Abstract
Background
Image-guided intussusception reduction has been practised internationally for many decades. The use of different modalities, delayed repeat attempts, and sedation/anaesthesia are unknown.
Objective
To survey the practice of image-guided intussusception reduction.
Materials and methods
A 20-point questionnaire created by the European Society of Paediatric Radiology (ESPR) Abdominal Imaging Taskforce was distributed via the ESPR members’ mailing list and shared on social media between 28 March and 1 May 2023.
Results
There were 69 responses from 65 worldwide institutions, with a mean of 18 intussusception reductions performed per year: 55/69 (80%) from 52 European institutions and 14/69 (20%) from 13 institutions outside of Europe. European centres reported using 19/52 (37%) fluoroscopy, 18/52 (35%) ultrasound, and 15/52 (28%) a mixture of both, with 30/52 (58%) offering a delayed repeat at 15 min to 24 h. Non-European centres reported using 5/13 (39%) fluoroscopy, 6/13 ultrasound (46%), and 2/13 (15%) a mixture of both, with 9/13 (69%) offering a delayed repeat attempt. Sedation or analgesia was used in 35/52 (67%) of European and 2/13 (15%) non-European institutions.
Conclusion
There is wide variation in how image-guided intussusception reduction is performed, and in the use of sedation/anaesthesia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intussusception is the telescoping and entrapment of a bowel segment into more distal gastrointestinal loops. Ileocolic intussusception is the most common type and involves the terminal ileum invaginating into the colon for a varying length, with mesenteric fat, lymph nodes, and vessels. The trapped bowel and mesentery can cause upstream bowel obstruction, oedema, eventual ischaemia, and perforation; therefore, urgent reduction is a priority to prevent loss of viable bowel. Image-guided enema reduction is the first-line treatment internationally for ileocolic intussusception not complicated by peritonitis, shock, or sepsis. The quoted success rate varies widely due to discrepancies in the definition and heterogenous data; it is reported to be 24–95% in published data [1], but the generally accepted rate of successfully reducing an intussusception without the child requiring surgical intervention is approximately 75–80% [2, 3], although this may vary depending on the presence of a pathological lead point seen in approximately 10% [1, 4].
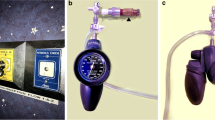
There is consensus on the use of ultrasound as a diagnostic test for ileocolic intussusception, but variation exists in the methods of intervention. Hydrostatic reduction with ultrasound is widely practiced, often with the addition of dilute water-soluble contrast to confirm a successful reduction fluoroscopically at the end of the study. The use of fluoroscopy with either pressurised gas or water-soluble contrast remains the standard intervention in many centres. There is currently no accepted consensus and current evidence suggests that both guidance methods appear to have good success rates with limited difference in perforation rates [5,6,7]. In addition, there is no international agreement on whether sedation or anaesthetic should be used.
The objective of the European Society of Paediatric Radiology (ESPR) Abdominal Imaging Taskforce is to survey and evaluate how radiological intussusception reduction is carried out at different institutions, particularly in relation to the use of fluoroscopy versus ultrasound as a guidance modality, and the experience of using sedation or general anaesthetic (GA) in this setting. The aim is to establish current practice with a view to issuing evidence-based guidance in the future.
Materials and methods
Ethical approval was not required for this optional survey of participants’ experience. Informed written consent to publish individual, anonymised responses was obtained from all participants.
Survey design, distribution and analysis
A 20-point questionnaire was created by the ESPR Abdominal Imaging Taskforce using the Google Forms platform [8]. The survey included sections on place of work, grade, and profession of the person performing the reduction, and specific details regarding radiological modality, distension medium, and whether or not sedation or anaesthetic are routinely offered. The questions were split into three sections as follows: background data, reduction methods, and the use of sedation/GA/analgesia (Table 1).
The survey was distributed via the ESPR members’ mailing list on 28 March 2023 and was available for responses until 1 May 2023. The survey was also shared via ESPR social media networks and sent personally to colleagues of the ESPR Abdominal Imaging Taskforce.
Descriptive statistics with simple proportions for the responses of each question were calculated and results displayed as bar charts. The qualitative results from open questions regarding sedation and GA were grouped into themes and reproduced without editing.
