Abstract
Objective
The aim of this study was to evaluate the safe zone for performing blind sternal procedures based on computed tomography (CT) evaluation of congenital midline sternal foramina using multidetector computed tomography (MDCT).
Materials and methods
This retrospective study was carried out on 1,180 patients who underwent MDCT of the thorax from March 2015 to February 2016. The MDCT images were evaluated in axial and reformatted planes. Morphometry and prevalence of midline congenital sternal foramina (SF) and manubrio-foraminal distance (MFD) were evaluated. The safe zone was defined for a blinded intervention, based on palpable anatomical landmarks. Data were presented in terms of percentage, mean ± standard deviation and calculations were carried out using Microsoft Excel.
Results
The prevalence of SF in our study sample was 11.6 %. The majority of SF were located in a typical position in the lower sternal body at the level of fifth costo-chondral junction (CCJ) in 108 patients (78.8 %). The structure directly beneath the SF was mediastinal fat in 73 patients (53.3 %), followed by anterior pericardium in 44 patients (32.1 %) and lung parenchyma in 20 patients (14.6 %). The mean MFD in our study population was 11.90 ± 1.31 cm.
Conclusions
Sternal interventions should be avoided at the level of fourth to sixth CCJ, which is considered the danger zone. An intervention at the fourth to sixth CCJ may lead to disastrous consequences in patients who have SF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sternal foramina (SF) refer to congenital midline defects in the sternum. They occur as a result of developmental defects in the sternum due to incomplete fusion of the sternal ossification centers. Riolanus (1649) reported that the first description of SF in the mesosternum was made by Massa (cited in Ashley [1]). SF can be observed in the manubrium, body, and xiphoidal process. The most common location for the SF is in the lower sternal body. The close contact of SF to vital structures of the thorax predisposes to the risk of life-threatening complications during sternal puncture or bone marrow biopsy [2, 3]. Hence, knowledge of SF is essential because of the potential danger of cardiac tamponade, pneumothorax, pneumo-mediastinum or pneumo-pericardium, which may occur secondary to inadvertent insertion of the needle through SF during bone marrow aspiration (BMA), bone marrow biopsy [4] or acupuncture [3]. SF also have forensic importance because they can lead to erroneous autopsy results in criminal cases [5], where they can be mistaken for penetrating injuries.
The aim of this study was to evaluate the safe zone for performing blind sternal procedures based on the evaluation of the manubrio-foraminal distance (MFD) in patients with congenital midline sternal foramina using multidetector computed tomography (MDCT). The present study cohort to our knowledge comprises the largest number of sternal foramina studied in any given population.
Materials and methods
Patient selection
We retrospectively evaluated a total of 1,180 consecutive chest CTs during a 1-year period from March 2015 to February 2016. The chest MDCTs were performed for other indications, such as to investigate primary or metastatic tumors, trauma, and vascular and airway pathological conditions. Repeat CTs were excluded. We also excluded patients with gross sternal deformities, previous sternotomy, sternal fractures, sternal masses, and infections. A total of 1,180 chest CTs met these criteria. All 1,180 chest CTs were reviewed for the existence of foramen in the sternal body, out of which, 137 showed the presence of sternal foramina.
CT protocol
The MDCT examinations were performed using a 64-slice scanner (Aquilion 64; Toshiba Medical Systems Corporation, Tokyo, Japan). The same parameters (120 kV, 100 mAs, 1-mm slice thickness, and automatic exposure control) were used in all patients. Chest MDCTs were acquired during a breath-hold in deep inspiration.
Data evaluation
Analysis of the MDCT image data was based on axial and reformatted images. All images were evaluated in the axial plane followed by sagittal and coronal multiplanar reconstruction (MPR). Maximum intensity projection (MIP) and surface shaded display (SSD) images were also evaluated. Two experienced radiologists evaluated the images with a consensus on the presence and morphometry of midline sternal body foramen and MFD.
