Abstract
Objective
To determine the ultrasonographic changes after steroid injection in carpal tunnel syndrome (CTS) and to evaluate the diagnostic value of ultrasound in post-treatment examination with clinical correlation.
Materials and methods
Twenty-seven wrists with idiopathic CTS after a single injection of 40 mg of prednisolone hydrochloride were prospectively studied using a high-resolution ultrasound. Axial images of the wrists were obtained at the level of the distal radius, pisiform and hamate prior to and 1, 4 and 8 weeks after steroid injection. The cross-sectional area (CSA, mm2) and flattening ratio (FR) of the median nerve were measured. The bowing of the flexor retinaculum (palmar displacement: PD, mm) and the transverse sliding distance of the median nerve (TSD, mm) during flexion-extension of the index finger were computed. Pre- and post-injection ultrasonographic findings were analyzed in relation to clinical parameters such as pain score.
Results
At all levels of the wrist, the CSA decreased significantly at 1 week after the injection, which continued to 8 weeks post-injection. The PD also diminished significantly 1 week after the injection. Furthermore, the TSD significantly increased from 1 week after injection, which lasted to the end of this study. The CSA, PD and TSD showed significant correlation with improvement of pain scores.
Conclusion
Ultrasound is useful in follow-up examinations of CTS. Significant ultrasound findings after steroid injections in CTS include decreased swelling of the median nerve, decreased bowing of the flexor retinaculum and increased mobility of the median nerve. All of them significantly correlate with clinical symptoms.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Carpal tunnel syndrome (CTS), the most common type of entrapment neuropathy, results from compression of the median nerve at the wrist. The diagnosis is usually based on the characteristic symptoms and signs as well as electrophysiological studies [1]. Electrodiagnostic studies are the most reliable methods of confirming the clinical diagnosis of CTS [2, 3]. However, 10–20% of these studies are falsely negative [4]. Although electrophysiological studies reveal the level of the lesion, they do not provide anatomical information about the nerve or its surroundings. In the last few years, ultrasonography (US) has become a useful diagnostic tool in CTS. US is advantageous given that it is non-invasive, inexpensive, readily available and displays real-time lesion anatomy [1, 4,5,6,7]. The clinical utility of high-resolution US in the diagnosis of CTS was first demonstrated by Buchberger et al. [5]. Variable diagnostic criteria and critical values have been previously described in order to diagnose CTS [1, 4, 5, 8]. Although many studies have investigated various anatomic locations within the forearm and wrist, as well as different sonographic techniques in the evaluation of the median nerve, the largest cross-sectional area (CSA) of the median nerve within the carpal tunnel region appears to be the most useful parameter in CTS [7, 9,10,11,12]. In some studies, dynamic US has been used to evaluate median nerve motion in CTS [13,14,15,16].
There are various treatment options for CTS, including nonsteroidal anti-inflammatory drugs, wrist splinting, steroid injections and surgery. Among these methods, steroid injection is an easy, safe and effective treatment that is frequently used [10, 17]. Despite the widespread use of local steroid injection for CTS, however, few prospective and quantitative trials have evaluated its utility. Several studies have investigated ultrasonographic changes following CTS surgery [18,19,20,21]; however, few have evaluated the sonographic changes after steroid injection [22,23,24]. Therefore, in this study, we determined the ultrasonographic changes after steroid injection in CTS and evaluated the diagnostic value of ultrasound in the post-treatment follow-up of steroid injections for CTS with clinical correlation.
Materials and methods
This clinical study was approved by the Institutional Review Board of our institution. Written informed consents were obtained from all participants.