Results
Survey participants and institutions
During the 1-month questionnaire period, 71 responses were obtained from 67 institutions across 29 countries worldwide: 57/71 (80%) participants were from 54 unique European institutions, across 18 European countries, and 14/71 (20%) participants were from 13 non-European institutions across 11 countries (Table 2). There was a relative lack of responses from Eastern Europe (Fig. 1), compared to the rest of Europe. Two participants from Estonia and Spain reported that intussusception reduction was not performed at their institutions; their responses were not included in the rest of the survey, leaving 69 survey participants from 65 unique institutions in total worldwide: 55 participants from 52 unique European institutions and 14 participants from 13 non-European institutions.
Participating countries: Worldwide (a) and Europe (b). Maps created using https://www.mapchart.net/world.html
Participant job role
Those that practiced paediatric radiology full time constituted 46/55 (83%) of the participants in Europe, 7/55 (13%) practiced a mixture of adult and paediatric radiology, 5/7 (71%) majority of working time in paediatric radiology and 2/7 (29%) majority of working time in adult radiology, 1/55 (2%) respondent was a paediatric surgeon, and 1/55 (2%) respondent was a retired paediatric radiologist (Fig. 2). Of the non-European respondents, 6/14 (43%) practiced paediatric radiology full time, 7/14 (50%) practiced a mixture, 5/7 (71%) majority paediatric and 2/7 (29%) majority adult radiology, and 1/14 (7%) was a paediatric surgeon.
Where is the intussusception reduction performed?
When asked where intussusception reduction is performed (more than 1 choice allowed), 48/52 (92%) participants from unique European institutions and 12/14 (86%) from non-European institutions performed reductions in the diagnostic radiology department (Fig. 3).
Operator
The survey allowed multiple responses about the operator of intussusception reductions and 35/52 (67%) participants from European institutions responded with a single answer: 27/35 (77%) radiology consultant; 6/34 (18%) trainee with consultant supervision; 1/34 (3%) trainee without direct consultant supervision; and 1/34 (3%) surgeon. In the 17 participants with >1 response, 16/17 (94%) involved a radiology consultant, 14/17 (82%) trainee with consultant supervision, and 4/17 (24%) surgeon (Fig. 4). In non-European institutions, 13/14 (93%) respondents reported a radiology consultant performing or supervising intussusception reductions, and 1/14 (7%) participant reported intussusception reductions at their institution were performed by a surgeon.
Number of intussusception reductions
The participants were asked to estimate the number of intussusception reductions performed at their centre per year. The mean number of intussusception reductions performed per year across the 52 unique European institutions surveyed was 17 (range 2–60), comparable to a mean of 13, range (3–60) in the 13 centres outside of Europe.
Modality and reduction medium
The imaging modality and reduction method used by 52 unique European and 13 non-European institutions is presented in Fig. 5. There was wide variation in the methods used across Europe, with 19/52 (37%) choosing fluoroscopy, 18/52 (35%) ultrasound, and 15/52 (28%) using a mixture of both. Ultrasound with fluid was the most popular combination inside and outside of Europe, utilised by 17/52 (33%) European institutions, with those using fluoroscopy having an almost equal split between fluid and gas as the chosen reduction medium: 10/19 (53%) and 9/19 (47%), respectively. Of the 17 institutions that reported using ultrasound with fluid, 12/17 (71%) reported a radiology consultant as the operator, 8/17 (47%) have trainees under direct consultant supervision, and 1/17 (6%) reported a surgeon as the operator (>1 answer permitted). Two European centres also reported using manual manipulation alongside ultrasound—one centre reported a surgeon and the other centre reported a radiology consultant or trainee under direct supervision as the operator. Of the two institutions who reported having the highest number of intussusception reductions per year (60), both used ultrasound-fluid reduction. Of the eight European institutions that reported < 5 intussusception reductions per year, 5/8 (63%) used fluoroscopy (two with fluid, three with gas), 2/8 (25%) used ultrasound with fluid, and 1/8 (13%) used both ultrasound and fluoroscopy with fluid (Fig. 6). There were otherwise no specific trends in modality utilised versus the number of intussusception reductions per year.
Success rate
The participants were asked to estimate the success rate of intussusception reductions at their institution. Four out of fifty-two (8%) European institutions reported a <70% success rate, 17/52 (33%) reported a 70–90% success rate, and 30/52 (58%) reported a success rate of >90%. One participant responded that there was no current audit. There was proportionally higher use of ultrasound versus fluoroscopy in the centres with a self-reported success rate of >90% compared to those with lower self-reported success rates. However, the number of intussusception reductions performed per year has likely confounded this result; there were proportionally higher success rates reported amongst institutions that performed higher numbers of intussusception reductions.
