Abstract
Objective
To compare the diagnostic value of cone-beam computed tomography (CBCT) and conventional radiography (CR) after acute small bone or joint trauma.
Materials and methods
Between March 2013 and January 2014, 231 patients with recent small bone or joint trauma underwent CR and subsequent CBCT. CR and CBCT examinations were independently assessed by two readers, blinded to the result of the other modality. The total number of fractures as well as the number of complex fractures were compared, and inter- and intraobserver agreement for CBCT was calculated. In addition, radiation doses and evaluation times for both modalities were noted and statistically compared.
Results
Fracture detection on CBCT increased by 35 % and 37 % for reader 1 and reader 2, respectively, and identification of complex fractures increased by 236 % and 185 %. Interobserver agreement for CBCT was almost perfect, as was intraobserver agreement for reader 1. The intraobserver agreement for reader 2 was substantial. Radiation doses and evaluation time were significantly higher for CBCT.
Conclusion
CBCT detects significantly more small bone and joint fractures, in particular complex fractures, than CR. In the majority of cases, the clinical implication of the additionally detected fractures is limited, but in some patients (e.g., fracture-dislocations), the management is significantly influenced by these findings. As the radiation dose for CBCT substantially exceeds that of CR, we suggest adhering to CR as the first-line examination after small bone and joint trauma and keeping CBCT for patients with clinical-radiographic discordance or suspected complex fractures in need of further (preoperative) assessment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cone-beam computed tomography (CBCT) was first introduced in the early 1980s as a new technique intended for head and neck imaging [1, 2]. Nowadays, it is not only one of the most important modalities for dental imaging, but also has numerous applications in the field of maxillofacial, middle ear and musculoskeletal imaging and is used in vertebroplasty and in the guidance of other interventional procedures [3–11].
Unlike ‘conventional’ multidetector CT (MDCT), where a fan-shaped beam moves helically around the patient and falls on a linear detector (Fig. 1a), CBCT uses a cone-shaped beam and a flat panel detector (Fig. 1b). This allows acquisition of the entire scan volume in only one rotation, resulting in a lower radiation dose than MDCT. Other advantages of CBCT include higher spatial resolution, reduction of metal artifacts (e.g., dental implants, osteosynthesis material) and the relatively low cost of the equipment [8, 12–16].
Schematic drawing of the differences between multidetector computed tomography (MDCT) and cone-beam computed tomography (CBCT). In MDCT (a), a thin, linear-shaped radiation beam falls on a thin, curved detector. To scan a certain volume, both the XR tube and detector must make multiple rotations around the patient. In CBCT (b), the cone-shaped beam allows the same volume in only one rotation
This, however, comes at the cost of a loss of contrast resolution (decreased soft tissue visualization), an increase in scan time (increased susceptibility to motion artifacts) and limited scan volume/surface (limited to the size of the flat panel detector) [17].
Imaging studies on small bone or joint trauma typically consist of a series of conventional radiographs. Conventional radiography (CR) has proven to be inferior compared to MDCT in fracture detection [18, 19], but the high radiation dose of MDCT limits its systematic use. CBCT combines a high spatial resolution and low radiation dose (compared to MDCT) and is therefore a performant modality for imaging of small osseous structures such as temporal bones or peripheral joints, which has been previously demonstrated [3–9]. However, to the best of our knowledge, there has not been a study yet directly comparing CBCT and CR in the detection of small bone and joint trauma.
Materials and methods
This study was approved by our hospital’s ethical review board, and written informed consent was obtained from all patients [or their parent(s) in case of minor patients].
Inclusion criteria and patient population
Patient inclusion criteria were: age 6 years or older and recent (<1 week old) trauma of a small bone or joint (finger, hand, wrist, elbow, toe, foot, ankle or knee). Patients who were considered to be unable to remain perfectly immobile during the CBCT examination were excluded (mostly young children and elderly patients with tremor). Based on these criteria, we included 231 patients (110 females, 121 males, mean age 32 ± 14.2 years old) during the study period from March 2013 to January 2014. In this period, 15 patients were excluded (14 patients aged under 6 and 1 elderly patient with severe essential tremor).
Imaging protocols
All patients first underwent conventional radiography of the affected bone or joint, immediately followed by CBCT. The conventional radiographic examination consisted of 2–6 radiographs depending on the examined area, e.g., only one anteroposterior (AP) and one oblique view of the hand compared to one posteroanterior, one lateral, two oblique and two dedicated scaphoid views of the wrist.
