Abstract
Purpose
Determine the sensitivity, specificity and accuracy of unenhanced and enhanced MRI in diagnosing scaphoid proximal pole (PP) avascular necrosis (AVN) and correlate whether MRI can help guide the selection of a vascularized or nonvascularized bone graft.
Methods
The study was approved by the IRB. Two MSK radiologists independently performed a retrospective review of unenhanced and enhanced MRIs from 18 patients (16 males, 2 females; median age, 17.5 years) with scaphoid nonunions and surgery performed within 65 days of the MRI. AVN was diagnosed on the unenhanced MRI when a diffusely decreased T1-W signal was present in the PP and on the enhanced MRI when PP enhancement was less than distal pole enhancement. Surgical absence of PP bleeding was diagnostic of PP AVN. Postoperative osseous union (OU) was assessed with computed tomography and/or radiographs.
Results
Sensitivity, specificity and accuracy for PP AVN were 71, 82 and 78 % for unenhanced and 43, 82 and 67 % for enhanced MRI. Patients with PP AVN on unenhanced MRI had 86 % (6/7) OU; 100 % (5/5) OU with vascularized bone grafts and 50 % (1/2) OU with nonvascularized grafts. Patients with PP AVN on enhanced MRI had 80 % (4/5) OU; 100 % (3/3) OU with vascularized bone grafts and 50 % (1/2) OU with nonvascularized grafts. Patients with viable PP on unenhanced and enhanced MRI had 91 % (10/11) and 92 % (12/13) OU, respectively, all but one with nonvascularized graft.
Conclusions
When PP AVN is evident on MRI, OU is best achieved with vascularized grafts. If PP AVN is absent, OU is successful with nonvascularized grafts.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Late complications of scaphoid fractures include osteoarthritis, malunion and nonunion. Approximately 10 % of scaphoid fractures fail to unite, which may result in chronic pain, instability and disability [1–4]. While several risk factors are associated with a higher likelihood of nonunion, avascularity of the proximal pole is considered a major determinant. As a result, accurate preoperative assessment of proximal pole vascularity is critical, often determining whether or not a vascularized bone graft is employed [5]. Although conventional radiography, bone scintigraphy, computed tomography (CT) and magnetic resonance imaging (MRI) have all been utilized in the evaluation of scaphoid fractures, most investigators consider MRI the most beneficial for assessing proximal pole vascularity.
The effectiveness of unenhanced MRI in evaluating avascular necrosis (AVN) of the proximal pole has been inconclusive in prior studies. Some authors have demonstrated a strong correlation with the vascular status at surgery [6–10]; however, others have concluded the opposite [11]. Disparate conclusions have also been reported regarding the usefulness of gadolinium-enhanced MRI to evaluate proximal pole vascularity, even when dynamic imaging was used [11–13]. The issue is further complicated by a report describing the “apparent increased contrast pattern” in 6 of 13 patients with surgically proven avascular proximal poles [14]. To our knowledge, only four articles have attempted to correlate surgical outcome and the preoperative MRI findings, two analyzing nonvascularized bone grafts, one analyzing vascularized bone grafts, and one analyzing both vascularized and nonvascularized grafts, [11, 12, 15, 16].
Therefore, we sought to determine the sensitivity, specificity and accuracy of unenhanced and enhanced MRI in diagnosing AVN and whether the MR findings can help guide the selection of a vascularized or nonvascularized bone graft.
Materials and methods
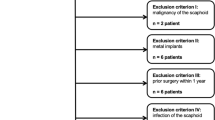
This study was approved by our Institutional Review Board, which waived the requirement for informed consent. Following IRB approval, a retrospective database search identified 18 patients who had undergone the surgical repair of a chronic scaphoid fracture nonunion utilizing either a vascularized or nonvascularized bone graft between 2006 and 2011. Using the clinical history provided by the 18 patients as documented in the electronic medical record, the mean time between injury and surgery was approximately 11 months (range ∼5 months to 24 months); however, in some patients the exact date of injury was estimated by the patient. All patients had preoperative enhanced MRI performed on a 1.5-T system (Siemens Symphony, Espree or Avanto, Erlangen, Germany) with a 120 mm field of view using a dedicated four-channel wrist coil. All patients received 0.2 mmol/kg of gadopentetate dimeglumine (Magnevist, Bayer Healthcare Pharmaceuticals, Berlin, Germany) intravenously with the enhanced scanning beginning within 5 min after the injection. Intraoperative assessment of the proximal pole vascular status was performed within 65 days (median 27 days, range 1–65 days) of the MRI examination. Coronal precontrast T1-weighted (T1-W) and postcontrast fat-suppressed (FS) T1-W sequences (512 × 220 matrix) were retrospectively evaluated by MSK radiologists with 1 and 10 years of experience independently; both radiologists were blinded to the surgical findings.