Study participants
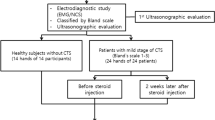
To define reference US standards for the diagnosis of CTS before steroid injection, patients with electrophysiologically documented CTS and a group of asymptomatic healthy control subjects were enrolled and underwent high-resolution US of the carpal tunnel. All patients were referred from the Department of Rehabilitation Medicine of our institution between January 2014 and January 2015. A clinical diagnosis of CTS was suspected based on the patient’s history (such as tingling, nocturnal hand discomfort and sensory impairment in the distribution of the median nerve) and specific clinical examinations (including positive Phalen test and Tinel sign) by one of the authors who had a specialty in electrodiagnostic medicine and musculoskeletal rehabilitation for 20 years. Their clinical diagnoses were confirmed by electrodiagnostic studies. In each case, routine motor and sensory nerve conduction studies, including mid-palm stimulation of the median sensory nerve, and needle EMG were performed. Participants were excluded if they had a history of surgery for CTS, wrist trauma or fracture, cervical radiculopathy or systemic conditions associated with neuropathy (e.g., diabetes mellitus, hypothyroidism, rheumatoid arthritis, chronic renal failure and pregnancy). Those who had received previous steroid injection or oral steroid therapy for CTS were also barred. In addition, participants with anatomical variants of the carpal tunnel (such as accessory muscles, bifid median nerves and persistent median arteries, as depicted with US) were excluded. The same exclusion criteria were applied to the control group, which consisted of 36 wrists from 21 asymptomatic female volunteers. All controls were examined with US, but not with electrophysiological studies. The observer bias in the interpretation of our US data could be avoided because US assessment was executed by one radiologist who had no idea of the results of the electrophysiological study.
Ultrasonography
Ultrasound evaluations were conducted using a Philips iU22 machine (Philips Healthcare, Bothell, WA) equipped with a 12-5-MHz linear array transducer. To ensure the reliability of measurement, all image processing and estimation were completed by the first author, a radiologist with 18 years of experience in musculoskeletal ultrasound. During the examination, the participants were positioned facing the examiner with their arms extended and wrists resting on a hard, flat surface. Their forearms were supinated with semi-extended fingers. A dedicated protocol with optimization of the scanning parameters (musculoskeletal superficial setting: frame rate: 38 Hz, 2D, 75% gain, 3rd gray map, depth: 2.5 cm, focus: 1-1.4 cm) was pre-programmed for the purpose of this study to ensure the consistency of the results obtained. All examinations were carried out according to the same protocol. Axial images of the wrists were obtained in the neutral position. The CSA and flattening ratio (FR, transverse diameter/anteroposterior diameter) of the median nerve were measured at the distal radioulnar joint, pisiform, and hamate levels. The CSA was computed by a direct continuous tracing around the margin of the median nerve. The tracing was executed along the inner border of the perineural echogenic rim around the hypoechoic nerve. The margin of the nerve referred to the margin outside the hypoechoic nerve fascicles and inside the hyperechoic nerve sheath [6]. We also measured the bowing of the flexor retinaculum, which was defined by the distance from the palmar apex of the retinaculum to a straight line drawn between the tubercle of trapezium and the hook of the hamate bone. Finally, the mobility of the median nerve in the carpal tunnel was observed dynamically. During passive flexion-extension of the second finger, the distance between the median nerve and ulnar artery was measured at each position respectively at the pisiform level; then, the transverse sliding distance (TSD) was defined as the difference in the distance between each motion (Fig. 1) [13].
Ultrasonographic technique to evaluate the transverse sliding of the median nerve. Transverse ultrasound of the wrist is performed dynamically during passive flexion (a) and extension (b) of the second finger on a specially designed plate. The transverse sliding of the median nerve at each motion is measured as the distance between the median nerve and ulnar artery, respectively. The transverse sliding distance (A-B) is calculated as the difference between flexion (c) and extension of the finger (d). MN: median nerve, UA: ulnar artery, P: pisiform. The ultrasonographic parameter setting (iU22, L12-5 MHz linear transducer, Philips Healthcare, Bothell, WA) is the musculoskeletal small part in the superficial setting.
Steroid injections
Under sterile conditions, a single injection of 1 ml 40 mg methylprednisolone acetate and 0.2 ml of 2% lidocaine was injected by the same physiatrist, who is the corresponding author. The needle was inserted in a distal and dorsal direction starting on the radial border of the pisiform bone. The needle was directed toward the middle portion of the carpal tunnel, thus immediately dorsal to the median nerve. Ideally, one should not experience any resistance at the final point of the injection. Following this, the syringe was disengaged from the needle, and another separate syringe with lidocaine was reattached and the solution was injected.
