Abstract
Intima-media thickness is a known subclinical radiologic marker of the early manifestations of atherosclerotic disease. It is the thickness of the vessel wall, most often the carotid artery. Intima-media thickness is measured on conventional US manually or automatically. Other measurement techniques include radiofrequency US. Because there is variation in its measurement, especially in children, several recommendations have been set to increase the measurement’s validity and comparability among studies. Despite these recommendations, several pitfalls should be avoided, and quality control should be performed to avoid erroneous interpretation. This article summarizes current literature in relation to the clinical applications for intima-media thickness measurement in children with known risk factors such as obesity, liver steatosis, hypercholesterolemia, diabetes, hypertension, systemic inflammatory diseases, cancer survival, kidney and liver transplant, and sickle cell disease or beta thalassemia major. Most potential indications for intima-media thickness measurement remain in the research domain and should be interpreted combined with other markers. The objective of diagnosing an increased intima-media thickness is to start a multidisciplinary treatment approach to prevent disease progression and its sequelae in adulthood.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
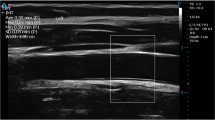
The need for a noninvasive, safe diagnostic test to detect early subclinical changes in vessel walls is of utmost clinical importance for risk stratification in children with known risk factors for early atherosclerotic disease. In relation to pediatric applications of intima-media thickness measurement, the US-based technique lacks abiding by standardization and validation guidelines. Risk factors for atherosclerosis begin in childhood. Obesity is linked to atherosclerosis, dyslipidemia and insulin resistance [1]. Several studies have shown vascular changes and fat streaks deposition in vessel walls of children and young adults who are otherwise asymptomatic [1, 2]. The process starts with abnormal vascular wall vasodilatation secondary to fat deposition, which leads to further abnormal vasomotion, vascular wall smooth muscle hyperplasia, intima-media thickening and ultimately the development of atherosclerotic plaques in late adulthood [3]. Intima-media thickness is defined as the distance between the interface lumen-intima and the interface media-adventitia (Fig. 1).
Common carotid artery in a healthy 12-year-old boy. a, b Longitudinal US images show the different layers (a) and the lumen-intima (long arrow) and media-adventitia (short arrow) interfaces delineating the intima-media thickness (b). The intima-media thickness is measured as the distance between the lumen-intima interface and the media-adventitia interface (lines)
Obese children tend to remain obese as adults [4]. Several cohorts have shown an association between risk factors for atherosclerosis and intima-media thickness [2, 5]. Obese children have increased intima-media thickness and diminished vascular wall elasticity [6, 7]. Mortality and morbidity from atherosclerotic disease is prevalent in adults. However, studies in young adults have shown progression of intima-media thickening in time with the prevalence of risk factors [8]. In a meta-analysis, Lorenz et al. [9] found that the association between risk factors and increased intima-media thickness becomes linear when the intima-media thickness is significantly increased. This indicates the need to start treatment and prevention early to avoid disease progression and further sequelae in adulthood. Intima-media thickness measured by B-mode has been shown to be a definite surrogate marker for atherosclerosis [10]. Measuring intima-media thickness could help in the early identification and stratification of at-risk individuals, and it could be used to carefully follow the impact of disease interventions, including lifestyle changes or medication. Most potential indications for intima-media thickness measurement remain in the research domain and should be interpreted in combination with other markers. This article reviews the guidelines for standardized intima-media measurement on US in children and briefly summarizes the current literature on potential clinical indications in children.
Intima-media thickness measurement techniques
Intima-media thickness is measured according to guidelines set forth by the Mannheim [11], the Association for European Paediatric Cardiology [12], the American Heart Association [13] and the American Society of Echocardiography Carotid Intima-Media Thickness Task Force [14]. The aim of these guidelines is to standardize intima-media thickness measurement to improve reproducibility and comparability of the measurements in time and among different cohorts. These consortiums recommend measuring the common carotid artery bilaterally at more than 5 mm of the carotid bifurcation on the far wall of the vessel relative to the US probe [11,12,13,14]. The patient should be in a supine position, head tilted 45° to the opposite side. Several measurements with different insonation angles and during diastole are preferred [11]. A linear 7–14-MHz probe placed longitudinally along the vessel is used and the measurement is taken after a 10-min rest. The focus should be about 30–40 mm, frame rate of at least 25 Hz with a gain of 60 dB [11,12,13]. The measurement is reported on each side and the average of both sides could be given. Measurements are done on conventional B-mode US using calipers to manually measure the distance between the two interfaces or using special software to get an automated measurement. The latter is more robust because it reflects the average measurements along a segment of the vessel wall rather than between just two points [12]. The software usually gives the standard deviation and the minimal and maximal intima-media thickness values along the segment. Manual techniques have demonstrated more inter- and intraobserver variability because of the difficulty in manually placing the calipers given that the measurement is usually less than half a millimeter [12]. Several studies have shown good agreement between the techniques in healthy adults but less so in children and adolescents, probably because of children’s inherently smaller intima-media thickness [15].