Avascular necrosis (AVN) of the proximal pole of the scaphoid was diagnosed on the enhanced T1-W FS images when the T1wFS signal intensity (enhancement) in the proximal pole was qualitatively less than the signal (enhancement) in the distal pole. Avascular necrosis was diagnosed on the T1-W precontrast sequence if the signal in the proximal pole was diffusely less than or equal to that of the skeletal muscle [10] (Fig. 1a–b). The imaging appearance within 1 mm of the fracture margin was not considered when evaluating the vascular status as the appearance of this area is often heterogeneous with respect to signal or enhancement. The proximal pole was considered viable unless the proximal pole met the above criteria (Fig. 2a–c). Disagreements regarding the MRI signal or enhancement were resolved by consensus.
a–b A 17-year-old male with avascular necrosis at surgery performed 9 days post-MRI. a Unenhanced T1-weighted (T1-W) coronal image (TR/TE 959/22) demonstrates diffusely decreased T1-W signal in the proximal pole (*) meeting the criteria for AVN. b Postcontrast T1-W coronal image (TR/TE 686/23) demonstrates lack of enhancement in the proximal pole (*) meeting the criteria for AVN. (Note enhancing synovial tissue (arrow)
a–c A 15-year-old female with a viable proximal pole at surgery. a T1-weighted (TR/TE 604/15) coronal image demonstrates heterogeneous proximal pole signal with areas of fat signal remaining (arrow) meeting the criteria for viability. b Postcontrast fat-suppressed T1-W (TR/TE; 500/12) coronal image demonstrates signal intensity in the proximal pole (*) equal to that in the distal pole, consistent with viability. c Precontrast fat suppressed T1-W (TR/TE; 500/12) coronal image for comparison
The final determination of proximal pole viability was the presence of any punctate bleeding at surgery during (1) the debridement of the fracture, (2) curetting of sclerotic bone or (3) the creation of a groove for the bone graft. Avascular necrosis was diagnosed if no bleeding was apparent in the proximal pole during surgery. The sensitivity, specificity and accuracy of unenhanced and enhanced MRI were then calculated. Weighted kappa statistics were calculated to determine the interreader correlation.
Eight patients received vascularized pedicle bone grafts from the 1, 2 intercompartmental supraretinacular artery, and ten patients were treated with conventional autogeneous bone grafting. Patients were assessed for osseous union at least 4 months postoperatively or until union was identified using either computed tomography (CT) (n = 14 patients; median time post-surgery 96 days, range 56–209) and/or radiographs (n = 16 patients; median time post-surgery 149 days, range 95–320). Radiographs were the sole source of postsurgical evaluation for osseous union in four patients (median time postsurgery 105 days, range 95–129). The postoperative CT and radiographs were evaluated by the more senior MSK radiologist blinded to the MRI reports and the operative findings. Osseous union was considered present if at least 25 % of the fracture demonstrated bone bridging, including osseous bridging of the vascularized graft if present (Fig. 3a–b).
a–b A 20-year-old male with scaphoid fracture nonunion and AVN diagnosed on both MRI and at surgery performed 29 days post-MRI. a Preoperative radiograph demonstrating fracture at the junction of the proximal and middle aspects of the scaphoid (arrow). b CT obtained 96 days postsurgery demonstrates near complete osseous union (arrows)
Results
Eighteen patients met the entry criteria (16 male, 2 female; 9 right, 9 left). The median patient age was 17.5 years (range 14–39 years), 17 years for patients with a viable proximal pole and 19 years for patients with AVN. Sixty-one percent (11/18) of the fractures were located in the mid to distal 2/3 of the scaphoid with 39 % (7/18) located in the proximal pole or at the junction of the proximal and middle thirds. The median interval from MRI to surgery was 27 days (range 1 to 65), 26 days (range 9–38) for those with AVN and 30 days (range 1–65) for those without AVN. At surgery, 39 % (7/18) of the proximal poles did not demonstrate any punctate bleeding and were diagnosed with AVN, with AVN present surgically in 57 % (4/7) of the more proximal fractures and in 27 % (3/11) of the mid to distal fractures (Table 1).