All patients were examined by the same radiologist using a high-resolution US at pre- and post-injection 1, 4 and 8 weeks.
The pain score using the visual analog scale (VAS) was also assessed at pre-injection and each follow-up after injection to document clinical improvement.
Statistical analysis
Statistical analyses were executed using the SPSS software program for Windows, version 19 (SPSS Inc., Chicago, IL). The arithmetic mean values and standard deviation of the data were determined, and T-test and chi-square goodness of fit tests were performed to test the normal distribution of the data. Unpaired t-tests were used to compare US quantitative measurements between patients and controls. The ultrasonographic changes on serial evaluations after steroid injection were analyzed using repeated measures analysis of variance (ANOVA). The correlations between US changes and pain scores were assessed with Spearman’s correlation coefficients (r). For all analyses, p-values less than 0.05 were considered statistically significant.
Results
Table 1 summarizes the measured values in CTS patients and controls. A total 104 wrists from 58 women with electrodiagnostically proven idiopathic CTS (mean age, 53 years; range, 35–75 years) were included. The average duration of the disease at the time of inclusion was 5 years (range, 1 month to 20 years). Thirty-six age-matched wrists from 21 asymptomatic healthy female volunteers (mean age, 49 years; range, 33–69 years) were recruited as the control. There was no significant difference in demographic data such as height, weight and distribution of right versus left wrists between the two groups.
The CSA increased significantly at all levels of the carpal tunnel in the patient group compared to the control group (p < 0.0001). The FR of the median nerve increased significantly in the patient group, but only at the hamate level, suggesting that the nerve is more likely constricted at the distal part of the tunnel (p = 0.0001). The PD of the flexor retinaculum also increased significantly in the patient group (p = 0.0001). In addition, the TSD of the median nerve on flexion-extension of the index finger decreased significantly in the patient group (p < 0.0001).
Among the patient group, 27 wrists from 18 patients with electodiagnostically and ultrasonographically diagnosed CTS were serially followed up after steroid injection. Their mean age was 52 years (range, 35–67 years), affecting the right hand in 17 and left hand in 10. Table 2 demonstrates serial US findings of the ultrasonographic parameters and pain score (VAS) before and after steroid injection in CTS patients. The CSA of the median nerve at all levels of the wrist decreased significantly at 1 week after injection (Fig. 2), which continued to 8 weeks post-injection (p < 0.0001). However, the FR did not change significantly. The PD diminished significantly starting 1 week after steroid injection (p = 0.0001) (Fig. 3). Furthermore, the TSD increased significantly at 1 week post-injection, lasting to the end of this study (p = 0.0001) (Fig. 4). Pain scores significantly improved from 1 week after steroid injection, which lasted to 8 weeks (p = 0.0001).
A 52-year-old female with right carpal tunnel syndrome. a. Axial sonogram of the wrist at the pisiform level shows an enlarged hypoechoic median nerve (arrow), with the cross-sectional area measured as 15 mm2. b. At 1 week after steroid injection, axial sonogram of the wrist reveals substantially decreased swelling of the median nerve (arrow), with the cross-sectional area as 9.6 mm2. MN: median nerve
A 49-year-old female with right carpal tunnel syndrome. a Axial sonogram at the hook of the hamate level shows increased palmar bowing of the flexor retinaculum. Palmar displacement of the flexor retinaculum is computed as 4.2 mm. b At 8 weeks after steroid injection, axial sonogram of the wrist reveals decreased palmar displacement, measured as 2.8 mm. PD: palmar displacement
Transverse sliding distance (TSD) of the median nerve in a 47-year-old female with right carpal tunnel syndrome. Axial sonograms of the wrist during flexion (a) and extension (b) of the index finger show nearly no difference in transverse sliding of the median nerve between two motions, with TSD of 0.1 mm. At 4 weeks after steroid injection, axial sonograms of the wrist during flexion (c) and extension (d) of the finger reveal increased TSD, calculated as 1.4 mm. MN: median nerve, UA: ulnar artery
Table 3 shows the results of the correlation analysis between the ultrasonographic changes and pain scores after steroid injection. There was a good positive correlation between the CSA of all levels, PD and symptom improvement (p < 0.0001). A statistically significant negative correlation was also observed between the TSD of the median nerve and pain score (p < 0.0001). However, no relationship between the FR and symptom was observed.