The other technique used is radiofrequency US, which basically uses the raw US data to localize the two interfaces and hence theoretically gives a more accurate measurement along a segment of the artery wall and hence is automatic and more robust. Specifying which technique was used is important because these measurements are not always interchangeable in children [7, 15]. Omitting to do so could lead to erroneous interpretation of the measurement because normative charts depend on the age and gender of the child and the technique used, either in B-mode, radiofrequency, manual or automatic. As for calibration, the Association for European Paediatric Cardiology recommended a rate of interobserver variability of 0.055 mm; a 10-patient sample for quality control; and a coefficient of variation of 6%, defined as standard deviation divided by the mean [12]. The consensuses recommended to always measure the artery diameter in correlation to the intima-media thickness [11,12,13,14]. The American Heart Association described three potential further research avenues to better understand intima-media thickness: (1) longitudinal cohorts to determine normal intima-media thickness values in children according to age, gender and race; (2) longitudinal studies to determine the impact of increased intima-media thickness on mortality and morbidity in adulthood and the threshold of age, weight and body mass index at which the intima-media thickness becomes most reproducible and accurate; and (3) the cost effectiveness of measuring intima-media thickness [13].
This brings us to the fact that there are less normative tables in the literature in the pediatric population compared to adults. The Association for European Paediatric Cardiology mentioned that the available cohorts are relatively small (smaller than 100 patients) [12]. Therefore, the impact of intima-media thickening on mortality and morbidity in adulthood cannot be determined without more longitudinal studies. Doyon et al. [16] published a multicentric study about the normative intima-media thickness in children ages 6–18 years using manual and semi-automated techniques on B-mode US. He found that intima-media thickness increases with age, height, body mass index and blood pressure. Therefore, intima-media thickness values should not be interpreted independently from these factors. Gender difference was detected for children ages 15 years and older, with intima-media thickness being increased in boys. Several other cohorts in the literature used B-mode techniques manually or semi-automatically (Table 1) [16,17,18,19,20,21,22,23,24,25,26,27,28]. A recent meta-analysis by Torkar et al. [28] reported normative values for intima-media thickness in children. Their measurements were comparable to the literature. However, one study compared B-mode-based and radiofrequency-based intima-media thickness measurements on the same cohort of children and found poor correlation [15]. In contradistinction, in adults there is good correlation between the B-mode and radiofrequency techniques [29]. In our practice, we use the semi-automated technique on B-mode images to measure intima-media thickness together with a radiofrequency-based video loop sequence of at least five cardiac cycles. This video sequence is then analyzed by our collaborators on a noninvasive vascular elastography software (Object Research Systems [ORS] Visual Inc.; Montreal, Canada), that generates intima-media thickness based on radiofrequency as well as elastography parameters including the axial strain, translation, shear strain and the lateral translation [7]. We always include a control group in evaluating intima-media thickness in research settings.
Important patient characteristics to be included in any intima-media thickness assessment are therefore age, sexual maturation (Tanner stage), height, weight, body mass index, waist circumference, and systolic, diastolic and pulse pressure. Other anthropometric measures to help better stratify risk for early atherosclerosis could include skin fold thickness, hip circumference and calf circumference. In this perspective, it is to note that physiological change in the intima-media thickness in children related to age, gender and sexual maturity is not well-known and that these anthropometric measures could likely indicate a physiological increase in the intima-media thickness. Therefore, the threshold above which the intima-media thickness becomes abnormally increased in children has not been determined. This is in keeping with the recent publication of Chiesa et al. [30], who suggested that changes in intima-media thickness could be physiological and not necessarily indicate early atherosclerosis. Baroncini et al. [24] did not find a difference in intima-media thickness between healthy males and females. However, in their recent systematic literature review, Torkar et al. [28] found that intima-media thickness is lower in girls and increases with age, height and hip circumference in both girls and boys. Although intima-media thickness increases with age in adults [31], the results are more heterogeneous in children. Several studies did not find a relationship between intima-media thickness and age in children [17, 25, 26]; others found a weak one [18]. Calabrò et al. [25] found a weak correlation between intima-media thickness and height in boys. Jourdan et al. [18] also found a correlation between height and intima-media thickness. In summary, literature suggests accounting for these factors in interpreting intima-media thickness in children.
How to measure a reliable intima-media thickness
Despite recommendations and specific criteria to measure intima-media thickness, there are several important aspects to avoiding erroneous measurements.
