Abstract
Objective
To validate femoral version measurements made from biplanar radiography (BR), three-dimensional (3D) reconstructions (EOS imaging, France) were made in differing rotational positions against the gold standard of computed tomography (CT).
Materials and methods
Two cadaveric femurs were scanned with CT and BR in five different femoral versions creating ten total phantoms. The native version was modified by rotating through a mid-diaphyseal hinge twice into increasing anteversion and twice into increased retroversion. For each biplanar scan, the phantom itself was rotated −10, −5, 0, +5 and +10°. Three-dimensional CT reconstructions were designated the true value for femoral version. Two independent observers measured the femoral version on CT axial slices and BR 3D reconstructions twice. The mean error (upper bound of the 95 % confidence interval), inter- and intraobserver reliability, and the error compared to the true version were determined for both imaging techniques.
Results
Interobserver intraclass correlation for CT axial images ranged from 0.981 to 0.991, and the intraobserver intraclass correlation ranged from 0.994 to 0.996. For the BR 3D reconstructions these values ranged from 0.983 to 0.998 and 0.982 to 0.998, respectively. For the CT measurements the upper bound of error from the true value was 5.4–7.5°, whereas for BR 3D reconstructions it was 4.0–10.1°. There was no statistical difference in the mean error from the true values for any of the measurements done with axial CT or BR 3D reconstructions.
Conclusion
BR 3D reconstructions accurately and reliably provide clinical data on femoral version compared to CT even with rotation of the patient of up to 10° from neutral.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Femoral version refers to the relationship of the femoral neck axis to the transcondylar axis, or coronal axis, of the distal femur. Femoral anteversion is defined as anterior rotation of the femoral head from the coronal plane (which effectively creates more clinical internal rotation of the long axis of the femur), while retroversion is relative posterior rotation of the femoral head (Figs. 1 and 2). On average, there is 30–40° of anteversion at birth, and it decreases with time to approximately 10–15° in skeletally mature individuals. However, there can be significant variation between individuals and even between contralateral sides [1–3].
Femoral version contributes to the normal stability and function of the hip and knee joints and is an important clinical factor in many pathologic conditions, including torsional syndromes and their sequelae [2], femoral fractures [1], developmental dysplasia of the hip [4], hip joint arthroplasty [5, 6], Legg-Calve-Perthes disease [7] and slipped capital femoral epiphysis [8, 9].
Routine clinical assessment of the femoral version consists of a clinical examination [10] and orthogonal radiographs [11]. For surgical planning, plain radiographs are often inadequate to assess the femoral version, and advanced imaging is needed. Measurements from computed tomography (CT) scans are more accurate than measurements made from plain radiographs [12–14]. As a result, CT imaging is considered the gold standard in femoral version measurement [12].
While CT imaging allows for more accurate version measurement than plain radiographs, it also exposes patients to significantly more ionizing radiation. For this reason, the recent literature has questioned the increasing use of diagnostic CT scans, especially in the pediatric population as children are more susceptible to the effects of radiation [15]. New measurement techniques that allow femoral version to be measured from 3D reconstructions of biplanar radiographs can potentially provide accurate measurements without increased radiation exposure. One such technology is the EOS imaging system and sterEOS software (EOS Imaging, Paris, France), which provides imaging of lower limb torsional alignment at a 4- to 30-times decreased radiation dose compared to a 16-slice CT scanner [16]. Several studies have compared femoral version calculations from CT to measurements made from BR 3D reconstructions [3, 14, 17, 18], but several questions remain. Our primary goal was to assess whether positioning of the patient can contribute to errors in interpreting biplanar radiography. Since no research has looked at error from rotational variation, we created a pilot study to establish reliability with cadavers.
Methods
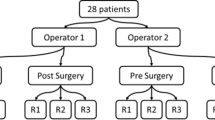
The proximal ends of two cadaveric femurs were attached to stabilizing platforms. A mid-diaphyseal hinge was added to each femur to allow version to be adjusted (Fig. 3). Both femurs were imaged at an unaltered femoral version and with version modified by rotating the distal portions twice into increasing anteversion and twice into increasing retroversion to obtain five phantoms for each femur. The actual values for the rotations were established by 3D CT reconstructions. Supine CT images and upright biplanar images were acquired for each phantom. Within the EOS scanner, phantoms were imaged with the stabilizing platform parallel to the coronal imaging plane and with the platform rotated −10, −5, +5 and +10°. Platform rotation within the EOS scanner was measured using a protractor and the laser positioning lines produced by the scanner (Fig. 4). This resulted in one CT scan and five biplanar imaging scans for each phantom.