Delayed repeat attempt
In the 52 unique European institutions, 30/52 (58%) reported offering a delayed repeat attempt at intussusception reduction if the first attempt failed, comparable to 9/13 (69%) of the institutions from outside of Europe. The repeated attempts ranged in time interval from 15 min to 24 h, median 1–3 h, after the initial attempt (Fig. 7). One institution reported repeating the attempt after hydrating the child.
Sedation and general anaesthetic
Sedation or GA was reported to be used by 35/52 (67%) European institutions and 2/13 (15%) institutions outside of Europe (Fig. 8). Of the European institutions, 3/35 (9%) use GA, 26/35 (74%) use sedation, 6/35 (18%) use either GA or sedation. An anaesthetist oversees the sedation/GA administration in 19/35 (54%) institutions, paediatrician 7/35 (20%), nurse 2/35 (6%), surgeon 2/35 (6%), emergency physician 2/35 (6%), radiologist 1/35 (3%), neonatologist OR anaesthetist 1/35 (3%), and unknown in 1/35 (3%) (Fig. 9). The proportion using sedation or GA was slightly higher in those using ultrasound rather than fluoroscopy alone, as expected due to the need to keep the child as still as possible when using ultrasound (Fig. 10). The most common reasons given for using GA or sedation were for the comfort of the child, to increase chance of success and to relax the abdomen/improve compliance (Table 3).
There were 17/52 (33%) European institutions and 11/13 (85%) non-European institutions who reported not using sedation or GA. In the European institutions, 8/17 (47%) used analgesia only and 9/17 (53%) did not use analgesia. In the institutions outside of Europe, 4/11 (36%) used analgesia and 7/11 (64%) did not.
The reasons given for not using GA or sedation can be categorised into staffing/institutional limitations, the view that sedation/GA are not required, and potential risks to the child (Table 4). Staffing and institutional reasons were the most common, stated by 12/17 (71%) of the European institutions. Medications used for sedation and analgesia used are given in Table 5.
Discussion
This survey, which includes participants from 52 European institutions and 13 institutions outside of Europe, performing between two and 60 image-guided intussusception reduction procedures per year, confirms wide variation in modality used, the offering of a delayed repeat attempt, and the use of sedation or GA. In Europe, 19/52 (37%) use fluoroscopy guidance, compared to 18/52 (35%) ultrasound and 15/52 (28%) a mixture of both, with fluoroscopy being more popular in institutions who perform < five reductions per year 5/8 (63%), which perhaps relates to fluoroscopic reduction being the more traditional and well-established method [9]. This coupled with a reducing incidence of ileocolic intussusception, due to the recent pandemic [10] and an unpublished observation made amongst some in the paediatric radiology community since before the pandemic, may mean that centres currently using fluoroscopy would not be able to achieve adequate case numbers to train in ultrasound-guided reduction. Only one European institution used gas as a reduction medium with ultrasound, which can be explained by fluid being the more easily visible medium on ultrasound with a similar safety efficacy and safety profile [11]. Outside of Europe, 5/13 (38%) use fluoroscopy, 6/13 (46%) ultrasound, and 2/13 (15%) use both. The majority (30/52, 58% in Europe and 8/13, 62% outside of Europe) self-reported an estimated success rate of >90%. The use of ultrasound and the number of intussusception reductions per year were both proportionally higher in those that reported a success rate of >90%, although the rate of irreducible intussusception (for example, due to pathological lead point) is unknown and may be a confounder. Thirty out of 52 (58%) European institutions and 9/13 (69%) non-European institutions offer a delayed repeat attempt. Thirty-five out of 52 (67%) European institutions and 2/13 (15%) non-European institutions use sedation or GA. Although participant numbers are relatively small, the survey confirms a large degree of variability across all stages of intussusception reduction and is likely due to a combination of institutional preferred methods and the available evidence, which does not show large differences in success rate by modality, the use of delayed repeat attempts, or GA/sedation. Survey responses could have been increased with further reminder email communications, direct communication with the departments of major paediatric centres, or incentives.
Overall, there were almost equal numbers of institutions using fluoroscopy versus ultrasound guidance (37% and 35%, respectively). In comparison to a prior ESPR survey from 1999 with 204 respondents [12], the use of ultrasound as image guidance in intussusception reduction has increased from 9.5% who used ultrasound alone, and 18% who used ultrasound with radiography. Similarly, a prior Society of Pediatric Radiology (SPR) survey in 2015 [13] reported that 96% of 456 respondents used fluoroscopy as the guidance method. Although there were no respondents from the USA, and only one from Canada, European institutions tend towards being more ultrasound focused, for example, in the diagnosis of midgut malrotation which has only been adopted by North American institutions in recent years [14], and in the use of contrast-enhanced ultrasound instead of fluoroscopic micturating cystourethrogram [15, 16]. The trend demonstrated by this survey compared to the prior ESPR survey, however, does suggest an apparent shift towards more institutions using ultrasound, which is welcome, given the comparable effectiveness and safety of the method, and the added benefit of no ionising radiation.