The interreader agreement was 88 % overall with an overall kappa statistic of 0.75 (95 % CI 0.53–0.97), kappa = 0.73 (95 % CI 0.38–1.0) for enhanced MRI and kappa = 0.77 (95 % CI 0.48–1.0) for unenhanced MRI. In the four cases in which there was disagreement, a consensus interpretation was rendered with the independent interpretation for each radiologist utilized as the consensus interpretation in two cases each.
Using the consensus interpretation, enhanced MRI resulted in nine true-negative (TN), four false-negative (FN), three true-positive (TP) and two false-positive (FP) diagnoses for a sensitivity, specificity and accuracy of 43, 82 and 67 % in predicting AVN, respectively. Unenhanced MRI resulted in nine TN, two FN, five TP and two FP diagnoses for a sensitivity, specificity and accuracy of 71, 82 and 78 % in diagnosing AVN, respectively (Fig. 4a–c) (Table 1).
a–d A 16-year-old male with proximal pole avascular necrosis (AVN) at surgery. a Unenhanced T1-weighted (TR/TE 551/14) coronal image demonstrates diffusely decreased T1-w signal intensity in the proximal pole (*) meeting the criteria for AVN. b Pre- (TR/TE 762/14) and c postcontrast T1-weighted fat-suppressed (TR/TE 464/14) coronal images demonstrate signal intensity in the proximal pole equal to the signal in the distal pole (arrow), incorrectly diagnosing proximal pole viability (false negative). d Radiograph obtained 26 months postsurgery demonstrates complete osseous union (arrows)
All patients diagnosed with AVN at surgery received vascularized pedicle bone grafts from the 1, 2 intercompartmental supraretinacular artery, with five meeting and two not meeting the criteria for proximal pole AVN on the noncontrast MRI and three meeting and four not meeting the criteria for proximal pole AVN on the contrast-enhanced MRI. In addition, one patient who had evidence of proximal pole viability at both MRI and surgery also received a vascularized graft. The surgeon’s decision to use a vascularized bone graft in this patient, which varies from the typical treatment, was based on “his clinical judgment” given her young age (15) and the minimal bleeding of the proximal pole at surgery. Ten patients had punctate bleeding at surgery and received conventional autogeneous nonvascularized bone grafting, eight meeting the criteria for proximal pole viability and two meeting the criteria for AVN on both the noncontrast and contrast-enhanced MRIs (Table 1).
Of the seven patients with scaphoid proximal pole AVN at surgery who received a 1, 2 supraretinacular vascularized bone graft; 86 % (6/7) did and 14 % (1/7) did not demonstrate osseous union (Fig. 4d). The patient who received a vascularized bone graft even though the MRI and surgical findings were consistent with a viable proximal pole had osseous union. All eight patients with viable proximal poles at both MRI and surgery who received nonvascularized bone grafts had osseous union. Of the two patients with punctate bleeding at surgery but evidence of proximal pole AVN on MRI who received nonvascularized bone grafts, one did and one did not demonstrate osseous union (median, 122 days; range, 113–130 days) (Fig. 5a–d) (Table 1). Of note, longer postsurgical radiographic follow-up (median 177 days; range 130–223 days) was obtained for the two patients that did not demonstrate osseous union.
a–d A 23-year-old male with mid-pole scaphoid fracture and punctate bleeding at surgery. a Unenhanced T1-W (TR/TE 483/15) image demonstrates diffusely decreased T1w signal within the proximal pole (*) consistent with AVN. b Postcontrast T1-W fat suppressed MR image (TR/TE 713/14) demonstrates decreased proximal pole enhancement (*) compared to the distal pole meeting the criteria for AVN. c Reformatted oblique coronal CT image obtained 96 days postsurgery demonstrates persistent fracture line (arrow) with little if any osseous union. d Subsequent 'radiograph obtained 130 days postsurgery also demonstrates a persistent fracture line (arrow) without appreciable osseous union
Discussion
The use of MRI to evaluate AVN in scaphoid fracture nonunions has been advocated since the early 1990s [6, 8, 17]. More recently, attention has shifted to gadolinium-enhanced MRI to evaluate the viability of the proximal pole of the scaphoid. However, there have been surprisingly few controlled studies addressing this in the literature. Furthermore, there is disagreement in these studies regarding the sensitivity, specificity and accuracy of gadolinium-enhanced MRI in predicting the vascular status of the proximal pole. We compared contrast-enhanced to unenhanced T1-W MR images for diagnosing AVN in the proximal pole of the scaphoid to determine whether MRI is useful in guiding the use of a vascularized or nonvascularized bone graft.
