Abstract
Objective
Operative treatment of an intra-articular distal radius fracture is one of the most common procedures in orthopedic and hand surgery. The intra- and interobserver agreement of common radiographical measurements of these fractures using cone beam computed tomography (CBCT) and plain radiographs were evaluated.
Materials and methods
Thirty-seven patients undergoing open reduction and volar fixation for a distal radius fracture were studied. Two radiologists analyzed the preoperative radiographs and CBCT images. Agreement of the measurements was subjected to intra-class correlation coefficient and the Bland–Altman analyses.
Results
Plain radiographs provided a slightly poorer level of agreement. For fracture diastasis, excellent intraobserver agreement was achieved for radiographs and good or excellent agreement for CBCT, compared to poor interobserver agreement (ICC 0.334) for radiographs and good interobserver agreement (ICC 0.621) for CBCT images. The Bland–Altman analyses indicated a small mean difference between the measurements but rather large variation using both imaging methods, especially in angular measurements.
Conclusions
For most of the measurements, radiographs do well, and may be used in clinical practice. Two different measurements by the same reader or by two different readers can lead to different decisions, and therefore a standardization of the measurements is imperative. More detailed analysis of articular surface needs cross-sectional imaging modalities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Distal radius fracture is one of the most common types of fracture, especially in pediatric patients and in the elderly patient population. In Western countries, a 50-year-old woman has a 15% risk of suffering a Colles’ fracture during her remaining lifetime, whereas the risk is only 2% for a man of the same age [1]. The optimal treatment of distal radius fractures is still controversial. Most fractures can be treated non-surgically with a cast. However, operative treatment of these fractures has increased rapidly over the last few years. For example, the number of operatively treated distal radius fractures in Finland doubled between 1998 and 2008 [2]. The possible reasons for this increase include improved imaging techniques, development of locking compression plates, and better treatment outcomes. Results after plate fixation have been reported significantly better than after external fixation and percutaneous pin fixation, especially among patients with AO group-C2 fractures [3].
The decision of whether to treat the fracture of the distal radius fracture operatively or not most often relies on three radiographical measurements: ulnar variance, volar tilt, and radial inclination. These parameters are also used to better understand the extent of the injury and to predict treatment outcomes. The criteria for acceptable anatomical reduction have become stricter because of the improved technology and the subsequently improved surgical fixation methods. Articular incongruities may lead to early degenerative changes and a common belief is that incongruity of the radiocarpal joint must be corrected. Many questions are still under debate, as the radiological findings in elderly patients do not correlate with the functional outcome [4–6].
Conventional radiographs have an essential role in diagnostic evaluation of distal radius fractures. Computed tomography (CT) is often used, as it is more a sensitive method in identifying and quantifying articular incongruities. Quantification of articular angles and dorsovolar and mediolateral distances are also better identified on CT [7]. A prospective study on 120 distal radius fractures found that the recommended treatment plan changed in 23% of the cases when multidetector computed tomography (MDCT) imaging was combined with conventional radiographs [8]. The authors reported that viewing CT images led to an operative treatment plan more often than after viewing radiographs alone.
Cone beam computed tomography (CBCT) scanning has been shown to be a valuable method for assessing wrist ligaments and radiocarpal cartilage [9]. The use of CBCT in fracture diagnosis is, however, relatively new. High-resolution images [10], easy installation [9], and low radiation doses [11] associated with CBCT are some reasons for its increasing use. In addition, fewer metallic artefacts are observed on CBCT scans postoperatively compared to MRI.
The main aim of the present study was to compare the intra- and interobserver agreement of common radiographical measurements of distal radial fractures on plain radiographs and on CBCT images and to evaluate the role of CBCT in fracture diagnosis.