Conventional radiography was performed on the AXIOM Luminos dRF (Siemens, Erlangen, Germany) consisting of an X-ray tube (Optitop 150/40/80 HC-100; focal spot size, 0.6 mm), a high-voltage generator (Polydoros F65) and an amorphous silicon image detector (43 × 43-cm sensing surface, 2,840 × 2,880 matrix, 148-μm pixel size).
CBCT imaging was performed on a Newtom 5G-system (QR, Verona, Italy), equipped with a high frequency, rotating anode and silicone flat detector. Anode voltage was 110 kV; anode current varied between 1 and 20 mA depending on the examined bone or joint. An 8 × 8-cm field of view was used, centered on the most painful region. In 30 s, the gantry performed a 360° movement during which projection images were acquired. Subsequently, these were reconstructed to axial slices (thickness 0.2 mm) as well as sagittal and coronal reconstructions (thickness 1 mm; reconstruction time 60 s).
All images were sent by DICOM communication to a PACS system (Impax, AGFA Healthcare, Mortsel, Belgium).
Image analysis
All images were independently evaluated by two radiologists (2 and 25 years of experience). A first evaluation of both the conventional radiographs and cone-beam images (in random order but blinded to the result of the other examination) was performed immediately after both examinations. A second reading of both examinations was performed 6 weeks later.
The following parameters were scored: (1) presence of fractures and fracture complexity: simple/complex (complex: either intraarticular extension or comminuted fractures, consisting of multiple fragments), (2) radiation dose (dose area product, DAP) and (3) evaluation time.
Statistical analysis
Statistical analysis was performed with SPSS statistical software (IBM SPSS Statistics for Windows, version 22.0; Armonk, NY: IBM Corp.). For both readers, fracture detection on CR and CBCT was compared using the McNemar test. Wilcoxon paired rank-test was applied to compare radiation dose and interpretation time. Inter- and intraobserver agreement was calculated using weighted kappa tests. Statistical significance was considered if p < 0.05.
Results
Fracture detection-fracture complexity
Results of fracture detection on CR and CBCT are summarized in Table 1. Reader 1 (R1) identified 35 % more fractures on CBCT than CR (109 vs. 81, p < 0.001), reader 2 (R2) 37 % (107 versus 78, p < 0.001) (Figs. 2 and 3). R1 and R2 detected respectively 11 and 14 complex fractures on CR compared to 37 and 40 complex fractures on CBCT (Figs. 4, 5 and 6). This corresponds to an increase of 236 % (p <0.001) and 185 % (p <0.001), respectively. All of the complex fractures detected on CR were identified on CBCT; the complex fractures that were additionally found on CBCT were initially classified as simple fractures.
A 16-year-old male after a fall on an outstretched hand and lateral wrist pain. The conventional radiographs of the wrist (a, b) show obliteration of the scaphoid fat pad (arrowhead), but cannot reveal an underlying fracture. On CBCT (c,d); both interruption of the cortex and a radiolucent line are delineated (arrows), indicating a non-displaced fracture through the distal pole of the scaphoid
A 14-year-old female after eversion trauma of the ankle with persistent pain and soft tissue swelling around the lateral malleolus. The conventional radiograph (a) shows no osseous lesions. On the coronal (b) and axial (c) CBCT reconstructions, a small avulsion fracture of the distal fibula is noted (arrows)
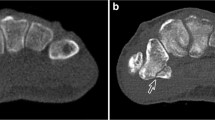
A 41-year-old male after a fall from a ladder, presenting with wrist pain and deformity. Both the conventional radiographs (a, b) and CBCT (c, d) show a dislocation of the lunate (white asterisk) and capitate (black asterisk) bones, but only the CBCT reveals the additional fracture of the distal radius with multiple fracture fragments (arrow in d)
A 25-year-old male after crush trauma of the right foot with persistent pain at the base of metatarsal I and II. Conventional radiographs (a, b) cannot demonstrate any osseous lesions, but CBCT (c, d) clearly demonstrates a fracture (arrows) through the base of metatarsal II with intraarticular extension (Lisfranc fracture)
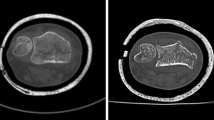
A 57-year-old male after a fall from stairs on his left elbow. Both the conventional radiographs (a, b) and CBCT reconstructions (c) reveal a nondisplaced fracture of the radial head (arrows) with obliteration of the adjacent fat pads. There is however an additional avulsion fracture with an intraarticular fragment, which is only noted on CBCT (arrowhead in d). Therefore, the patient was treated surgically (removal of the loose fragment) instead of conservatively
The interobserver agreement for CBCT was 0.938 (almost perfect). The intraobserver agreement for R1 was 0.93 (almost perfect) and for R2 0.81 (very good).