All CTs were reviewed and relationships of SF to intra-thoracic organs such as mediastinal fat, lung, and pericardium were evaluated. We measured the MFD in all these patients, which we define as the vertical distance between the superior margin of the manubrium sterni to the superior margin of the SF. The other morphometric parameters evaluated were: width and height of the foramen, mediastinal structures directly beneath the foramen, location of the SF according to the level of the costo-chondral junction (CCJ), distance from the posterior surface of the foramen to the underlying vital structure, and distance from the skin to the anterior pericardium. A correlation between the thickness of the subcutaneous fat and the distance to a vital structure was performed.
Statistical analysis
The collected data were presented in terms of percentage, mean ± standard deviation, and calculations were carried out using Microsoft Excel.
Results
The mean age was 38 years in our study sample of 1,180 patients, with a male:female ratio of 2.2:1. The prevalence of SF in our study sample was 11.6 %. Among the 137 patients with SF in the final study group, the mean age of patients was 45 years, with a male:female ratio of 2.5:1. The majority of SF were located in a typical position in the lower sternal body at the level of the fifth CCJ in 108 patients (78.8 %), at the sixth CCJ in 19 patients (13.9 %), and at the fourth CCJ in 10 patients (7.3 %; Table 1).
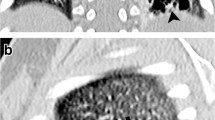
The mean width of the SF was 5.58 ± 2.28 mm (range 1.3–15.1 mm) and the mean height was 6.66 ± 3.36 mm (range 1.6–18.6 mm). The important measurements have been summarized in Table. 2. The structure directly beneath the SF (Table 3) was mediastinal fat in 73 patients (53.3 %; Fig. 1) followed by the anterior pericardium in 44 (32.1 %; Fig. 2) and the lung parenchyma in 20 patients (14.6 %; Fig. 3). The mean MFD was 11.90± 1.31 cm.
A 25-year-old man who had a midline sternal foramen (SF) with mediastinal fat beneath the SF. a, b Unenhanced axial and c, d reconstructed coronal and sagittal computed tomography (CT) images in a bone algorithm showed a well-defined oval-shaped midline bony defect in the lower third of the sternal body at the level of the fourth and fifth costo-chondral junctions (CCJ) with mediastinal fat beneath the SF (b, d). e surface shaded display (SSD) images showed the bony defect
A 37-year-old man with SF and a sclerotic band below the SF in whom the lung parenchyma was just behind the sternal foramen. a Coronal reformatted maximum intensity projection (MIP) image showed the SF with a thin dense midline sclerotic sternal band below the SF. b Axial lung and mediastinal window CT images showed direct contact of the lung parenchyma with SF (white arrow)
Distance from the SF to any vital structure was 4.84 ± 3.96 mm. The mean distance from the skin to the pericardium was 21.53 ± 8.85 mm.
The distribution of other associated sternal anomalies have been summarized in Fig. 4. A sternal cleft below the SF was noted in 7 of our patients (5.1 %), giving a “key-hole” appearance (Fig. 5). Ten (7.3 %) patients had a suprasternal tubercle, among which 3 patients (2.2 %) had a unilateral suprasternal tubercle (Fig. 6a) and 7 patients (5.1 %) had bilateral suprasternal tubercles (Fig. 6b, c). The suprasternal bone was noted in 3.7 % of patients, where 3 patients (2.2 %) had bilateral para-median suprasternal bones (Fig. 7a, b) and 2 patients (1.5 %) had a single midline suprasternal bone (Fig. 7c, d). Thirty-one patients (22.6 %) had both manubrio-sternal and sterno-xiphoidal fusions, whereas 26 patients (19 %) had manubrio-sternal fusion only and 17 (12.4 %) had sterno-xiphoidal fusion only (Fig. 8). Seven patients (5.1 %) had a sclerotic sternal band below the SF (Fig. 9) whereas 1 patient (0.7 %) had a sclerotic band over the SF. Twelve patients with a midline sternal body foramen (8.7 %) had associated xiphoidal foramina. A nodular dense sclerotic lesion was noted in 1 patient (0.7 %) in the lower third of the sternal body at the level of the fifth CCJ, which was a probable site of SF (Fig. 10).