We found unenhanced T1-W MRI more sensitive and accurate in predicting AVN than contrast-enhanced MRI primarily as a result of two false-negative cases for AVN in the enhanced group. Our findings are similar to two prior reports that evaluated the sensitivity and accuracy of contrast-enhanced images in detecting AVN in the proximal pole, but differ from a third [11, 12, 14]. Cerezal et al. compared precontrast T1-W images without fat suppression to postcontrast T1-W images with fat suppression in 30 patients with scaphoid fracture nonunion. Using a classification system based on the percentage of enhancement in the proximal pole of the scaphoid to determine viability, Cerezal et al. reported that contrast-enhanced MRI was 86 % sensitive, 96 % specific and 93 % accurate in diagnosing AVN [11]. Singh et al., using fat-suppressed postcontrast T1-W images and criteria for AVN similar to that of Cerezal, examined 16 patients with scaphoid fracture nonunion and found a sensitivity of 25 %, specificity of 100 % and accuracy of 73 % in diagnosing AVN [12], findings that are similar to ours. Anderson et al. evaluated 13 surgically proven cases of proximal pole AVN with contrast-enhanced MRI before and after vascularized bone grafting. Like Cerezal, they compared non-fat-suppressed precontrast T1-W images with fat-suppressed postcontrast T1-W images and found that 46 % (6/13) of their surgically proven AVN proximal poles exhibited increased bone marrow signal following contrast enhancement relative to the other carpal bones, three even demonstrating markedly increased signal [14]. This mirrors our experience of 57 % (4/7) of the proximal poles with surgically proven AVN demonstrating increased signal intensity relative to the distal scaphoid following contrast administration. We agree with Anderson et al. that the cause of nonviable bone having increased signal following contrast enhancement is unknown [14]. Proposed mechanisms for this apparent enhancement include diffusion of contrast material [18] and the in-growth of fibrous mesenchymal tissue into the proximal pole [19].
The discrepancy in identifying AVN in the proximal pole of the scaphoid in these published results may be partially explained by how “enhancement” is interpreted, a process complicated by several factors. In many cases, MRI signal within the proximal pole is heterogeneous, with central signal intensity differing from signal intensity along the fracture margin, possibly skewing qualitative assessment. As a result, we did not include the 1–2 mm of bone along the fracture margin in our imaging assessment. Additionally, depending on slice thickness, partial volume averaging with adjacent hyperemic soft tissue may also result in perceived “enhancement.” Routine contrast-enhanced MRI of the wrist is usually performed with a delay prior to image acquisition, which may result in contrast diffusing into the proximal pole, possibly incorrectly suggesting viability when AVN is present [18]. However, Donati et al. reported that dynamic contrast-enhanced MRI performed no better than delayed contrast MRI in the assessment of proximal pole AVN in the setting of chronic fracture nonunions with the two reviewers in their study having a sensitivity and accuracy of 54–62 % and 75–78 % for detecting AVN, respectively [13]. The lack of increased accuracy for predicting AVN using dynamic contrast enhancement may be partially explained by the fat content of bone marrow as some investigators have noted that even normal marrow may not appear to enhance, fatty marrow enhancing less than cellular marrow [20, 21].
To our knowledge, only four studies have evaluated whether preoperative MRI can help predict the surgical outcome following treatment for scaphoid fracture nonunion, two studies evaluating contrast-enhanced preoperative MRI and autologous bone graft fusion, one study evaluating preoperative contrast-enhanced MRI and vascularized bone graft placement and one study evaluating both preoperative unenhanced and enhanced MRI using both vascularized and nonvascularized bone grafts [11, 12, 15, 16].