Materials and methods
The patients included in this study were treated at the department of hand surgery in our hospital. A total of 37 patients (nine males and 28 females, with a mean age of 58 years [range, 30–84 years]) who were undergoing open reduction and volar fixation due to an intra-articular distal radius fracture were enrolled into the study between February and June 2012. The patients were recruited consecutively when the radiological examinations related to this study could be arranged without delaying the fracture treatment. The study protocol was approved by the hospital’s ethics committee. The patients gave their informed consent for the study.
According to the AO fracture classification, all fractures were of type C. None of the patients had had a previous fracture on the distal radius. The main reason for choosing operative treatment was articular incongruity. Fourteen of the 37 patients had been preoperatively treated with closed reduction and cast immobilization.
Standard posteroanterior (PA) and lateral radiographs of the wrist were obtained using direct digital equipment (Philips Digital Diagnost, Best, The Netherlands) at the same time points. The posteroanterior imaging was performed with the shoulder abducted 90° from the trunk and the elbow in a flexion of 90° with the ulna perpendicular to the humerus and the forearm in pronated position. The hand was palm down on the detector [12]. In this way, the wrist was in neutral position. The lateral imaging was performed with the forearm in a neutral position and the elbow in a flexion of 90°.
The patients were examined preoperatively using a novel extremity CBCT scanner (Planmed Verity, Planmed Oy, Helsinki, Finland). The imaging was performed with the patient in a sitting position, the forearm in slight to moderate pronation and the elbow extended or nearly extended [9]. Standard 1.5-mm axial, coronal, and sagittal reformation images were analyzed. Imaging parameters were as follows: field-of-view (FOV) 13 × 16 cm, 90–92 kVp, and 6–10 mA (36–60 mAs).
Two radiologists (denoted R1 and R2), a fourth-year resident, and a specialist with more than 15 years of experience in musculoskeletal (MSK) trauma imaging analyzed the radiographs and the CBCT images. A clinical workstation (Agfa DS3000, IMPAX 5.3, Agfa-Gaevert, Mortsel, Belgium) with two megapixel monitors (Barco Inc., Kortrijk, Belgium) was used for the image analyses. Studies were analyzed twice with an interval of a mean of 5 weeks (range, 2–8 weeks) between each analysis. The patient data were blinded for the observers.
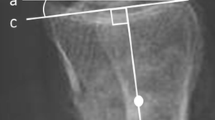
The radiographical parameters analyzed were: radial length (RL), articular step-off (SO), fracture fragment diastasis (FD), radial inclination (RI), volar tilt (VT), teardrop angle (TDA), and anteroposterior distance (APD) [13]. The measurements are shown in Fig. 1. The TDA and ADP are newly characterized radiographical parameters. In this study, the RL was defined as the difference in axial length between the ulnar corner of the distal radius and the most distal extent of the ulnar head on the posteroanterior view. This measurement is also called ulnar variance. The SO is the vertical distance between articular surfaces in articular incongruity and the FD is the maximum separation between fracture fragments. The RI is the angle between a line connecting the radial styloid tip and the ulnar aspect of the distal radius and a line perpendicular to the longitudinal axis of the radius. The VT is measured on the lateral view and it represents the angle between a line along the distal radial articular surface and the line perpendicular to the longitudinal axis of the radius at the joint margin. The TDA is measured as the angle formed by the intersection of a line drawn along the central axis of the radial shaft and a line drawn along the central axis of the teardrop. The teardrop is a U-shaped structure identified on the lateral view that represents the volar rim of the lunate facet. The APD is measured on the lateral view, and determines the distance between the apices of the dorsal and volar rims [13, 14].
We calculated the intraclass correlation coefficients [15, 16] in order to assess the repeatability of the measurements. The intraclass correlation (ICC) assesses the repeatability of measurements by comparing the variability of different measurements of the same radiologist to the total variation of all measurements and the two radiologists. We determined that ICC values of less than 0.40 indicate poor repeatability, ICC values in the range of 0.40 to 0.75 indicate fair to good repeatability, and an ICC value of greater than 0.75 shows excellent repeatability [17, 18]. Intra- and inter-observer variation for each of the measurements was also assessed using the mean difference, with its 95% limits of agreement [19].