The evidence for a delayed repeat is limited [17] and the survey returned results which could not be easily extrapolated. Firstly, the survey question did not define a time frame for a “delayed” repeat attempt and some centres reported attempts as early as 15 min as delayed, whereas some may define this as a repeated attempt within the same session. It is also possible that the term “delayed repeat attempt” may have been misinterpreted as a second attempt should an intussusception reoccur. Nevertheless, it seems that the use of a delayed repeat attempt in some form is utilised by 30/52 (58%) of European centres and may be a point for further consideration and detailed multicentre investigation in the future as it is currently not possible to draw conclusions on whether it is useful. Data on success rate of the delayed attempt was deemed outside of the scope of the survey; to draw accurate inferences from the results, we would have required the survey participants to record actual rather than estimated success rates, and this was unlikely to be data that was immediately available to all. It may not be advisable to delay for too many hours due to the risk of impending necrosis of bowel; there is a relationship between duration of symptoms > 24 h and ischaemic bowel requiring resection in childhood intussusception.
There was variation in the use of sedation and GA and differences were demonstrated inside and outside of Europe, with centres inside of Europe having a greater propensity to sedate or use GA, compared to those outside of Europe who tended towards regular analgesia or nothing at all. The use of sedation in North America has been previously reported in the aforementioned SPR survey, where 93% of respondents did not sedate [13]. In this current survey, those that use sedation or GA reported usually doing so via an anaesthetist and most commonly for the comfort of the child, although many also believe that it increases chances of success. Those that do not use sedation or GA in contrast mainly do so due to staffing or logistical reasons, a belief that it is not necessary, or due to perceived risks to the child. The limited literature on this topic suggests that success rates may be higher with the use of sedation or GA [18,19,20]. There are concerns of increased perforation rate, although the data on this is very limited and numbers are too small to draw definitive conclusions [21]. It is also unknown as to whether GA or sedation is the better option, although recent literature suggests the easier conversion to an operative procedure makes GA a more attractive option [22], assuming the operation takes place in the same location as the reduction attempt.
The survey had limitations which must be acknowledged. The survey advertised on social media and therefore was accessible to anyone. Responses included open text but there were no responses that were deemed nefarious or unlikely to come from a genuine source. There was a risk of selection bias; paediatric radiologists who were not ESPR members and who do not follow ESPR on social media may not have seen or responded to the survey. The survey was also only open for a short time frame (1 month), the sample size is relatively small, and an estimation of the representativeness of the survey has not been specifically calculated. However, at least one response from 52 different European institutions with broad geographical coverage does seem reasonable in terms of displaying the diversity in how reductions are performed and to illustrate the need for more evidence-based guidelines. Further responses may have resulted in numerous participants from the same institutions, which may have not added to the results, unless there were intra-institutional differences. The added value of including responses from non-European countries was limited as the numbers were small and from disparate locations which did not include the USA, Russia, or China. The snapshot suggests there are differences, for example, in the use of sedation and the use of ultrasound within Europe compared to outside of Europe, although “outside of Europe” does not represent all non-European countries.
In terms of the survey content, there were limitations in what to include to make the questionnaire a convenient length and the data non-onerous for participants to obtain, without the need for extracting system data. This meant that data on accurate success rates, time to reduction attempt, lead points, and surgical outcomes were not collected and may have provided some context to the findings. On retrospect, data on complication rates could have been collected in the same manner as success rate, using broad range estimations and accepting a degree of skew due to confirmation bias.
Following this demonstration of wide variability in practice at all stages of intussusception reduction across institutions, it is now appropriate to develop evidence-based guidance.
Conclusion
The survey confirms wide variation in the practice of intussusception reduction, based on replies from institutions performing as little as two, to as many as 60 reductions per year and no current consensus on modality, the use of a delayed repeat attempt, or sedation/general anaesthetic. Establishing a unified, evidence-based approach for Europe could be beneficial for all those involved in radiology-led intussusception reduction.
Data Availability
Data available within the article.