For the manual technique, placing the calipers can be tricky; for this reason, taking several measurements manually and reporting the average increases the validity of the measurement (Fig. 2). As for the semi-automated (Fig. 3) and automated techniques (Fig. 4), several studies reported good interobserver and intraobserver agreement [32,33,34,35,36,37]. The advantage of the semi-automated technique stems from the fact that the measurement is an average over a segment of the vessel wall, which theoretically is more robust and reliable than a single measurement over a specific point of the vessel wall. The software usually gives the minimal, maximal and average values together with the standard deviation, hinting to the quality of the mean reported measurement. The software could measure the near wall of the vessel, which is against standards. Usually, it is recommended for the semi-automated and the automated techniques to measure the intima-media thickness over a 1-cm segment of the vessel wall, usually the carotid artery. However, sometimes the application fails to detect the edges and a narrower segment enables the application to generate a less robust measurement. The quality index in some softwares (e.g., M’Ath software, Argenteuil, France) should be at least 50%, indicating that the software used at least half of the measurement for the intima-media thickness to calculate the given average. This index is important in keeping with the advantage of the semi-automated technique over the manual technique (Fig. 5). However, edge detection could be a problem and operators should be aware of the possible misregistration of the edge delineating the intima-media complex (Fig. 6).
Manual measurement. Longitudinal B-mode US image of the common carotid artery in a healthy 16-year-old boy obtained during diastole (R wave) on a Vivid E9 US system (GE Healthcare, Chicago, IL). Two echogenic (bright) lines, representing the lumen-intima interface and the media-adventitia interface (intima-media complex), are identified; the shortest perpendicular distance between them is measured with calipers. Usually, 3 to 10 such measurements are obtained to increase measurement reliability and for interobserver variability studies
Semi-automated measurement. Longitudinal B-mode US image using a semi-automated measurement technique of the intima-media thickness in a 12-year-old overweight boy (body mass index at 88th percentile) using M’Ath SR software version 3.2.1 (Argenteuil, France) connected to a Aplio XG US machine (Toshiba, British Columbia, Canada) and a 14-MHz linear probe. A 1-cm green line is drawn by the operator next to the lumen-intima interface. The software then measures the mean thickness over that segment with a minimum and maximum value and standard deviation. A quality index of at least 0.5 means that the software accounted for at least 50% of the measurement in the calculation of the mean intima-media thickness over the segment in question. This reflects a robust measurement if the edge detection lines are adequately generated
Automated measurement. Longitudinal B-mode US image using an automated measurement technique for the intima-media thickness of the same boy as in Fig. 3, measured using a Smart 3300 US machine (Terason, Burlington, MA) and a linear 15L4A probe. The box is 1 cm long and automatically gives the mean, minimum and maximum values of the intima-media thickness, as shown
Measurement index. Longitudinal B-mode US image using a semi-automated measurement technique for the intima-media thickness in a healthy 12-year-old girl. Image shows edge detection lines shorter than the green line indicated by the operator. This reflects a poorer measurement because the quality index would be small, indicating that the mean measurement reflects intima-media thickness over a shorter segment. The yellow line and magenta line are generated through edge detection analysis by the software and indicate the lumen-intima interface and the media-adventitia interface, respectively
Erroneous edge detection. Longitudinal B-mode US image using a semi-automated measurement technique for the intima-media thickness of the same 12-year-old girl as in Fig. 5 shows erroneous edge detection by the software, leading to misinterpretation of the intima-media thickness. The green line drawn by the operator next to the lumen-intima interface indicates to the software the arterial segment to be analyzed for intima-media thickness. The yellow line and magenta line are generated through edge detection analysis by the software and should theoretically indicate the lumen-intima interface and the media-adventitia interface, respectively
Calibration is another important aspect of these measurements, especially for software that is not integrated in the US machine [12]. This is usually done by measuring a known segment three times and recording the known length in the calibration procedure.
The intraobserver and interobserver agreement depends on the technique used and ranges between an interclass correlation coefficient of 0.84 to 0.93 and 0.7 to 0.8, respectively, according to a meta-analysis [28]. Although the left common carotid artery is reported to show increased intima-media thickness with respect to the right side [38], results are more heterogeneous in adults [39]. In children, a single-side intima-media thickness is sufficient to detect age- and gender-related intima-media thickness [19].
Optimal resolution in diastole and measurement during R wave using electrocardiography (ECG) do not correlate well in children, and hence the same technique should be used to compare groups, cohorts and follow-up measurements [21]. This important finding could explain the discordance between the B-mode and the radiofrequency techniques, with the latter being automated and always measured during diastole (Fig. 7). As to the segment of the carotid artery at which intima-media thickness is measured, Weberruß et al. [40] did not find any difference in the intima-media thickness.