Radiation dose
Radiation doses of CBCT were significantly higher in all examined bones and joints except the knee (Table 2). This difference was the largest in the smaller bones/joints (fingers and toes) and decreased when bone or joint size increased.
Examination time
The average time necessary to interpret a conventional radiographic examination (2–6 radiographs) ranged between 15 and 34 s, depending on the examined bone/joint. This was significantly higher (51 to 83 s) for the CBCT examinations (Table 3).
Discussion
Several studies have already demonstrated the excellent performance of CBCT in the detection and assessment of fractures, with radiation doses far below those of conventional MDCT. However, we did not find any study directly comparing CBCT and CR in the detection of fractures and comparing radiation doses of these two imaging modalities. Given the high fracture detection rate and low radiation dose of CBCT, we wondered whether CR could be replaced by CBCT as the first-line examination after small bone and joint trauma.
This study confirmed the results from previous studies regarding the high sensitivity of CBCT in fracture detecting: our readers found 35-37 % more fractures compared to CR. Moreover, CBCT proved to be particularly valuable in diagnosing complex (intraarticular or comminuted) fractures.
The majority of these additionally detected fractures were either nondisplaced or small avulsion fractures, and detecting them had no definite or only limited impact on patient treatment. Nonetheless, we believe that patient reassurance is also an important parameter in these cases. The knowledge that a (small) fracture is present is reassuring for the patient as it explains the cause of their pain.
Performing a CBCT examination is more time-consuming than CR for the radiology technician (due to more precise patient positioning, longer scan time, and post-processing and reconstruction). For the radiologist, the CBCT burden on the global workflow was limited as it took on average only 30 to 50 s longer to interpret a CBCT examination than to evaluate a conventional radiographic examination (2 up to 6 radiographs).
Several studies [3, 7–9] have demonstrated the (relatively) low radiation dose of CBCT compared to MDCT for dental and maxillofacial as well as extremity examinations. In our study, the DAP of cone-beam examinations varied from 107 to 1,530 mGy × cm2. Applying a conversion factor of 0.01 mSv/Gy × cm2, this equals an effective dose (ED) of 1 to 15.3 μSv, indeed far below reported values for MDCT. However, these values were still considerably higher than the ED for the conventional radiographs (0.07 to 5 μSv).
As DAP depends on the scan surface (i.e., field of view), it would be possible to further diminish the ED of CBCT by decreasing the field of view. In our study design we were unable to do so, as the location of the (possible) fracture at first presentation was unknown, and we would not tolerate missing a fracture by applying an FOV that was too limited. If CBCT is used in the further assessment of an already diagnosed fracture (with known location), limiting the FOV will severely decrease the DAP and ED.
The major limitations in our study were the relatively small number of patients, population selection and lack of a gold standard. Our study population included 231 cases divided over 8 small bones/joints, resulting in a small number of patients per joint. There were especially few patients with knee trauma (n = 6), resulting in a low power for detecting differences concerning this joint. Furthermore, we might suffer from a bias in our results due to the exclusion of a part of the general population: elderly patients with tremor and very young patients were excluded because of their inability to remain immobile during the CBCT examination. Given the high susceptibility of CBCT to motion artifacts, image quality in these patients would definitely be suboptimal and lead to inconclusive results. We also acknowledge the lack of an ‘absolute’ gold standard in this study. MDCT is considered the gold standard in the detection of osseous lesions, but performing an additional MDCT examination could not be justified because of the high radiation dose. A previous study [8] demonstrated, however, that although MDCT was more performant in detecting small fracture fragments, the sensitivity of CBCT for fractures equaled that of MDCT. In this previous study, the clinical significance of the missed fragments was however limited as the mean diameter was less than 1 mm and none of them were located intraarticularly. Finally, the number of readers (only 2) and different levels of experience (2 years versus 25 years) should be mentioned, although the results do not show a significant difference in the fractures detected.