The accepted method for calculating femoral version from axial CT images is to measure the angle between a line tangent to the posterior femoral condyles and a line through the center of the femoral neck [12–14] (Figs. 1 and 2). This method requires multiple CT slices through the hip and knee to identify the correct view of the posterior condyles and center of the femoral neck on axial views. Two independent observers measured the femoral version from each set of axial CT images at two different time points using custom MATLAB software (Mathworks, Natick, MA).
Version measurements were made from each BR 3D reconstruction using sterEOS software, which was introduced for torsional measurements by Chaibi et al. [19]) and has been used in several studies [3, 17, 18). The two observers had no experience in sterEOS prior to the study, but underwent appropriate training before making study measurements. SterEOS software guides the observers through the identification of important femoral landmarks, such as the head, neck, greater and lesser trochanters, distal condyles and proximal shaft (Fig. 5). The software adjusted a template femoral model to fit the identified landmarks, then automatically calculated femoral version from the model. Each observer completed the sterEOS measurement process at two different time points for each reconstruction.
We used 3D CT reconstructions as our “true” femoral version. High-quality surface reconstructions were created for all phantoms from CT images using MIMICS (Materialise, Leuven, Belgium), which has been demonstrated to produce highly accurate 3D reconstructions from CT using a single predefined set of parameters [12, 19]. The femoral version of each model was calculated using MATLAB. For this calculation: (1) the measurement plane was defined to be perpendicular to the anatomical axis of the femur; (2) a line was placed through the center of the femoral neck; (3) the condyle plane was defined to be tangential to both femoral condyles and perpendicular to the measurement plane. The femoral version was defined to be the angle between the femoral neck centerline and condyle plane projected into the measurement plane (Fig. 2). Manually determining the version of cadaveric femurs in the laboratory can be accurate, but also introduces complexity and possible error. Since MIMICS 3D CT reconstructions are accurate and eliminate the possible error of manual measurements, these 3D surface measurements were considered the “true” femoral version for each phantom.
Statistics
Inter- and intraobserver reliability and error from the true version were determined for both scanning techniques. Mean errors and 95 % confidence intervals were calculated for each technique. The measurement accuracies of axial CT measurements and BR 3D reconstruction measurements at all platform rotations were compared using repeated measures ANOVA. Significance was set to p < 0.05.
No a priori power analysis could be performed because of the paucity of research on the topic. Without understanding the clinical significance of error in rotation, a valid post hoc analysis is difficult to determine. The primary outcome measure for this study was the intraclass coefficients of the measures.
Results
The true femoral versions of the phantoms derived by rotating the first femur about the mid-diaphyseal hinge were −20.1, −7.7, 3.6, 12.2 and 20.6°. The phantoms derived by rotating the second femur were 19.1, 26.2, 37.8, 44.7 and 50.6° (Fig. 6). The version values indicate that the second femur was much more anteverted than the first femur.
For axial CT measurements, the interobserver intraclass correlation (ICC) ranged from 0.981–0.991, and the intraobserver ICC ranged from 0.994 to 0.996. For BR 3D reconstructions, the interobserver ICC ranged from 0.983 to 0.998, and the intraobserver ICC ranged from 0.982 to 0.998.
For axial CT measurements, the upper bound error was 5.4–7.5°. The upper bound error was 4.0–10.1° for BR 3D reconstructions (Table 1, Fig. 6) for all rotations of the platform. There was no statistical difference in the combined average measurement error from the true values between any of the BR 3D reconstructions and CT (p = 0.34, Table 2).
Discussion
Assessment of femoral version is necessary in many clinical situations including trauma, malalignment/torsional syndromes, developmental dysplasia of the hip and hip joint reconstruction. Treatment decisions, surgical planning and outcomes depend on this measurement. Hip instability, rotational deformity and altered gait can result from incorrect femoral version. By using imaging phantoms, our study compared axial CT and BR 3D reconstruction measurements to “true” version values in the form of 3D reconstructions from CT. To our knowledge, we are the first to assess whether phantom rotation altered the femoral version values obtained by BR 3D reconstruction. Our results show that measurements were robust up to even 10° of phantom malrotation within the scanner.