References
Bekdash B, Merven S, Sprigg A (2013) Reduction of intussusception: defining a better index of successful non-operative treatment. Pediatr Radiol 43:649–656
Sadigh G, Zou K, Razavi S et al (2015) Meta-analysis of air versus liquid enema for intussusception reduction in children. AJR Am J Roentgenol 205:W542-549
Rosenfeld K, McHugh K (1999) Survey of intussusception reduction in England, Scotland and Wales: how and why we could do better. Clin Radiol 54:452–458
Fiegel H, Gfroerer S, Rolle U (2016) Systematic review shows that pathological lead points are important and frequent in intussusception and are not limited to infants. Acta Paediatr 105:1275–1279
Chew R, Ditchfield M, Paul E, Goergen S (2017) Comparison of safety and efficacy of image-guided enema reduction techniques for paediatric intussusception: a review of the literature. J Med Imaging Radiat Oncol 61:711–717
Plut D, Phillips G, Johnston P, Lee E (2020) Practical imaging strategies for intussusception in children. AJR Am J Roentgenol 215:1449–1463
Sanchez T, Doskocil B, Stein-Wexler R (2015) Nonsurgical management of childhood intussusception: retrospective comparison between sonographic and fluoroscopic guidance. J Ultrasound Med 34:59–63
Google Forms (2023) ESPR intussusception reduction survey. Available: https://forms.gle/ypmvgjPd64uuALrP7. Accessed 30 April 2023
Gu L, Alton D, Daneman A et al (1988) Intussusception reduction in children by rectal insufflation of air. AJR Am J Roentgenol 150:1345–1348
Yoon S, Han C, Eun S (2022) Impact of the COVID-19 pandemic on the incidence of intussusception: a systematic review. Eur Rev Med Pharmacol Sci 26:9040–9049
Xie X, Wu Y, Wang Q et al (2018) A randomized trial of pneumatic reduction versus hydrostatic reduction for intussusception in pediatric patients. J Pediatr Surg 53:1464–1468
Schmit P, Rohrschneider W, Christmann D (1999) Intestinal intussusception survey about diagnostic and nonsurgical therapeutic procedures. Pediatr Radiol 29:752–761
Stein-Wexler R, O’Connor R, Daldrup-Link H, Wootton-Gorges S (2015) Current methods for reducing intussusception: survey results. Pediatr Radiol 45:667–674
Nguyen H, Sammer M, Ditzler M et al (2021) Transition to ultrasound as the first-line imaging modality for midgut volvulus: keys to a successful roll-out. Pediatr Radiol 51:506–515
Riccabona M (2012) Application of a second-generation US contrast agent in infants and children-a European questionnaire-based survey. Pediatr Radiol 42:1471–1480
Ellison J, Maxfield C, Wiener J (2009) Voiding cystography practices and preferences of North American pediatric urologists. J Urol 182:299–304
Navarro O, Daneman A, Chae A (2004) Intussusception: the use of delayed, repeated reduction attempts and the management of intussusceptions due to pathologic lead points in pediatric patients. AJR Am J Roentgenol 182:1169–1176
van de Bunt J, Veldhoen E, Nievelstein R et al (2017) Effects of esketamine sedation compared to morphine analgesia on hydrostatic reduction of intussusception: a case-cohort comparison study. Paediatr Anaesth 27:1091–1097
Giacalone M, Pierantoni L, Selvi V et al (2022) Midazolam premedication in ileocolic intussusception: a retrospective multicenter study. Eur J Pediatr 181:3531–3536
Teoh K, Palmer G, Teague W et al (2021) Periprocedural analgesia and sedation in air enema reduction for intussusception: a retrospective Australian cohort study. J Paediatr Child Health 57:103–108
Feldman O, Weiser G, Hanna M et al (2017) Success rate of pneumatic reduction of intussusception with and without sedation. Paediatr Anaesth 27:190–195
Khorana J, Tepjuk S, Singhavejsakul J et al (2023) A comparison of the success rate of pneumatic reduction in intussusception between general anesthesia and deep sedation: a randomized controlled trial. Pediatr Surg Int 39:186
Author information
Authors and Affiliations
Contributions
G.P. conceptualised and designed the study. R.M., L-S.O-M., S.S., S.F.A., C.S., A.C., P.P., and G.P prepared material and collected data. R.M. and G.P. performed data analysis and wrote the first draft of the manuscript. All authors contributed to review and editing of the draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Meshaka, R., Müller, LS.O., Stafrace, S. et al. Intussusception reduction methods in daily practice—a survey by the European Society of Paediatric Radiology Abdominal Imaging Taskforce. Pediatr Radiol 54, 571–584 (2024). https://doi.org/10.1007/s00247-023-05798-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05798-0