Conclusion
This study demonstrates the high sensitivity of CBCT compared to CR in detecting small bone and joint lesions, particularly complex (intraarticular or comminuted) fractures, as well as the high inter- and intraobserver agreement of this modality. However, the higher radiation dose and high susceptibility to motion artifacts are limiting factors in the use of CBCT as a primary imaging modality. Therefore, we suggest performing conventional radiography as the first-line examination and reserving CBCT for those patients with negative radiographs notwithstanding high clinical suspicion or for those with complex fractures in whom better (preoperative) assessment is mandatory.
References
Feldkamp LA, Davis LC, Webb S. Comments, with reply, on: 'Tomographic reconstruction from experimentally obtained cone-beam projections' by S. Webb et al. IEEE Trans Med Imaging. 1988;7:73–4.
Guerrero ME, Jacobs R, Loubele M, Schutyser F, Suetens P, van Steenberghe D. State-of-the-art on cone beam CT imaging for preoperative planning of implant placement. Clin Oral Investig. 2006;10:1–7.
Tsiklakis K, Donta C, Gavala S, et al. Dose reduction in maxillofacial imaging using low dose cone beam CT. Eur J Radiol. 2005;56:413–7.
Dalchow CV, Weber AL, Yanagihara N, et al. Digital volume tomography: radiologic examinations of the temporal bone. AJR Am J Roentgenol. 2006;186:416–23.
Dalchow CV, Weber AL, Bien S, et al. Value of digital volume tomography in patients with conductive hearing loss. Eur Arch Otorhinolaryngol. 2006;263:92–9.
Offergeld C, Kromeier J, Aschendorff A, et al. Rotational tomography of the normal and reconstructed middle ear in temporal bones: an experimental study. Eur Arch Otorhinolaryngol. 2007;264:345–51.
De Cock J, Mermuys K, Goubau J, Van Petegem S, Houthoofd B, Casselman JW. Cone-beam computed tomography: a new low dose, high resolution imaging technique of the wrist, presentation of three cases with technique. Skelet Radiol. 2012;41:93–6.
Faccioli N, Foti G, Barillari M, Atzei A, Mucelli RP. Finger fractures imaging: accuracy of cone-beam computed tomography and multislice computed tomography. Skelet Radiol. 2010;39:1087–95.
Koskinen SK, Haapamäki VV, Salo J, et al. CT arthrography of the wrist using a novel, mobile, dedicated extremity cone-beam CT (CBCT). Skelet Radiol. 2013;42:649–57.
Hiwatashi A, Yoshiura T, Noguchi T, et al. Usefulness of cone-beam CT before and after percutaneous vertebroplasty. AJR Am J Roentgenol. 2008;191:1401–5.
De Groote J, Dewaele T, Defreyne L. Conebeam-CT and fluoroscopy guided percutaneous absolute alcohol sclerotherapy of aneurysmal bone cysts—a single centre experience. JBR-BTR. 2014;97(4):270.
Miracle AC, Mukherji SK. Conebeam CT of the head and neck, Part I: physical principles. AJNR Am J Neuroradiol. 2009;30:1088–95.
Zbijewski W, De Jean P, Prakash P, et al. A dedicated cone-beam CT system for musculoskeletal extremities imaging: design, optimization, and initial performance characterization. Med Phys. 2011;38:4700–13.
Mattila KT, Kankare JA, Kortesniemi M, et al. (2011) Cone beam CT for extremity imaging. EPOS Abstract, ECR 2011, Vienna March 3–7. Doi:10.1594/ecr2011/c-0297
Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009;91:1882–9.
Leng S, Zambelli J, Tolakanahalli R, et al. Streaking artifacts reduction in four-dimensional cone-beam computed tomography. Med Phys. 2008;35:4649–59.
Pasquet G, Cavezian R. Diagnostic means using oral and maxillofacial cone beam computed tomography: results. J Radiol. 2009;90:618–23.
Zeitoun F, Dubert T, Frot B, Laredo JD. Imaging of the wrist and of the hand: what is the best modality? J Radiol. 2001;82:335–52.
Schreibman KL, Freeland A, Gilula LA, Yin Y. Imaging of the hand and wrist. Orthop Clin N Am. 1997;28:537–82.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Smet, E., De Praeter, G., Verstraete, K.L.A. et al. Direct comparison of conventional radiography and cone-beam CT in small bone and joint trauma. Skeletal Radiol 44, 1111–1117 (2015). https://doi.org/10.1007/s00256-015-2127-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2127-3