a A 67-year-old man with SF and a right suprasternal tubercle. Coronal MIP image showed a peg-like right supra-sternal tubercle from the manubrium along with the SF. b, c. A 34-year-old man with SF and bilateral suprasternal tubercles. Coronal reformatted MIP and SSD images showed bilateral supra-sternal tubercles along with SF. Fusion of the manubrio-sternal junction was also noted
a, b A 29-year-old man with SF and bilateral para-median suprasternal bones. Coronal SSD and MIP images showed well-defined bilateral para-median suprasternal bones (arrow) just superior to the manubrium sterni along with SF. c, d A 36-year-old man with a midline suprasternal bone. Coronal SSD and MIP images showed a well-defined midline suprasternal bone (arrow) superior to the manubrium sterni along with a SF. Fusion of the manubrio-sternal junction was also seen
A 65-year-old woman with SF, manubrio-sternal and sterno-xiphoidal fusions and a xiphoid foramen. a Coronal reconstructed MIP image and b SSD image showed a midline lower sternal body foramen with complete manubrio-sternal and sterno-xiphoidal fusions. A single midline foramen was also seen in the xiphoid process (white arrow in a)
Discussion
The important findings in our study are that SF are typically located in the lower sternal body at the level of fifth CCJ in 78.8 % patients followed by the sixth CCJ in 13.9 % patients and the fourth CCJ in 7.3 % patients. The structure directly beneath the SF was mediastinal fat in 53.3 % patients followed by the anterior pericardium in 32.1 % and lung parenchyma in 14.6 % patients. The mean MFD was 11.90 cm ± 1.31 cm.
Embryologically, the sternum is formed by the cranio-caudal fusion of two sternal bars, which are condensations of mesenchymal tissue that are converted to pre-cartilage before fusion. Any defect in such midline fusion may lead to congenital anomalies such as foramina or cleft sternum or a hybrid deformity such as a key-hole shaped deformity in the sternum [6–8]. They have been reported in the manubrium, body, and xiphisternum [9–11]. Usually, the defect occurs in the lower third of the body of the sternum [12] as a single midline oval or round foramen. Xiphoid abnormalities are uncommon compared with defects of the manubrium and gladiolus [5, 13].
All these fusion defects of the sternum are usually asymptomatic and can be well demonstrated only by CT [14]. A complete fusion defect leads to a cleft sternum, whereas partial fusion defects lead to SF. Failure of fusion may be due to an early disturbance affecting midline mesodermal structures during the 6th to 9th weeks of gestation.
The incidence of SF was evaluated in previous literature as 4.3 % by Stark [12] using chest CT, 6.7 % in autopsy cases by Cooper [11], and 6.6 % by Moore et al. [10]. Aktan and Savas observed it in 5.1 % among a Turkish population [15] and Yekeler et al. stated an incidence of 4.5 % [4]. In our study we noted an incidence of 11.6 %. A high incidence of 16.6 % of this variation was observed in cadavers and dry bones by Babinski et al. [16]. According to Yekeler et al., MDCT showed the size of SF ranging between 2 and 16 mm, with a mean of 6.5 mm [4]. In our study, we observed a mean width of 5.58 ± 2.28 mm and a height of 6.66 ± 3.36 mm. Most of the SF were located in the lower part of the sternal body at the fifth CCJ, accounting for 78.8 %. The imaging appearances of the sternal variation and anomalies are necessary to differentiate SF from pathological conditions, such as traumatic fissure or fracture and lytic lesions [6, 17]. Cortical irregularity, bone expansion, and associated soft-tissue mass are usually not associated with SF and these features differentiate them from other mimickers. It is difficult to visualize sternal variations and anomalies by plain radiography. However, cross-sectional imaging, mainly MDCT, shows anatomical details of the sternum and its variations.