The two studies using autologous “nonvascularized” bone grafts disagreed about whether contrast-enhanced preoperative MRI findings could predict a successful surgical outcome [11, 12]. Using postoperative radiographs to diagnose osseous union, Cerezal et al. reported that the overall rate of osseous union was 74 % (20/27). They also found that the preoperative degree of enhancement correlated with the rate of osseous union, with 87 % (20/23) of the proximal poles with >20 % enhancement demonstrating osseous union and 0 % (0/4) of the proximal poles with <20 % enhancement demonstrating osseous union [11]. Singh et al. reported an overall osseous union rate of 75 % (12/16), similar to Cerezal et al. However, Singh et al. did not find an association between the degree of proximal pole enhancement and osseous union with 64 % (9/14) of the proximal poles with >25 % enhancement demonstrating osseous union and 100 % (2/2) of the proximal poles with <25 % enhancement demonstrating osseous union [12]. Dailiana et al. evaluated the use of postoperative contrast-enhanced MRIs to access osseous union following the placement of vascularized bone grafts for scaphoid fracture nonunion [16]. However, only 53 % (8/15) of the patients received preoperative contrast-enhanced MRIs with all eight patients exhibiting proximal pole bleeding at surgery; osseous union occurred in 93 % (14/15) of patients at 3-month follow-up [16].
To our knowledge, only Ciprian et al. have correlated the MRI appearance to the rate of postoperative osseous union using both vascularized and conventional bone grafts. They evaluated 21 patients with scaphoid fracture nonunions, 7 patients receiving vascularized bone grafts and 14 conventional bone grafts [15]. Ciprian et al. reported that vascularized grafts had a higher rate of union compared to nonvascularized grafts when decreased T1-W signal (83 to 57 %) or lack of enhancement (80 to 50 %) in the proximal pole was present on the MRI; however, they did not report the number of patients with AVN at the time of surgery [15]. We similarly found a higher rate of osseous union when vascularized grafts were used compared to nonvascularized grafts when either decreased T1-W signal (100 to 50 %) or a lack of enhancement (100 to 50 %) was present.
Limitations of our study included the retrospective nature and sample size of 18 patients (7 with AVN). We share these limitations with Cerezal (27 patients; 4 with AVN), Singh (16 patients; 2 with AVN), Ciprian (21 patients; unknown number with AVN) and Dailiana (8 patients; 0 with AVN) [11, 12, 15, 16]. To our knowledge, our sample size of seven patients with preoperative MRI, AVN diagnosed at surgery and postoperative follow-up is the largest study in the literature. Therefore, our findings could form the basis for a larger prospective study in order to corroborate our results. Our surgeons were also not blinded to the MRI findings. This was impractical because they utilized the results to counsel their patients and to plan the surgery. The use of bleeding at surgery as the “gold standard” is the method commonly used in the surgical community. However, there is potential for sampling bias, and some proximal poles considered necrotic at surgery might have had viable areas that were not sampled. The criteria utilized to determine avascular necrosis on both the unenhanced and enhanced images may also account for some of the differences found in the previous reports. It is inherently subjective when determining whether the signal on the unenhanced images is diffusely decreased, equal to or less than that of skeletal muscle or whether the signal on the enhanced images is equal to or greater than the distal pole. Even so, using these criteria, there was overall good interreader agreement.
In conclusion, unenhanced MRI was slightly more accurate than contrast-enhanced MRI in diagnosing scaphoid proximal pole AVN. More importantly, our findings suggest that relying solely on the vascular status of the proximal pole at surgery may not identify all of the patients who might benefit from a vascularized pedicle graft. As a result, use of a vascularized bone graft should be considered when the preoperative MRI is suspicious for AVN even if punctate bleeding is present at surgery.
References
Barton NJ. The late consequences of scaphoid fractures. J Bone Joint Surg (Br). 2004;86-B:626–30.
Adams JE, Steinmann SP. Acute scaphoid fractures. Orthop Clin N Am. 2007;38:229–35.
Morgan WJ, Breen TF, Coumas JM, Schulz LA. Role of magnetic resonance imaging in assessing factors affecting healing in scaphoid nonunions. Clin Orthop Relat Res. 1997;336:240–6.
Ciprian S, Iochum S, Kohlmann R, Dautel G, Dap F, Blum A. MR imaging accuracy in the prediction of bone graft healing potential in scaphoid non-union. J Radiol. 2004;85:1699–706.