CT has been shown to provide accurate estimates of femoral version, but there is increasing concern with the radiation exposure. MRI has been used as an alternative in some situations, but it also has drawbacks including increased cost, time and possible motion artifacts. Patients undergoing MRI may also require anesthesia, which increases the cost and risk to the patient [20]. Technology such as EOS appears to provide similar results, but with a fraction of the radiation exposure [3, 16, 21], and it is time effective. An additional benefit of imaging subjects with the biplanar radiography technique is that the imaging can be performed upright to simulate weight-bearing situations.
Kuo et al. [14] compared cadaveric femoral CT and biplanar radiography without 3D reconstructions, but based on a method described by Ogata and Goldsand [11]. They found that there was no statistical difference between CT and the anatomic reference. However, they found version was significantly (p = 0.004) overestimated when comparing the biplanar radiographs to the anatomic references measuring a mean difference of 13.5° more anteversion. The 95 % confidence limit for the anatomic reference was 7.3–12.0° compared to 18.1–28.0° for biplanar radiography. There was also increased inter- and intraobserver variability with biplanar radiographs compared to CT. Our study and others [3, 16, 18, 22] show that with the new imaging software available, the measurements from 3D reconstructions of biplanar radiography are accurate and reproducible.
The results in our study comparing axial CT cuts and BR 3D reconstructions were similar to those of similar recent studies [3, 17, 18] in showing high inter- and intraobserver agreement. The study by Buck et al. [17] was on adult patients about to undergo total knee replacement. In their analysis of the femoral version, the ICC for the CT measurements was 0.952 (95 % CI, 0.905–0.976), and with the BR 3D reconstructions, it was 0.943 (95 % CI, 0.886–0.971). They used a method for obtaining the biplanar images described by Chaibi et al. [22] where one foot is placed slightly anterior to the other to decrease the overlap of the limbs and make landmarks on the lateral view easier to identify. They concluded that the average difference between CT and BR 3D reconstructions was 0° (range of −5 to 7°).
The study by Rosskopf et al. [18] that studied 50 children and adolescents had an average difference of 4.9 ± 3.8° when comparing femoral version measurements using CT and BR 3D reconstructions. The intermethod ICC for BR 3D reconstructions was 0.90, and the interreader ICC was 0.93 –0.97. This study also positioned the patient as described by Chaibi [22]. This study also demonstrated a high variability in femoral version (−13 to 59° by CT and −6 to 65° for BR 3D reconstructions) in this younger patient population. It also highlighted the importance of positioning as these patients may have less bone mineral density than adults, making it more difficult to identify landmarks for the sterEOS software.
The retrospective study by Folinais et al. [3] of 43 limbs in 30 adult patients being evaluated prior to or after hip replacement found no statistically significant difference (P = 0.5) between femoral version measured by BR 3D reconstructions (13.4 ± 9.1°) and CT (13.7 ± 9.4°), with ICC of 0.93 for BR 3D reconstructions and 0.86 for CT. In the study they intentionally positioned the patients either rotated 15° relative to the acquisition system or had the contralateral limb flexed out of the way to help differentiate anatomical landmarks on the lateral view. This positioning did not seem to affect results given the agreement between BR 3D reconstructions and CT, but the sample sizes were too small to find a difference between the positioning methods. This is pertinent to our study as we found imaging that was 10° from neutral rotation in the biplanar radiographic scanner to be in high agreement with the CT imaging. In the study by Folinais et al., they also mention the radiation doses administered. For the biplanar radiograph system made by EOS imaging, the mean radiation dose measured was 0.18 ± 0.05 mGy for the AP view and 0.45 ± 0.08 mGy for the lateral view; for the CT they estimated according to the established protocol (femoral and tibial torsion measurements) that the dose was 8.4 to 15.6 mGy. This supports the contention that biplanar radiograph reconstructions like those created from the EOS imaging system require significantly less radiation exposure than CT.