The MDCT showed a “bow-tie” defect at the level of SF in axial sections (Fig. 1), whereas in sagittal reconstruction SF presented as defects in the continuity of the sternum. In coronal reconstruction, SF was seen as oval or circular defects with or without mild surrounding sclerosis. On scintigraphy and single photon emission tomography, SF are seen as a distinct area of photopenia [14, 18].
The clinical importance of SF lies in the fact that a fatal cardiac tamponade can occur following insertion of a needle through the sternal defect. The sternum is one of the bones chosen for bone marrow aspiration in hematological diseases. Other bony sites for bone marrow aspiration (BMA) are iliac crest in adults and tibial shin in infants. Improper needling during BMA may lead to cardiac tamponade or great vessel injury [19, 20]. Another importance of the sternum is that the acupuncture point CV-17 (Danchu or Shanzong or sea of energy) is located at the level of the nipples in the midline. Vertical insertion of an acupuncture needle can lead to pericardial effusion or cardiac tamponade [17, 21].
In forensic investigations, the SF could be misinterpreted as bullet injuries or other ante-mortem penetrating injuries. The misinterpretation of such sternal defects in medico-legal cases can be a serious pitfall in determining the nature and cause of death in cases of homicide and suicide [2]. Hence, its awareness is extremely important to the autopsy pathologist.
A deep sternal notch can resemble SF. However, in a sternal notch there will be deep defects in the cortical bones of the sternum with an intervening bony bar in between the anterior and posterior bony cortices (Fig. 11), whereas SF have complete bony cortical defects.
Sternal foramina can also be misinterpreted as osteolytic lesions on cross-sectional imaging of the sternum. However, observation of a midline smoothly margined bony defect can clinch the diagnosis of congenital SF. Midline SF should be differentiated from other osteolytic lesions in the sternum. The other common solitary osteolytic lesions in the sternum are simple bone cyst (SBC), eosinophilic granuloma, aneurysmal bone cyst (ABC), chondroma, chondrosarcoma, giant cell tumor of bone (GCT), and osteosarcoma [22]. Plasmacytoma and osteolytic metastasis can occur in the sternum, usually in elderly individuals. The usual differential diagnosis for SF in young children is SBC, whereas in adults it is ABC and GCT. Even though SBC simulates most features of congenital midline SF, its location is usually paramedian (Fig. 12). ABC of the sternum is a locally destructive lesion characterized by the presence of a spongy or multiloculated cyst. Blood–fluid levels are commonly seen in ABC and well demonstrated on MRI.
Although this was to our knowledge the largest study group involving SF on CT, there were certain limitations. The MFD and other parameters may vary with race, especially with the western population, and in future such studies are required in different population groups. However, the consistent presence of SF at the level of the fifth CCJ was an interesting and notable finding in our study. Hence, any sternal intervention is best avoided from the fourth to sixth CCJ. The relatively higher incidence of SF in our study group in comparison with previous ante-mortem studies is probably due to the improved MDCT imaging, providing better reformatted images, thereby identifying more patients with SF. However, postmortem studies have resulted in a significantly higher prevalence.
Conclusions
Sternal foramen is a minor variation with important clinico-radiological and forensic relevance, and awareness of its existence is of utmost importance for the physician to avoid inadvertent complications during BMA. Bone marrow biopsy should ideally be performed in the iliac crest and sternal biopsy should be avoided. If needed, it can be performed safely after previous CT of the thorax and after ruling out the presence of SF, or it has to be performed under image guidance. Sternal interventions should be avoided at the level of fourth to sixth CCJ, which is considered the danger zone.
References
Ashley GT. The relationship between the pattern of ossification and the definitive shape of the mesosternum in man. J Anat. 1956;90(1):87–105.
Van Marum RJ, Velde LT. Cardiac tamponade following sternal puncture in two patients. Neth J Med. 2001;59(1):39–40.