Discussion
CTS is a compressive neuropathy of the median nerve at the wrist caused by elevated pressure within the carpal tunnel. Compression of the median nerve leads to impaired nerve perfusion, endoneurial edema, inflammation, fibrosis and thickening of the perineurium and endoneurium. Enlargement of the median nerve and increased CSA on sonography reflect these processes [15, 25,26,27]. Recently, newer US techniques such as color and power Doppler [10, 12, 15] and elasatography [28] have been introduced to assess the intraneural vascularity of the median nerve or to measure the stiffness of the tissue. However, these studies have not been yet extensively studied with regard to reliability.
The ultrasonographic criteria for CTS include proximal median nerve swelling, distal nerve flattening and bowing of the flexor retinaculum [1, 4, 5, 8, 25]. The most consistent diagnostic criterion in the literature for CTS is measurement of the CSA of the median nerve within the carpal tunnel at the level of the pisiform [4, 6, 7, 9, 12, 29]. Buchberger et al. performed measurements of the median nerve at three levels, which allowed for a more complete morphological assessment of the enlarged nerve [8]. In this study, we also computed the CSA of the median nerve at the three levels. The CSA measurements at each level were significantly higher in the patients than in the controls (p < 0.0001). Among all three levels, the CSA at the pisiform level was the highest.
Prior studies have suggested that the FR is highly variable and therefore poorly predictive of CTS [4]. In addition, nerve flattening has not been consistently useful in the diagnosis of CTS [9, 30, 31]. However, we found that the FR of the median nerve increased significantly at the hamate level, which is consistent with findings from several prior studies [5, 8, 15, 26, 29, 32].
Swelling of the median nerve itself and increased inflammation of the nerve or tendons may account for the increased retinacular bowing that is observed in individuals with CTS [5, 8, 15]. Previous research has been inconclusive regarding the utility of retinacular bowing (palmar displacement, PD), possibly because of the difficulty in obtaining clear images of the retinaculum in the distal carpal tunnel [33]. Regardless, we observed differences in the retinacular bulge between the patients and the controls in this study.
We also found that patients with CTS had significantly reduced median nerve mobility under the flexor retinaculum in the axial plane during passive flexion-extension of the index finger compared to the normal controls. The authors estimated the mobility of the median nerve and quantified the sliding distance using a method outlined by Nakamichi et al. [13]. This immobility may be related to fibrosis and adherence of the median nerve to the retinaculum and/or increased carpal tunnel pressure in CTS [13,14,15,16]. Kang et al. [16] also reported that movement of the median nerve decreased significantly during finger flexion in the transverse plane, and this parameter correlated negatively with CTS severity. The sliding of the median nerve in the control group indicates that the nerve physiologically changes its position in relation to the motion of the flexor tendons. As the index finger is passively extended, the flexor digitorum superficialis and profundus tendons produce a combined force on the dorsal and radial aspects of the median nerve, pushing it in an ulnar direction [13]. Decreased sliding indicates that this physiologic motion is significantly restricted in patients with CTS.
Several modalities are available in the treatment of CTS. One conservative management approach frequently used in the outpatient setting is local steroid injection. Corticosteroid injection is a well-established treatment option for mild to moderate CTS. Injections relieve local ischemia, inflammation, synovial swelling around the median nerve and vascular congestion in the carpal tunnel [10, 22]. Steroid injections are also very safe with few local complications. Median nerve damage from intraneural injection has been estimated to occur in less than 0.1% of cases [34].