Results
Each imaging study was technically successful. The anteroposterior distance, the teardrop angle, and the volar tilt could not be assessed in one case on the radiograph due to imperceptible or indistinct anatomical landmarks. For the same reason, the radial length could not been measured on CBCT in two cases. The articular step-off could not been measured in one case, and the fracture diastasis and the teardrop angle were not measured in two cases on CBCT images.
The mean values of radial length, step-off, fracture diastasis, radial inclination, teardrop angle, anteroposterior distance, and volar tilt of four independent measurements by R1 and R2 are presented in Table 1. The measurements of radial length, step-off, fracture diastasis, and teardrop angle made from CBCT images were shown to be within a greater range than the same measurements made from conventional radiographs.
The ICC analyses for CBCT and plain radiographs are presented in Table 2. For radial length, step-off, radial inclination, teardrop angle, anteroposterior distance, and volar tilt, the intra- and interobserver agreement was good or excellent for both radiographs and CBCT images. For fracture diastasis, excellent intraobserver agreement was achieved for radiographs and good or excellent agreement for CBCT, compared to poor interobserver agreement (ICC 0.334) for radiographs and good interobserver agreement (ICC 0.621) for CBCT images. Interobserver agreement for radiographs was better for radial length, teardrop angle, anteroposterior distance, and volar tilt compared to interobserver agreement for CBCT.
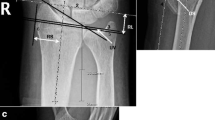
The Bland–Altman analysis (Table 3) shows that although the mean difference is generally small, the variation, however, is rather large. Especially the teardrop angle shows relatively large mean difference and variation in interobserver analysis in both imaging methods. Figure 2 shows a graphical presentation of Bland–Altman analysis of interobserver agreement for radial inclination.
Discussion
The interobserver and intraobserver agreement of common radiographical measurements for intra-articular distal radius fractures were evaluated using the ICC coefficient and Bland–Altman analyses. The ICC method provides quantitative measures of the agreement between the measurements whereas the Bland–Altman analysis provides a qualitative assessment. The Bland–Altman analyses indicated a small mean difference between the measurements but a rather large variation using both imaging methods. Especially in angular measurements a wide range of agreement was seen. This is explained by the comminuted nature of the fractures. In quantitative analyses for CBCT, none of the ICC values were, however, classified as poor agreement.
The measurements used in this study are relevant in managing distal radius fractures. The criteria for an acceptable anatomical reduction of the fracture vary according to the literature [20, 21]. An operation is generally performed when the radial shortening is more than 3 mm, the dorsal tilt is more than 10°, the volar tilt is more than 20°, the radial inclination is less than 15°, or the articular step-off is more than 1 mm. With elderly patients, the criteria tend to be less strict. The decision of whether to operate or is often based on a 1–2 mm or a 5° deviation from the acceptable values. Individual measurements of both intra- and extra-articular parameters may affect the choice of treatment method.
The ICC values showed good intra- and interobserver agreement for radial length, step-off, teardrop angle, anteroposterior distance, radial inclination, and volar tilt for both radiographs and for CBCT images. However, the Bland–Altman analysis showed large variation in intra- and interobserver analysis for angular measurements.
Fracture diastasis is difficult to measure in comminuted fractures with multiple fragments. Computed tomography is most often performed with the intent to evaluate fracture diastasis, as the evaluation of the articular surface is much more precise with CBCT or CT scans than with plain radiographs. We obtained different interobserver results for fracture fragment diastasis on radiographs and CBCT. In ICC analyses, the interobserver agreement for fracture diastasis was poor (ICC 0.344) for radiographs and good (0.621) for CBCT images. There is no consensus on how precisely the articular surface should be restored or which value of fracture diastasis is acceptable. Despite this, viewing CT scans with the intent to evaluate the articular surface often tempts the surgeon to choose surgical procedures ahead of conservative treatment [8].