Halvorsen TB, Anda SS, Naess AB, Levang OW. Fatal cardiac tamponade after acupuncture through congenital sternal foramen. Lancet. 1995;345(8958):1175.
Yekeler E, Tunaci M, Tunaci A, Dursun M, Acunas G. Frequency of sternal variations and anomalies evaluated by MDCT. Am J Roentgenol. 2006;186:956–60.
Taylor HL. The sternal foramen: the possible forensic misinterpretation of an anatomic abnormality. J Forensic Sci. 1974;19(4):730–4.
Saccheri P, Sabbadini G, Toso F, Travan L. A keyhole shaped sternal defect in an ancient human skeleton. Surg Radiol Anat. 2012;34(10):965.
McCormick WF. Sternal foramena in man. Am J Forensic Med Pathol. 1981;2:249–52.
Fokin AA. Cleft sternum and sternal foramen. Chest Surg Clin N Am. 2000;10:261–76.
Shivakumar GL, Deepa G, Kadlimatti HS. Variations in human sterna. J Evol Med Dent Sci. 2013;2(2):99–104.
Moore MK, Stewart JH, McCormick WF. Anomalies of the human chest plate area: radiographic findings in a large autopsy population. Am J Forensic Med Pathol. 1988;9(4):348–54.
Cooper PD, Stewart JH, McCormick WF. Development and morphology of the sternal foramen. Am J Forensic Med Pathol. 1988;9(4):342–7.
Stark P. Midline sternal foramen: CT demonstration. J Comput Assist Tomogr. 1985;9:489–90.
Collin T, Cox C. Chest wall and breast. In: Standring S, editor. Gray’s anatomy: the anatomical basis of clinical practice. 40th ed. Edinburgh: Churchill Livingstone Elsevier; 2008. p. 917–18.
Pevenage P, De Maeseneer M, Muylle K, Osteaux M. Sternal foramen simulating osteolytic lesion on scintigraphy and SPET imaging. Ann Nucl Med Sci. 2002;15(4):227–30.
Aktan ZA, Savas R. Anatomic and HRCT. Demonstration of midline sternal foramina. Turk J Med Sci. 1998;28:511–4.
Babinski MA, Rafael FA, Steil AD, et al. High prevalence of sternal foramen: quantitative, anatomical analysis and its clinical implications in acupuncture practice. Int J Morphol. 2012;30(3):1042–9.
Kirchgatterer A, Schwarz D, Hoeller E. Cardiac tamponade following acupuncture. Chest. 2000;117:1510–1.
Ishii S, Shishido F, Miyajima M, et al. Causes of photopenic defects in the lower sternum on bone scintigraphy and correlation with multidetector CT. Clin Nucl Med. 2011;36(5):355–8.
Wolochow MS. Fatal cardiac tamponade through congenital sternal foramen. Lancet. 1995;346:442.
Pascali VL, Lazzaro P, Fiori A. Is sternal bone marrow needle biopsy still a hazardous technique? Report of three further fatal cases. Am J Forensic Med Pathol. 1987;8:42–4.
Cheng TO. Pericardial effusion from self-inserted needle in the heart. Eur Heart J. 1991;12:958.
Teitelbaum SL. Twenty years’ experience with intrinsic tumors of the bony thorax at a large institution. J Thorac Cardiovasc Surg. 1972;63:776.
Acknowledgements
We acknowledge Dr Hiranya Saikia (statistician), Dr B. Hazarika (chest physician, Dr G. Kushre (anatomist), Dr M. Talukdar (cardiothoracic surgeon) of Assam Medical College for guiding us in carrying this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Funding
None.
Rights and permissions
About this article
Cite this article
Boruah, D.K., Prakash, A., Yadav, R.R. et al. The safe zone for blinded sternal interventions based on CT evaluation of midline congenital sternal foramina. Skeletal Radiol 45, 1619–1628 (2016). https://doi.org/10.1007/s00256-016-2473-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-016-2473-9