US can be used to monitor the therapeutic response following corticosteroid injection. Compared to several publications on its value in the evaluation of the treatment efficacy in postoperative CTS (from 2 weeks to 12 months) [18,19,20,21, 35,36,37], there are few papers evaluating the ultrasonographic changes after steroid injection [22,23,24]. Postoperatively, US examinations of the carpal tunnel typically focus on the CSA of the median nerve at its widest site and the comparison between these values obtained pre- and postoperatively. Some reports emphasize the relationship between the CSA of the median nerve and clinical symptoms in CTS [21, 36, 37]. However, others argue that there is no consensus regarding the utility of the CSA of the median nerve as a predictor of postoperative outcomes [18, 35]. Naranjo et al. [38] found that ultrasound imaging is of limited value.
Jeong et al. [22] demonstrated a significant reduction in the CSA of the median nerve following steroid injection. Most of the improvements occurred during the first month after the injection and lasted for up to 6 months. We also found that the CSA of the median nerve was significantly reduced at all levels after steroid injection starting from 1 week. Another study identified the structural and functional changes in the median nerve following steroid injection using US and electrophysiological studies [23]. They identified significant improvement in the CSA, mobility and vascularity of the median nerve after steroid injection. Those changes in the ultrasonographic parameters were seen within 1 week of steroid injection. In addition, CSA correlated with the symptom score and electrodiagnositc parameters. Our study also showed that the mobility of the median nerve (TSD) after steroid injection increased significantly.
Karadas et al. [24] reported that there were significant improvements in the median nerve anterior-posterior diameter, transverse diameter, CSA at the proximal carpal tunnel and volar bulging after steroid injection. In our study, the PD of the flexor retinaculum also decreased significantly after the procedure. Meys et al. reported that patients who did not undergo surgery within 1 year after steroid injection had a lower median nerve CSA, lower swelling ratio and lower symptom severity score [39].
In this study, mean pain scores (VAS) significantly decreased at 1 week (3.85), 4 weeks (2.85) and 8 weeks (2.56) post-injection when compared to pre-injection (5.93) (p = 0.0001). There was a good positive correlation between the CSAs of all levels (r = 0.4102, 0.3546, 0.4897), PD (r = 0.3890) and pain score, whereas significant negative correlation between TSD (r = − 0.3912) and symptom (r = Spearman’s correlation coefficient, p < 0.0001).
This study has some limitations. It was a single institutional study with a small sample size of patients. In addition, ultrasound examinations were done by one radiologist not completely blinded to the clinical history, thus possibly exposing the results to expectation bias. Therefore, further studies will be necessary to analyze larger numbers of CTS patients and longer follow-up after steroid injection.
In this study, we demonstrated that the median nerve was significantly swollen at all levels of the carpal tunnel in CTS. The nerve was more likely to be compressed at the most distal part of the tunnel than at its more proximal regions. The physiologic mobility of the nerve was significantly restricted. There was significant improvement of US findings starting form 1 week after steroid injection, which continued to 8 weeks post-injection. These US changes have meaningful correlation with symptom improvement such as the pain score. These results provide morphological evidence of the therapeutic benefit of local steroid injection in patients with CTS. In conclusion, significant ultrasound findings after steroid injection in CTS included decreased swelling of the median nerve, decreased bowing of the flexor retinaculum and increased mobility of the median nerve during finger motion. Ultimately, ultrasound evaluation is not only useful in the diagnosis of CTS, but also in follow-up evaluation of therapeutic interventions, significantly correlating with symptoms in select cases.
References
Beekman R, Visser LH. Sonography in the diagnosis of carpal tunnel syndrome: a critical review of the literature. Muscle Nerve. 2003;27(1):26–33.
Nathan PA, Keniston RC, Meadows KD, Lockwood RS. Predictive value of nerve conduction measurements at the carpal tunnel. Muscle Nerve. 1993;16(12):1377–82.
Padua L, LoMonaco M, Gregori B, Valente EM, Padua R, Tonali P. Neurophysiological classification and sensitivity in 500 carpal tunnel syndrome hands. Acta Neurol Scand. 1997;96(4):211–7.