Automated calculations during diastole. Longitudinal US image using an automated radiofrequency-based measurement technique for the intima-media thickness in a 12-year-old boy. Images were obtained with a linear-array L10–5 40-mm US transducer (model 410.503) on the MyLab 70 platform (Esaote, Genoa, Italy) equipped with an ART.LAB platform (Pie Medical Imaging BV, Maastricht, The Netherlands). The software automatically calculates intima-media thickness across the cardiac cycles during diastole (values on the left of the US image)
Clinical indications
According to the consensuses, intima-media thickness measurement should start early on and be part of the overall assessment of risk for early atherosclerosis. Although it is of benefit in these clinical situations, intima-media thickness interpretation outside the research domain is still limited. Clinical indications include obesity, non-alcoholic fatty liver disease, sickle cell disease, prematurity, transplant and inflammatory bowel disease, among others.
Obesity and the metabolic syndrome
This is the main indication for assessing the intima-media thickness. Obese children have increased intima-media thickness [7]. The relationship between intima-media thickness and risk factors becomes linear when the intima-media thickness is significantly increased [9]. This increased intima-media thickness related to obesity in children is independent of the technique used [15]. The Bogalusa Heart Study showed a linear relationship between obesity in childhood and intima-media thickness of the carotid artery in adulthood [2, 5]. Children with even more increased body mass index and those who remain obese for a longer period tend to have the most increased intima-media thickness [13]. However, other studies did not find a correlation between intima-media thickness and body mass index in healthy children and adolescents [24]. A meta-analysis done in 2015 reported a rate of 68% of published articles confirming the relationship between increased intima-media thickness and obesity in adolescents [41]. In this perspective, the International Childhood Cardiovascular Cohort consortium found that adult metabolic syndrome, diabetes mellitus type 2 and subclinical atherosclerosis as measured by the intima-media thickness could be predicted during childhood as of 5 and 8 years, respectively [42]. Although several studies have demonstrated an increased intima-media thickness with increasing body mass index [6] and abdominal obesity [43], others including a meta-analysis demonstrated a rather stronger relationship between diminished arterial distensibility and obesity [44, 45].
Non-alcoholic fatty liver disease
Non-alcoholic fatty liver disease (NAFLD) is a known independent risk factor for atherosclerosis in children [46]. A meta-analysis in 2015 showed that only five articles evaluated the relationship between NAFLD and intima-media thickness in children. Children with NAFLD had significantly increased intima-media thickness [47, 48]. These changes were seen in children as of 10 years of age [49]. However, the relationship between NAFLD and increased intima-media thickness depends on the certainty with which the diagnosis of NAFLD is made [49]. In a study comparing obesity with and without liver steatosis and controls, intima-media thickness was significantly increased in the group of children who were obese with liver steatosis [50]. In a larger study of 642 children ages 11 to 13, Caserta et al. [51] found an association among increased intima-media thickness, NAFLD and body mass index. In this perspective, not only is intima-media thickness increased but also the left ventricular mass in obese adolescents with NAFLD [52] and epicardial adipose tissue [53]. Beyond the intima-media thickness, arterial stiffness was also found to be altered in obese children with liver steatosis [54, 55]. This relationship is not always demonstrated; in their small study of 78 obese children, Koot et al. [56] did not find a relationship between liver steatosis and increased intima-media thickness.
Sickle cell disease
Children with sickle cell disease have increased intima-media thickness. The pathophysiology of vascular disease in sickle cell disease is complex and multifactorial. This is in part because of increased endothelial damage secondary to the adherence of deformed and aggregated red blood cells, chronic inflammation and increased platelet activation, as well as alteration in the bioavailability of vasoactive agents including nitric oxide. Chronic hemolysis and, in some people, development of iron overload, might also contribute to the vascular damage, wall hyperplasia and increased intima-media thickness. While pathophysiology of other hemoglobinopathy might differ, increased intima-media thickness has been well-described in people with thalassemia major. Cystatin C, a biomarker of kidney function, is also a subclinical biomarker of cardiovascular disease. Cystatin C level has been correlated with increased intima-media thickness in children with sickle cell disease [57]. In the same perspective, intima-media thickness of the common femoral artery was significantly increased with the presence of leg ulcers, reflecting vasculopathy in people with sickle cell disease [58].
Prematurity
Studies in children and in young adults born prematurely did not all show an increased intima-media thickness in that population, although elasticity was altered [59, 60]. The literature review in this perspective focused on the need to correlate increased intima-media thickness with body habitus and the carotid artery diameter. The explanation for this finding could be the pathophysiology behind the increased cardiovascular risk in this population. In fact, the only variable associated with altered cardiovascular compliance was the presence of bronchopulmonary dysplasia [60]. Similarly, small-for-gestational-age children have increased intima-media thickness, according to some studies. The mechanism is, however, to be determined because rapid growth catch-up has been elucidated as an underlying cause [61].