To further discuss radiation exposure, the study by Delin et al. [16] examined the exposure in CT versus biplanar radiographs in measurements of limb torsion and anteversion. They found that CT doses were 4 times higher to the ovaries, 24 times higher to the testicles and 13–30 times more to the knees and ankles. A different study by Saltybaeva et al. [23] on standardized models found routine CT measurements at the knee and ankle may not produce clinically significant radiation [23]. However, they ascertained that a CT of the hip requires 28.5 times more radiation than that of the knee in an adult and 14 times more in a newborn. This is further evidence that CT measurements at the hip may be a source of excessive radiation.
The main advantage of our study is that it provided a controlled situation to obtain our measurements. By using two different femurs with varying versions we could assess the agreement of the BR 3D reconstructions with CT without interference of other structures, limit variability by studying the same femora and not expose living patients to radiation. Another notable finding of the study is that compared to other studies [3, 17, 18], the observers were relative novices to the EOS imaging system, but were still able to achieve high inter- and intraclass correlations showing a relative ease of use and quick learning curve for the sterEOS software.
Our study had several limitations. First, by testing only two femurs we limited our ability to draw distinct conclusions about all clinical situations. This issue can only be alleviated by future clinical validation of rotation now that the cadaver pilot study has been completed. Additionally, our “true” anteversion values were based on imaging as opposed to directly measuring from the anatomic reference. However, as addressed before, we felt that certain advantages were presented by using 3D reconstructions of the CT images as our true value including ease and reduction of error. In addition, it is rare to be able to assess anatomic version with anything but imaging. To completely expose the landmarks necessary to directly measure version is morbid and usually avoided. We felt that 10° was satisfactory in accounting for error in positioning or allowing visualization of the anatomic landmarks on the lateral view, but additional rotations beyond 10° within the EOS imaging scanner could further elucidate its limitations. Also, an assessment of cost and development of pathology associated with different imaging modalities may prove to be valuable. However, until the long-term effects of radiation exposure are better understood, our ability to perform long-term cost analysis is limited. Finally, it has been shown that femoral version in adults and children [1, 24] can vary as much as 15–18° from one side to another, but it is unknown how much femoral version alteration becomes clinically relevant. For this reason, it is unclear whether the error in BR 3D reconstruction measurements (4.0–10.1°) has any clinical relevance.
Future clinical validation of BR 3D reconstructions can now be reliably performed knowing that the inter- and intraobserver measurements have excellent correlation and that deviation from perfect AP and lateral scanning still provides valid measures of femoral rotation. These future clinical studies can now focus on validating the significance in rotation of the pathologies associated with femur fractures, developmental dysplasia of the hip, hip joint arthroplasty, Legg-Calve-Perthes disease, and slipped capital femoral epiphysis.
Our study reinforces previous research showing that BR 3D reconstructions using the EOS imaging system can measure femoral version with accuracy comparable to that of CT. Additionally, measurements were not affected by up to 10° of patient rotation within the scanner.
References
Brouwer KJ, Molenaar JC, van Linge B. Rotational deformities after femoral shaft fractures in childhood. A retrospective study 27–32 years after the accident. Acta Orthop Scand. 1981;52(1):81–9.
Leonardi F, Rivera F, Zorzan A, Ali SM. Bilateral double osteotomy in severe torsional malalignment syndrome: 16 years follow-up. J Orthop Traumatol. 2013;15:131–6.
Folinais D, Thelen P, Delin C, Radier C, Catonne Y, Lazennec JY. Measuring femoral and rotational alignment: EOS system versus computed tomography. Orthop Traumatol Surg Res: OTSR. 2013;99(5):509–16.
Sankar WN, Neubuerger CO, Moseley CF. Femoral anteversion in developmental dysplasia of the hip. J Pediatr Orthop. 2009;29(8):885–8.
Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21(5):696–701.
Daly PJ, Morrey BF. Operative correction of an unstable total hip arthroplasty. J Bone Joint Surg Am. 1992;74(9):1334–43.
Kim HT, Wenger DR. “Functional retroversion” of the femoral head in Legg-Calve-Perthes disease and epiphyseal dysplasia: analysis of head-neck deformity and its effect on limb position using three-dimensional computed tomography. J Pediatr Orthop. 1997;17(2):240–6.
