruction. Patients with injury of the PCL and presence of concomitant injury of the ACL, MCL, posterolateral corner, and meniscus were more likely to be managed surgically. However, the PCL was not repaired in the majority of surgically managed cases (61%). Patients with proximal third PCL tears were more likely to be managed surgically rather than conservatively. Among surgically managed patients, high-grade partial/complete PCL tears were more likely to undergo PCL reconstruction as a portion of surgical management than patients with low-grade partial PCL tear. These findings highlight the importance of reporting PCL tear grade and location and coexisting knee structure injuries in the setting of PCL tear in guiding management.
Limitations of this retrospective study include that patient positioning, length of time from injury to imaging, and detailed history from each patient could not be controlled, and information about these features was limited. Additionally, since surgical correlation was limited to those patients (N = 64) for whom operative details were available in our institution’s electronic medical record, management information about patients who got care at outside facilities was not included. This may have included patients who were managed surgically. The number of surgeons (14) and varying subspecialties (sports medicine, trauma, and arthroplasty) who operated on our patient population may mean there was variation in decision algorithm, choice of treatment, and operations performed.
In conclusion, proximal third PCL tears and PCL tears with injury of multiple knee soft tissue structures are more likely to be managed surgically rather than conservatively. High-grade partial/complete PCL tears are more likely than low-grade partial PCL tears to undergo PCL reconstruction as a portion of surgical management. Accurate reporting of PCL tear location, grade, and associated injuries on knee MRI is important for guiding clinical management.
References
LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med. 2015;43:3077–92.
Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: part II. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 1995;11:526–9.
Becker EH, Watson JD, Dreese JC. Investigation of multiligamentous knee injury patterns with associated injuries presenting at a level I trauma center. J Orthop Trauma. 2013;27:226–31.
Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45:462–9.
Chen G, Fu W, Tang X, Li Q, Li J. Clinical epidemiological analysis on posterior cruciate ligament injuries. Zhongguo Gu Shang China J Orthop Traumatol. 2015;28:638–42.
Owesen C, Sandven-Thrane S, Lind M, Forssblad M, Granan L-P, Årøen A. Epidemiology of surgically treated posterior cruciate ligament injuries in Scandinavia. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2015.
MacMahon PJ, Palmer WE. A biomechanical approach to MRI of acute knee injuries. AJR Am J Roentgenol. 2011;197:568–77.
Hayes CW, Brigido MK, Jamadar DA, Propeck T. Mechanism-based pattern approach to classification of complex injuries of the knee depicted at MR imaging. Radiogr Rev Publ Radiol Soc N Am Inc. 2000;20 Spec No:S121–134.
Sanders TG, Medynski MA, Feller JF, Lawhorn KW. Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiogr Rev Publ Radiol Soc N Am Inc. 2000;20 Spec No:S135–151.
Fanelli GC, Giannotti BF, Edson CJ. The posterior cruciate ligament arthroscopic evaluation and treatment. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 1994;10:673–88.
Clancy WG, Shelbourne KD, Zoellner GB, Keene JS, Reider B, Rosenberg TD. Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament. Report of a new procedure. J Bone Joint Surg Am. 1983;65:310–22.
Cosgarea AJ, Jay PR. Posterior cruciate ligament injuries: evaluation and management. J Am Acad Orthop Surg. 2001;9:297–307.
Dandy DJ, Pusey RJ. The long-term results of unrepaired tears of the posterior cruciate ligament. J Bone Joint Surg (Br). 1982;64:92–4.
LaPrade RF, Wentorf FA, Fritts H, Gundry C, Hightower CD. A prospective magnetic resonance imaging study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2007;23:1341–7.
Montgomery SR, Johnson JS, McAllister DR, Petrigliano FA. Surgical management of PCL injuries: indications, techniques, and outcomes. Curr Rev Musculoskelet Med. 2013;6:115–23.
Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1999;27:276–83.
Jacobi M, Reischl N, Wahl P, Gautier E, Jakob RP. Acute isolated injury of the posterior cruciate ligament treated by a dynamic anterior drawer brace: a preliminary report. J Bone Joint Surg (Br). 2010;92:1381–4.
Grover JS, Bassett LW, Gross ML, Seeger LL, Finerman GA. Posterior cruciate ligament: MR imaging. Radiology. 1990;174:527–30.
Sonin AH, Fitzgerald SW, Hoff FL, Friedman H, Bresler ME. MR imaging of the posterior cruciate ligament: normal, abnormal, and associated injury patterns. Radiogr Rev Publ Radiol Soc N Am Inc. 1995;15:551–61.
Rubin DA, Kettering JM, Towers JD, Britton CA. MR imaging of knees having isolated and combined ligament injuries. AJR Am J Roentgenol. 1998;170:1207–13.
Jung Y-B, Jung H-J, Yang JJ, Yang D-L, Lee YS, Song I-S, et al. Characterization of spontaneous healing of chronic posterior cruciate ligament injury: analysis of instability and magnetic resonance imaging. J Magn Reson Imaging JMRI. 2008;27:1336–40.
Ringler MD, Shotts EE, Collins MS, Howe BM. Intra-articular pathology associated with isolated posterior cruciate ligament injury on MRI. Skelet Radiol. 2016;45:1695–703.
Rodriguez W, Vinson EN, Helms CA, Toth AP. MRI appearance of posterior cruciate ligament tears. AJR Am J Roentgenol. 2008;191:1031.
Hong SH, Choi J-Y, Lee GK, Choi J-A, Chung HW, Kang HS. Grading of anterior cruciate ligament injury. Diagnostic efficacy of oblique coronal magnetic resonance imaging of the knee. J Comput Assist Tomogr. 2003;27:814–9.
Sonin AH, Fitzgerald SW, Friedman H, Hoff FL, Hendrix RW, Rogers LF. Posterior cruciate ligament injury: MR imaging diagnosis and patterns of injury. Radiology. 1994;190:455–8.
Cox MK, Key CH. Post hoc pair-wise comparisons for the Chi-square test of homogeneity of proportions. Educ Psychol Meas. 1993;53:951–62.
Ruxton GD, Neuhäuser M. Good practice in testing for an association in contingency tables. Behav Ecol Sociobiol. 2010;64:1505–13.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Spiridonov SI, Slinkard NJ, LaPrade RF. Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Joint Surg Am. 2011;93:1773–80.
Hamada M, Shino K, Mitsuoka T, Toritsuka Y, Natsu-Ume T, Horibe S. Chondral injury associated with acute isolated posterior cruciate ligament injury. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2000;16:59–63.
Geissler WB, Whipple TL. Intraarticular abnormalities in association with posterior cruciate ligament injuries. Am J Sports Med. 1993;21:846–9.
Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14:35–8.
Torg JS, Barton TM, Pavlov H, Stine R. Natural history of the posterior cruciate ligament-deficient knee. Clin Orthop. 1989;208–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived for individual participants included in the study. The study was approved by the local Institutional Review Board (IRB) and HIPAA compliant.
Rights and permissions
About this article
Cite this article
Anderson, M.A., Simeone, F.J., Palmer, W.E. et al. Acute posterior cruciate ligament injuries: effect of location, severity, and associated injuries on surgical management. Skeletal Radiol 47, 1523–1532 (2018). https://doi.org/10.1007/s00256-018-2977-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-018-2977-6