Transplant patients
In a study examining intima-media thickness in children with renal and liver transplants, intima-media thickness was increased in the renal transplant group compared to both the liver transplant and control groups [62]. However, in liver transplant children, intima-media thickness was associated with the more prevailing risk factors in this population, namely increased diastolic blood pressure and glucose intolerance [63]. Children with liver transplant have also been shown to demonstrate increased intima-media thickness [64]. Sirolimus, a mechanistic target of rapamycin (mTOR) inhibitor and an immunosuppressor drug used in renal transplantation, has been described to cause dyslipidemia. However, children on sirolimus had decreased intima-media thickness [65], suggesting a complex mechanism that needs further evaluation [66]. Similarly, pediatric heart transplant recipients show increased intima-media thickness [67]. Further studies are needed to clarify this drug-related effect in transplant children.
Inflammatory bowel disease patients
Despite their lower body mass index, children with inflammatory bowel disease were found to have increased intima-media thickness compared to controls [68]. This could stem from the fact that there is endothelial dysfunction as seen by an altered-flow-mediated vasodilatation in these children [69]. Another study demonstrated the same finding, although for the aortic intima-media thickness [70]. The same findings were noted in young adults with early rheumatoid arthritis [71].
Other clinical indications
Significant intima-media thickness increase was noted in children with familial hypercholesterolemia as early as 8 years of age [72].
The PositHIVe Health Study demonstrated an increased intima-media thickness in adolescents with human immunodeficiency virus (HIV) infection [73]. Poor dental hygiene was also correlated with increased intima-media thickness [74]. Dietz et al. [75] found an increased intima-media thickness in children with history of Kawasaki disease and coronary artery aneurysm. Children with beta-thalassemia major also have increased intima-media thickness, reflecting their increased risk for early atherosclerosis [76]. Children with chronic renal disease have increased intima-media thickness, indicating increased risk for atherosclerosis [77]. Intima-media thickness is also increased in children with hypertension [78] and type 1 diabetes [79]. Children with congenital adrenal hyperplasia might show altered intima-media thickness [80, 81]. Because of systemic inflammation and endothelial dysfunction, children with juvenile idiopathic arthritis could benefit from intima-media thickness assessment [82]. Similarly, children with rheumatic heart disease are predisposed to early atherosclerosis and could benefit from intima-media thickness assessment [83]. Finally, intima-media thickness is increased in young adults with a history of childhood cancer, especially following radiation therapy [84]. It should be noted, however, that the pathophysiology behind intima-media thickness might not be the same for all of these diseases and that atherosclerosis is not the only culprit [57, 59, 60, 64, 65, 67, 80,81,82,83,84,85].
Clinical significance
Because intima-media thickness is a subclinical marker of atherosclerosis, disease progression could theoretically be altered if a multidisciplinary treatment approach were initiated, which is the main reason intima-media thickness should be assessed in children. Longitudinal studies have demonstrated obesity-related increased risk for cardiovascular diseases in adulthood. Although longitudinal studies looking at the impact of intima-media thickness specifically on mortality and morbidity are lacking in the pediatric literature, measurement of the intima-media thickness remains a promising subclinical noninvasive and safe marker for early atherosclerosis based on US. The Bogalusa heart and cardiovascular risk study in young Finns showed a decrease in intima-media thickness following resolution of childhood metabolic syndromes [86]. Lifestyle intervention and sometimes medications for obese adolescents could change the risk [87, 88]. In this perspective, the American Heart Association (AHA) Expert Panel on Population and Prevention Science and the AHA’s Cardiovascular Disease in the Young Council; Epidemiology and Prevention Council; Nutrition, Physical Activity and Metabolism Council; High Blood Pressure Research Council; Cardiovascular Nursing Council; Kidney in Heart Disease Council; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research, in a scientific statement, stratified the risk and set guidelines to prevent disease progression. This statement was endorsed by the American Academy of Pediatrics [89].
Conclusion
Intima-media thickness measurement should be done according to the guidelines set by the major consensuses to increase reproducibility, comparability and clinical utility between cohorts and in time. The technique used should be explicitly mentioned in order to standardize measurement interpretation. In children, the techniques could not be interchangeable, and a technique-specific normative chart should be used according to age and body habitus. Intima-media thickness measurement should be interpreted in the context of other clinical markers and should be performed early for the stated potential clinical indications.