Measurement of radial length or ulnar variance can be performed using several different methods. In this study, radial length was defined as the difference in axial length between the ulnar corner of the distal radius and the most distal extent of the ulnar head on the posteroanterior view. A study comparing the different measuring methods found that each method of radiographic determination of ulnar variance had considerable disagreement with other methods [22]. Intra- and interobserver reliability was excellent using all methods. Also, different imaging modalities were found to underestimate ulnar variance in a study that compared measurements on plain radiographs, CT, MRI, and anatomic dissection [23]. It has previously been proposed that the ulnar variance could be more reliably measured on lateral radiographs but in comminuted fractures, determination of this measurement is ambiguous.
In addition to the widely used radiographical parameters, this study also included the recently characterized parameters of teardrop angle and anteroposterior distance. By measuring the teardrop angle, the presence of dorsal deformity and articular incongruity in impacted fractures in which there is dissociation of the volar and dorsal parts of the articular surface can be demonstrated. The anteroposterior distance increases in impaction fractures and it can also demonstrate incongruity across the sigmoid notch area. The intra-class correlation values showed good agreement with these measurements in radiographs and CBCT images. This study did not, however, define the relevance of these parameters in fracture treatment. These parameters can be useful in the overall evaluation of the extent of the injury and, together with other measurements, serve to evaluate the extent of the injury and to predict the treatment outcome.
For most of the measurements, radiographs do well and may be used in clinical practice, while more detailed analysis of articular surface needs cross-sectional imaging modalities. A routine use of CBCT, or CT in general, in the treatment of comminuted distal radius fractures may not be justified, and these more advanced imaging methods should be reserved for more complicated cases. On the other hand, CBCT provides logistically an intriguing alternative, since it can be installed in the same room with ordinary radiographic equipment or even in the operating room. For now, CBCT imaging is limitedly available.
Ordinary CT of the wrist and ankle has an effective dose of 30 and 70 μSv, respectively [24]. In a recent study, the effective doses of the ankle joint imaged with CBCT and plain radiographs were compared [25]. They found that ankle imaging performed with the same CBCT scanner used in our study and two standard view radiographs (AP and lateral) resulted in an effective dose of 6 and 1.5 μSv, respectively. To our knowledge, no similar comparative study of wrist imaging has been performed. However, the effective dose is assumed to be of the same magnitude as in ankle examination, i.e., less than 10 μSv. CBCT can thus be regarded as a potential low-dose 3D imaging technique for wrist examination. In the future, this novel approach may replace CT scans in dedicated MSK centers.
Plain radiographs provided a slightly poorer level of agreement when comparing intra- and interobserver agreement for common radiographical measurements of intra-articular fractures of the distal end of the radius. Based on the results of this study, it appears impossible to accurately determine the degree of difference between a 15° and a 20° volar tilt or radial inclination or a 1-mm or a 2-mm step-off in the articular surface. Two different measurements by the same reader or by two different readers can lead to different decisions and therefore a standardization of the measurements is imperative. However, even with standardized measurements, it is difficult to give strict guidelines to clinicians struggling with the decision to operate or not. Our study results support the use of cross-sectional imaging especially in cases with suspicion of fracture fragment diastasis or poor angular measurements in plain radiographs. In conclusion, it would be valuable to have prospective trials studying the relevance of the radiographical measurements and treatment decisions made based on these measurements.
References
Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles’, or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149(11):2445–8.
Mattila VM, Huttunen TT, Sillanpää P, Niemi S, Pihlajamäki H, Kannus P. Significant change in the surgical treatment of distal radius fractures: a nationwide study between 1998 and 2008 in Finland. J Trauma. 2011;71(4):939–43.
Leung F, Tu YK, Chew WY, Chow SP. Comparison of external and percutaneous pin fixation with plate fixation for intra-articular distal radial fractures. A randomized study. J Bone Joint Surg Am. 2008;90(1):16–22.
Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg. 2011;93(23):2146–53.