Gelberman RH, Cohen MS, Shaw BA, Kasser JR, Griffin PP, Wilkinson RH. The association of femoral retroversion with slipped capital femoral epiphysis. J Bone Joint Surg Am. 1986;68(7):1000–7.
Stanitski CL, Woo R, Stanitski DF. Femoral version in acute slipped capital femoral epiphysis. J Pediatr Orthop B. 1996;5(2):74–6.
Ruwe PA, Gage JR, Ozonoff MB, DeLuca PA. Clinical determination of femoral anteversion. A comparison with established techniques. J Bone Joint Surg Am. 1992;74(6):820–30.
Ogata K, Goldsand EM. A simple biplanar method of measuring femoral anteversion and neck-shaft angle. J Bone Joint Surg Am. 1979;61(6A):846–51.
Abel MF, Sutherland DH, Wenger DR, Mubarak SJ. Evaluation of CT scans and 3-D reformatted images for quantitative assessment of the hip. J Pediatr Orthop. 1994;14(1):48–53.
Hernandez RJ, Tachdjian MO, Poznanski AK, Dias LS. CT determination of femoral torsion. AJR Am J Roentgenol. 1981;137(1):97–101.
Kuo TY, Skedros JG, Bloebaum RD. Measurement of femoral anteversion by biplane radiography and computed tomography imaging: comparison with an anatomic reference. Investig Radiol. 2003;38(4):221–9.
Brenner DJ, Hall EJ. Computed tomography–an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–84.
Delin C, Silvera S, Bassinet C, Thelen P, Rehel JL, Legmann P, et al. Ionizing radiation doses during lower limb torsion and anteversion measurements by EOS stereoradiography and computed tomography. Eur J Radiol. 2014;83(2):371–7.
Buck FM, Guggenberger R, Koch PP, Pfirrmann CW. Femoral and tibial torsion measurements with 3D models based on low-dose biplanar radiographs in comparison with standard CT measurements. AJR Am J Roentgenol. 2012;199(5):W607–612.
Rosskopf AB, Ramseier LE, Sutter R, Pfirrmann CW, Buck FM. Femoral and tibial torsion measurement in children and adolescents: comparison of 3D models based on low-dose biplanar radiography and low-dose CT. AJR Am J Roentgenol. 2014;202(3):W285–291.
Gelaude F, Vander Sloten J, Lauwers B. Accuracy assessment of CT-based outer surface femur meshes. Comput Aided Surg: Off J Int Soc Comput Aided Surg. 2008;13(4):188–99.
Malviya S, Voepel-Lewis T, Eldevik OP, Rockwell DT, Wong JH, Tait AR. Sedation and general anaesthesia in children undergoing MRI and CT: adverse events and outcomes. Br J Anaesth. 2000;84(6):743–8.
Deschenes S, Charron G, Beaudoin G, Labelle H, Dubois J, Miron MC, et al. Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine (Phila Pa 1976). 2010;35(9):989–94.
Chaibi Y, Cresson T, Aubert B, Hausselle J, Neyret P, Hauger O, et al. Fast 3D reconstruction of the lower limb using a parametric model and statistical inferences and clinical measurements calculation from biplanar X-rays. Comput Methods Biomech Biomed Eng. 2012;15(5):457–66.
Saltybaeva N, Jafari ME, Hupfer M, Kalender WA. Estimates of effective dose for CT scans of the lower extremities. Radiology. 2014;132903.
Tomczak RJ, Guenther KP, Rieber A, Mergo P, Ros PR, Brambs HJ. MR imaging measurement of the femoral antetorsional angle as a new technique: comparison with CT in children and adults. AJR Am J Roentgenol. 1997;168(3):791–4.
Acknowledgments
The authors wish to acknowledge Tracey Bastrom for her statistical assistance and Christine Farnsworth for assistance with completion of the manuscript.
Conflict of interests
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pomerantz, M.L., Glaser, D., Doan, J. et al. Three-dimensional biplanar radiography as a new means of accessing femoral version: a comparitive study of EOS three-dimensional radiography versus computed tomography. Skeletal Radiol 44, 255–260 (2015). https://doi.org/10.1007/s00256-014-2031-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-014-2031-2