References
McGill HC Jr, McMahan CA, Zieske AW et al (2000) Associations of coronary heart disease risk factors with the intermediate lesion of atherosclerosis in youth. The Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. Arterioscler Thromb Vasc Biol 20:1998–2004
Raitakari OT, Juonala M, Rönnemaa T et al (2008) Cohort profile: the cardiovascular risk in young Finns study. Int J Epidemiol 37:1220–1226
Lim HS, Lip GYH (2008) Arterial stiffness: beyond pulse wave velocity and its measurement. J Hum Hypertens 22:656–658
Baker JL, Olsen LW, Sørensen TIA (2007) Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med 357:2329–2337
Freeman DS, Dietz WH, Tang R et al (2004) The relation of obesity throughout life to carotid intima-media thickness in adulthood: the Bogalusa Heart Study. Int J Obes Relat Metab Disord 28:159–166
Ozcetin M, Celikyay ZRY, Celik A et al (2012) The importance of carotid artery stiffness and increased intima-media thickness in obese children. S Afr Med J 102:295–299
El Jalbout R, Cloutier G, Roy-Cardinal MH et al (2019) The value of non-invasive vascular elastography (NIVE) is detecting early vascular changes in overweight and obese children. Eur Radiol 29:3854–3861
Srinivasan SR, Bao W, Wattigney WA, Berenson GS (1996) Adolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors: the Bogalusa Heart Study. Metabolism 45:235–240
Lorenz MW, Markus HS, Bots ML et al (2007) Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation 115:459–467
De Groot E, Hovingh GK, Wiegman A et al (2004) Measurement of arterial wall thickness as a surrogate marker for atherosclerosis. Circulation 109:III33–38
Touboul PJ, Hennerici MG, Meairs S et al (2012) Mannheim carotid intima-media thickness and plaque consensus (2004–2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis 34:290–296
DallaPozza R, Ehringer-Schetitska D, Fritsch P et al (2015) Intima media thickness measurement in children: a statement from the Association for European Paediatric Cardiology (AEPC) Working Group on Cardiovascular Prevention endorsed by the Association for European Paediatric Cardiology. Atherosclerosis 238:380–387
Urbina EM, Williams RV, Alpert BS et al (2009) Noninvasive assessment of subclinical atherosclerosis in children and adolescents: recommendations for standard assessment for clinical research: a scientific statement from the American Heart Association. Hypertension 54:919–950
Stein JH, Korcarz CE, Hurst RT et al (2008) Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. J Am Soc Echocardiogr 21:93–111
El Jalbout R, Cloutier G, Roy-Cardinal MH et al (2018) Carotid artery intima media thickness measurement in children with normal and increased BMI: a comparison of three techniques. Pediatr Radiol J 48:1073–1079
Doyon A, Kracht D, Bayazit AK et al (2013) Carotid artery intima-media thickness and distensibility in children and adolescents: reference values and role of body dimensions. Hypertension 62:550–556
Sass C, Herbeth B, Chapet O et al (1998) Intima-media thickness and diameter of carotid and femoral arteries in children, adolescents and adults from the Stanislas cohort: effect of age, sex, anthropometry and blood pressure. J Hypertens 16:1593–1602
Jourdan C, Wühl E, Litwin M et al (2005) Normative values for intima-media thickness and distensibility of large arteries in healthy adolescents. J Hypertens 23:1707–1715
Böhm B, Hartmann K, Buck M, Oberhoffer R (2009) Sex differences of carotid intima-media thickness in healthy children and adolescents. Atherosclerosis 206:458–463
Engelen L, Ferreira I, Stehouwer CD et al (2013) Reference intervals for common carotid intima-media thickness measured with echotracking: relation with risk factors. Eur Heart J 34:2368–2380
Selamet Tierney ES, Gauvreau K, Jaff MR et al (2015) Carotid artery intima-media thickness measurements in the youth: reproducibility and technical considerations. J Am Soc Echocardiogr 28:309–316
Prats-Puig A, Moreno M, Carreras-Badosa G et al (2016) Serum ferritin relates to carotid intima-media thickness in offspring of fathers with higher serum ferritin levels. Arterioscler Thromb Vasc Biol 36:174–180
DallaPozza R, Pirzer R, Beyerlein A et al (2016) Beyond intima-media-thickness: analysis of the carotid intima-media-roughness in a paediatric population. Atherosclerosis 251:164–169
Baroncini LAV, de Castro Sylvestre L, Pecoits Filho R (2016) Assessment of intima-media thickness in healthy children aged 1 to 15 years. Arq Bras Cardiol 106:327–332