Diaz-Garcia RJ, Oda T, Shauver MJ, Chung KC. A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. J Hand Surg Am. 2011;36(5):824–35.
Lichtman DM, Bindra RR, Boyer MI, et al. Treatment of distal radius fractures. J Am Acad Orthop Surg. 2010;18(3):180–9.
Haus BM, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults: reexamined as evidence-based and outcomes medicine. J Bone Joint Surg Am. 2009;91(12):2984–91.
Arora S, Grover SB, Batra S, Sharma VK. Comparative evaluation of postreduction intra-articular distal radial fractures by radiographs and multidetector computed tomography. J Bone Joint Surg Am. 2010;92(15):2523–32.
Koskinen SK, Haapamäki VV, Salo J, et al. CT arthrography of the wrist using a novel, mobile, dedicated extremity cone-beam CT (CBCT). Skeletal Radiol. 2013;42(5):649–57.
Carrino JA, Al Muhit A, Zbijewski W, et al. Dedicated cone-beam CT system for extremity imaging. Radiology. 2014;270(3):816–24.
Koivisto J, Kiljunen T, Wolff J, Kortesniemi M. Assessment of effective radiation dose of an extremity CBCT, MSCT and conventional X-ray for knee area using MOSFET dosemeters. Radiat Prot Dosimetry. 2013;157(4):515–24.
Hardy DC, Totty WG, Reinus WR, Gilula LA. Posteroanterior wrist radiography: importance of arm positioning. J Hand Surg Am. 1987;12(4):504–8.
Medoff RJ. Essential radiographic evaluation for distal radius fractures. Hand Clin. 2005;21(3):279–88.
Wald S, Woerter K. Measurements and classifications in musculoskeletal radiology. Stuttgart, Germany: George Thieme Verlag; 2014. p. 108–23.
Muller R, Buttner P. A critical discussion of intraclass correlation coefficients. Stat Med. 1994;13(23–24):2465–76.
Reilingh ML, Beimers L, Tuijthof GJM, Stufkens SAS, Maas M, van Dijk N. Measuring hindfoot alignment radiographically: the long axial view is more reliable than the hindfoot alignment view. Skeletal Radiol. 2010;39(11):1103–8.
Rosner B. Fundamentals of biostatistics. Belmont: CA. Duxbury Press; 2005.
Sampat MP, Whitman GJ, Stephens TW, et al. The reliability of measuring physical characteristics of speculated masses on mammography. Brit J Radiol. 2006;79:S134–40.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10.
Ilyas AM, Jupiter JB. Distal radius fractures—classification of treatment and indications for surgery. Hand Clin. 2010;26(1):37–42.
Ng CY, McQueen MM. What are the radiological predictors of functional outcome following fractures of the distal radius? J Bone Joint Surg Br. 2011;93(2):145–50.
Parker AS, Nguyen M, Minard CG, Guffey D, Willis MH, Reichel LM. Measurement of ulnar variance from the lateral radiograph: a comparison of techniques. J Hand Surg Am. 2014;39(6):1114–21.
Laino DK, Petchprapa CN, Lee SK. Ulnar variance: correlation of plain radiographs, computed tomography, and magnetic resonance imaging with anatomic dissection. J Hand Surg Am. 2012;37(1):90–7.
Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009;91(8):1882–9.
Koivisto J, Kiljunen T, Kadesjö N, Shi X-Q, Wolff J. Effective radiation dose of a MSCT, two CBCT and one conventional radiography device in the ankle region. J Foot Ankle Res 2015;8, doi: 10.1186/s13047-015-0067-8 eCollection
Conflict of interest
The authors declare that they gave no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suojärvi, N., Sillat, T., Lindfors, N. et al. Radiographical measurements for distal intra-articular fractures of the radius using plain radiographs and cone beam computed tomography images. Skeletal Radiol 44, 1769–1775 (2015). https://doi.org/10.1007/s00256-015-2231-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2231-4