Gunal I, Ozcelik A, Gukturk E, Ada S, Demirtas M. Correlation of magnetic resonance imaging and intraoperative punctate bleeding to assess the vascularity of scaphoid nonunion. Arch Orthop Trauma Surg. 1999;119:285–7.
Perlik PC, Guilford WB. Magnetic resonance imaging to assess vascularity of scaphoid nonunions. J Hand Surg [Am]. 1991;16A(3):479–84.
Sakuma M, Nakamura R, Imaeda T. Analysis of proximal fragment sclerosis and surgical outcome of scaphoid non-union by magnetic resonance imaging. J Hand Surg (Br). 1995;20B(2):201–5.
Trumble TE. Avascular necrosis after scaphoid fracture: a correlation of magnetic resonance imaging and histology. J Hand Surg [Am]. 1990;15A(4):557–64.
Desser TS, McCarthy S, Trumble TE. Scaphoid fractures and Kienbock’s disease of the lunate: MR imaging with histopathologic correlation. Magn Reson Imaging. 1990;8:357–61.
Fox MG, Gaskin CM, Chhabra AB, Anderson MW. Assessment of scaphoid viability with MRI: a reassessment of findings on unenhanced MR images. Am J Roentgenol. 2010;195:W281–6.
Cerezal L, Abascal F, Canga A, Garcia-Valtuille R, Bustamante M, del Pinal F. Usefulness of gadolinium enhanced MR imaging in the evaluation of the vascularity of scaphoid nonunions. Am J Roentgenol. 2000;174:141–9.
Singh AK, Davis TRC, Dawson JS, Oni JA, Downing ND. Gadolinium enhanced MR assessment of proximal fragment vascularity in nonunions after scaphoid fracture: does it predict the outcome of reconstructive surgery? J Hand Surg (Br). 2004;29B(5):444–8.
Donati OF, Zanetti M, Nagy L, Bode B, Schweizer A, Pfirrmann CWA. Is dynamic gadolinium enhancement needed in MR imaging for the preoperative assessment of scaphoidal viability in patients with scaphoid nonunion? Radiology. 2011;260(3):808–16.
Anderson SE, Steinbach LS, Tschering-Vogel D, Martin M, Nagy L. MR imaging of avascular scaphoid nonunion before and after vascularized bone grafting. Skelet Radiol. 2005;34:314–20.
Ciprian S, Iochum S, Kohlmann R, Dautel G, Dap F, Blum A. MR imaging accuracy in the prediction of bone graft healing potential in scaphoid non-union. J Radiol. 2004;85(10 Pt 1):1699–706. French.
Dailiana ZH, Zachos V, Varitimidis S, Papanagiotou P, Karantanas A, Malizos KN. Scaphoid nonunions treated with vascularised bone grafts: MRI assessment. Eur J Radiol. 2004;50(3):217–24.
Imaeda T, Nakamura R, Miura T, Makino N. Magnetic resonance imaging in scaphoid fractures. J Hand Surg (Br). 1992;17-B:20–7.
Sebag G, Ducou Le Pointe H, Klein I, et al. Dynamic gadolinium-enhanced subtraction MR imaging: a simple technique for the early diagnosis of Legg-Calvé-Perthes disease: preliminary results. Pediatr Radiol. 1997;27(3):216–20.
Sakai T, Sugano N, Nishii T, Haraguchi K, Ochi T, Ohzono K. MR findings of necrotic lesions and the extralesional area of osteonecrosis of the femoral head. Skelet Radiol. 2000;29(3):133–41.
Dawson JS, Martel AL, Davis TRC. Scaphoid blood flow and acute fracture healing. A dynamic MRI study with enhancement with gadolinium. J Bone Joint Surg (Br). 2001;83-B:809–14.
Verstraete KL, De Deene Y, Roels H, Dierick A, Uyttendaele D, Kunnen M. Benign and malignant musculoskeletal lesions: dynamic contrast-enhanced MR imaging—parametric “first-pass” images depict tissue vascularization and perfusion. Radiology. 1994;192(3):835–43.
Conflict of interest
The authors declare that they have no conflict of interest, grants or financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fox, M.G., Wang, D.T. & Chhabra, A.B. Accuracy of enhanced and unenhanced MRI in diagnosing scaphoid proximal pole avascular necrosis and predicting surgical outcome. Skeletal Radiol 44, 1671–1678 (2015). https://doi.org/10.1007/s00256-015-2221-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2221-6