Calabrò MP, Carerj S, Russo MS et al (2017) Carotid artery intima-media thickness and stiffness index β changes in normal children: role of age, height and sex. J Cardiovasc Med 18:19–27
Gooty VD, Sinaiko AR, Ryder JR et al (2018) Association between carotid intima media thickness, age, and cardiovascular risk factors in children and adolescents. Metab Syndr Relat Disord 16:122–126
Bassols J, Martínez-Calcerrada JM, Prats-Puig A et al (2018) Perirenal fat is related to carotid intima-media thickness in children. Int J Obes 42:641–647
Torkar AD, Plesnik E, Groselj U et al (2020) Carotid intima-media thickness in healthy children and adolescents: normative data and systematic literature review. Front Cardiovasc Med 7:597768
Schreuder FH, Graf M, Hameleers JM et al (2009) Measurement of common carotid artery intima media thickness in clinical practice: comparison of B-mode and RF-based technique. Ultraschall Med 30:459–465
Chiesa ST, Charakida M, Georgiopoulos G et al (2021) Determinants of intima-media thickness in the young: the ALSPAC Study. JACC Cardiovasc Imaging 14:468–478
Buljan K, Soldo SB, Janculjak D et al (2015) Relationship between age and thickness of carotid arteries in a population without risk factors for atherosclerosis. Coll Antropol 39:779–784
Mac Ananey O, Mellotte G, Maher V (2014) Comparison of semi-automated and manual measurements of carotid intima-media thickening. Biomed Res Int 2014:531389
Vilas Freire CM, Pinho Ribeiro AL, Lima Barbosa FB et al (2009) Comparison between automated and manual measurements of carotid intima-media thickness in clinical practice. Vasc Health Risk Manag 5:811–817
Xiao L, Li Q, Bai Y et al (2015) Automated measurement method of common carotid artery intima-media thickness in ultrasound image based on Markov random field models. J Med Biol Eng 35:651–660
Molinari F, Meiburger KM, Zeng G et al (2012) Automated carotid IMT measurement and its validation in low contrast ultrasound database of 885 patient Indian population epidemiological study: results of AtheroEdge software. Int Angiol 31:42–53
Naik V, Gamad RS, Bansod PP (2013) Carotid artery segmentation in ultrasound images and measurement of intima-media thickness. Biomed Res Int 2013:801962
Loizou CP (2014) A review of ultrasound common carotid artery image and video segmentation techniques. Med Biol Eng Comput 52:1073–1093
Foerch C, Buehler A, von Kegler S, Sitzer M (2003) Intima media thickness side differences are limited to the common carotid artery. Hypertension 42:e17
Loizou CP, Nicolaides A, Kyriacou E et al (2015) A comparison of ultrasound intima-media thickness measurements of the left and right common carotid artery. IEEE J Transl Eng Health Med 3:1900410
Weberruß H, Pirzer R, Dalla Pozza R et al (2016) Intima-media thickness does not differ between two common carotid artery segments in children. PLoS One 11:e0149057
Park MH, Skow A, De Matteis S et al (2015) Adiposity and carotid-intima media thickness in children and adolescents: a systematic review. BMC Pediatr 15:161
Koskinen J, Magnussen CG, Sinaiko A et al (2017) Childhood age and associations between childhood metabolic syndrome and adult risk for metabolic syndrome, type 2 diabetes mellitus and carotid intima media thickness: the International Childhood Cardiovascular Cohort Consortium. J Am Heart Assoc 6:e005632
Hochamdioglu B, Okutan V, Yozgat Y et al (2011) Abdominal obesity is an independent risk factor for increased carotid intima-media thickness in obese children. Turk J Pediatr 53:48–54
Weberruß H, Pirzer R, Böhm B et al (2016) Intima-media thickness and arterial function in obese and non-obese children. BMC Obes 3:2
Cote AT, Phillips AA, Harris KC et al (2015) Obesity and arterial stiffness in children: systematic review and meta-analysis. Arterioscler Thromb Vasc Biol 35:1038–1044
Pacifico L, Perla FM, Roggini M et al (2019) A systematic review of NAFLD-associated extrahepatic disorders in youths. J Clin Med 8:868
Cai J, Zhang S, Huang W (2015) Association between nonalcoholic fatty liver disease and carotid atherosclerosis: a meta-analysis. Int J Clin Exp Med 8:7673–7678
Madan SA, John F, Pyrsopoulos N, Pitchumoni CS (2015) Nonalcoholic fatty liver disease and carotid artery atherosclerosis in children and adults: a meta-analysis. Eur J Gastroenterol Hepatol 27:1237–1248
Karjoo S (2018) Is there an association of vascular disease and atherosclerosis in children and adolescents with obesity and non-alcoholic fatty liver disease? Front Pediatr 6:345