Duncan I, Sullivan P, Lomas F. Sonography in the diagnosis of carpal tunnel syndrome. AJR Am J Roentgenol. 1999;173(3):681–4.
Buchberger W, Schön G, Strasser K, Jungwirth W. High-resolution ultrasonography of the carpal tunnel. J Ultrasound Med. 1991;10(10):531–7.
Wong SM, Griffith JF, Hui AC, Lo SK, Fu M, Wong KS. Carpal tunnel syndrome: diagnostic usefulness of sonography. Radiology. 2004;232(1):93–9.
Junck AD, Escobedo EM, Lipa BM, et al. Reliability assessment of various sonographic techniques for evaluating carpal tunnel syndrome. J Ultrasound Med. 2015;34(11):2077–88.
Buchberger W, Judmaier W, Birbamer G, Lener M, Schmidauer C. Carpal tunnel syndrome: diagnosis with high-resolution sonography. AJR Am J Roentgenol. 1992;159(4):793–8.
Roll SC, Evans KD, Li X, Freimer M, Sommerich CM. Screening for carpal tunnel syndrome using sonography. J Ultrasound Med. 2011;30(12):1657–67.
McDonagh C, Alexander M, Kane D. The role of ultrasound in the diagnosis and management of carpal tunnel syndrome: a new paradigm. Rheumatology. 2015;54(1):9–19.
Yurdakul OV, Mesci N, Çetinkaya Y, Geler KD. Diagnostic significance of ultrasonographic measurements and median-ulnar ratio in carpal tunnel syndrome: correlation with nerve conduction studies. J Clin Neurol. 2016;12(3):289–94.
Chen YT, Williams L, Zak MJ, Fredericson M. Review of ultrasonography in the diagnosis of carpal tunnel syndrome and a proposed scanning protocol. J Ultrasound Med. 2016;35(11):2311–24.
Nakamichi K, Tachibana S. Restricted motion of the median nerve in carpal tunnel syndrome. J Hand Surg Br. 1995;20(4):460–4.
Yoshii Y, Ishii T, Tung WL, Sakai S, Amadio PC. Median nerve deformation and displacement in the carpal tunnel during finger motion. J Orthop Res. 2013;31(12):1876–80.
Ooi CC, Wong SK, Tan AB, et al. Diagnostic criteria of carpal tunnel syndrome using high-resolution ultrasonography: correlation with nerve conduction studies. Skelet Radiol. 2014;43(10):1387–94.
Kang HJ, Yoon JS. Effect of finger motion on transverse median nerve movement in the carpal tunnel. Muscle Nerve. 2016;54(4):738–42.
Hagebeuk EE, de Weerd AW. Clinical and electrophysiological follow-up after local steroid injection in the carpal tunnel syndrome. Clin Neurophysiol. 2004;115(6):1464–8.
Smidt MH, Visser LH. Carpal tunnel syndrome: clinical and sonographic follow-up after surgery. Muscle Nerve. 2008;38(2):987–91.
Abicalaf CA, de Barros N, Sernik RA, et al. Ultrasound evaluation of patients with carpal tunnel syndrome before and after endoscopic release of the transverse carpal ligament. Clin Radiol. 2007;62(9):891–4.
Inui A, Nishimoto H, Mifune Y, Kokubu T, Sakata R, Kurosaka M. Ultrasound measurement of median nerve cross-sectional area at the inlet and outlet of carpal tunnel after carpal tunnel release compared to electrodiagnostic findings. Arch Orthop Trauma Surg. 2016;136(9):1325–30.
Kapuścińska K, Urbanik A. Efficacy of high frequency ultrasound in postoperative evaluation of carpal tunnel syndrome treatment. J Ultrason. 2016;16(64):16–24.
Jeong JS, Yoon JS, Kim SJ, et al. Usefulness of ultrasonography to predict response to injection therapy in carpal tunnel syndrome. Ann Rehabil Med. 2011;35(3):388–94.
Cartwright MS, White DL, Demar S, et al. Median nerve changes following steroid injection for carpal tunnel syndrome. Muscle Nerve. 2011;44(1):25–9.
Karadaş O, Omaç OK, Tok F, Ozgül A, Odabaşi Z. Effects of steroid with repetitive procaine HCl injection in the management of carpal tunnel syndrome: an ultrasonographic study. J Neurol. 2012;316(1-2):76–8.
Bayrak IK, Bayrak AO, Tilki HE, Nural MS, Sunter T. Ultrasonography in carpal tunnel syndrome: comparison with electrophysiological stage and motor unit number estimate. Muscle Nerve. 2007;35(3):344–8.
Lu Y, Meng Z, Pan X, Qin L, Wang G. Value of high-frequency ultrasound in diagnosing carpal tunnel syndrome. Int J Clin Exp Med. 2015;8(12):22418–24.
Ajeena IM, Al-Saad RH, Al-Mudhafar A, Hadi NR, Al-Aridhy SH. Ultrasonic assessment of females with carpal tunnel syndrome proved by nerve conduction study. Neural Plast. 2013;2013:754564.
Orman G, Ozben S, Huseyinoglu N, Duymus M, Orman KG. Ultrasound elastographic evaluation in the diagnosis of carpal tunnel syndrome: initial findings. Ultrasound Med Biol. 2013;39(7):1184–9.
Azami A, Maleki N, Anari H, Iranparvar Alamdari M, Kalantarhormozi M, Tavosi Z. The diagnostic value of ultrasound compared with nerve conduction velocity in carpal tunnel syndrome. Int J Rheum Dis. 2014;17(6):612–20.
Sarría L, Cabada T, Cozcolluela R, Martínez-Berganza T, García S. Carpal tunnel syndrome: usefulness of sonography. Eur Radiol. 2000;10(12):1920–5.
Keleş I, Karagülle Kendi AT, Aydin G, Zöğ SG, Orkun S. Diagnostic precision of ultrasonography in patients with carpal tunnel syndrome. Am J Phys Med Rehabil. 2005;84(6):443–50.
Elsaman AM, Thabit MN, Radwan AR, Ohrndorf S. Idiopathic carpal tunnel syndrome: evaluation of the depth of the carpal tunnel by ultrasonography. Ultrasound Med Biol. 2015;41(11):2827–35.
Roll SC, Case-Smith J, Evans KD. Diagnostic accuracy of ultrasonography vs. electromyography in carpal tunnel syndrome: a systematic review of literature. Ultrasound Med Biol. 2011;37(10):1539–53.
Bland JD. Carpal tunnel syndrome. BMJ. 2007;335(7615):343–6.
Kim JK, Koh YD, Kim JO, Choi SW. Changes in clinical symptoms, functions, and the median nerve cross-sectional area at the carpal tunnel inlet after open carpal tunnel release. Clin Orthop Surg. 2016;8(3):298–302.
Mondelli M, Filippou G, Aretini A, Frediani B, Reale F. Ultrasonography before and after surgery in carpal tunnel syndrome and relationship with clinical and electrophysiological findings. A new outcome predictor? Scand J Rheumatol. 2008;37(3):219–24.
Oh WT, Kang HJ, Koh IH, Jang JY, Choi YR. Morphologic change of nerve and symptom relief are similar after mini-incision and endoscopic carpal tunnel release: a randomized trial. BMC Musculoskelet Disord. 2017;18(1):65.
Naranjo A, Ojeda S, Rúa-Figueroa I, Garcia-Duque O, Fernández-Palacios J, Carmona L. Limited value of ultrasound assessment in patients with poor outcome after carpal tunnel release surgery. Scand J Rheumatol. 2010;39(5):409–12.
Meys V, Thissen S, Rozeman S, Beekman R. Prognostic factors in carpal tunnel syndrome treated with a corticosteroid injection. Muscle Nerve. 2011;44(5):763–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consents were obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Lee, Y.S., Choi, E. Ultrasonographic changes after steroid injection in carpal tunnel syndrome. Skeletal Radiol 46, 1521–1530 (2017). https://doi.org/10.1007/s00256-017-2738-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-017-2738-y