Pacifico L, Cantisani V, Ricci P et al (2008) Nonalcoholic fatty liver disease and carotid atherosclerosis in children. Pediatr Res 63:423–427
Caserta CA, Pendino GM, Amante A (2010) Cardiovascular risk factors, nonalcoholic fatty liver disease, and carotid artery intima-media thickness in an adolescent population in southern Italy. Am J Epidemiol 171:1195–1202
Sert A, Pirgon O, Aypar E et al (2012) Relationship between left ventricular mass and carotid intima media thickness in obese adolescents with non-alcoholic fatty liver disease. J Pediatr Endocrinol Metab 25:927–934
Alp H, Karaarslan S, Eklioğlu BS et al (2013) Association between nonalcoholic fatty liver disease and cardiovascular risk in obese children and adolescents. Can J Cardiol 29:1118–1125
Lee YJ, Shim JY, Moon BS et al (2012) The relationship between arterial stiffness and nonalcoholic fatty liver disease. Dig Dis Sci 57:196–203
Kim BJ, Kim NH, Kim BS, Kang JH (2012) The association between nonalcoholic fatty liver disease, metabolic syndrome and arterial stiffness in nondiabetic, nonhypertensive individuals. Cardiology 123:54–61
Koot BGP, de Groot E, van der Baan-Slootweg OH et al (2015) Nonalcoholic fatty liver disease and cardiovascular risk in children with obesity. Obesity 23:1239–1243
Gawad Tantawy AA, MoneamAdly AA, Rahman Ismail EA, Abdelazeem M (2017) Clinical predictive value of cystatin C in pediatric sickle cell disease: a marker of disease severity and subclinical cardiovascular dysfunction. Clin Appl Thromb Hemost 23:1010–1017
Ayoola OO, Bolarinwa RA, Onakpoya UU et al (2018) Intima-media thickness of the common femoral artery as a marker of leg ulceration in sickle cell disease patients. Blood Adv 2:3112–3117
Flahault A, Paquette K, Fernandes RO et al (2020) Increased incidence but lack of association between cardiovascular risk factors in adults born preterm. Hypertension 75:796–805
Flahault A, Oliveira Fernandes R, De Meulemeester J et al (2020) Arterial structure and stiffness are altered in young adults born preterm. Arterioscler Thromb Vasc Biol 40:2548–2556
Faienza MF, Brunetti G, Delvecchio M et al (2016) Vascular function and myocardial performance indices in children born small for gestational age. Circ J 80:958–963
Siirtola A, Kallio T, Ala-Houhala M et al (2010) Carotid intima-media thickness after pediatric renal or liver transplantation at high-resolution B-mode ultrasonography. Transplant Proc 42:1695–1698
Perito ER, Phelps A, Vase T et al (2018) Subclinical atherosclerosis in pediatric liver transplant recipients: carotid and aorta intima-media thickness and their predictors. J Pediatr 193:119-127.e1
Naeser V, Brandt AH, Nyhuus B et al (2018) Risk markers for later cardiovascular diseases in liver-transplanted children and adolescents. Pediatr Transplant 22:e13298
Silva AL, Fusco DR, Nga HS et al (2018) Effect of sirolimus on carotid atherosclerosis in kidney transplant recipients: data derived from a prospective randomized controlled trial. Clin Kidney J 11:846–852
McKenna GJ, Trotter JF, Klintmalm E et al (2013) Sirolimus and cardiovascular disease risk in liver transplantation 95:215–221
Duncombe SL Hosking MCK, Coté AT et al (2018) Intimal thickening at coronary bifurcations in pediatric heart transplant recipients. Pediatr Transplant 22:e13100
Aloi M, Tromba L, Di Nardo G et al (2012) Premature subclinical atherosclerosis in pediatric inflammatory bowel disease. J Pediatr 161:589-594.e1
Principi M, Mastrolonardo M, Scicchitano P et al (2013) Endothelial function and cardiovascular risk in active inflammatory bowel diseases. J Crohns Colitis 7:e427–e433
Aloi M, Tromba L, Rizzo V et al (2015) Aortic intima-media thickness as an early marker of atherosclerosis in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 61:41–46
Adhikari MC, Guin A, Chakraborty S et al (2012) Subclinical atherosclerosis and endothelial dysfunction in patients with early rheumatoid arthritis as evidenced by measurement of carotid intima-media thickness and flow-mediated vasodilatation: an observational study. Semin Arthritis Rheum 41:669–675
Kusters DM, Wiegman A, Kastelein JJP, Hutten BA (2014) Carotid intima-media thickness in children with familial hypercholesterolemia. Circ Res 114:307–310
Augustemak de Lima LR, Petroski EL, Franco Moreno YM et al (2018) Dyslipidemia, chronic inflammation, and subclinical atherosclerosis in children and adolescents infected with HIV: the PositHIVe Health Study. PLoS One 13:e0190785
Uyar HS, Akpinar MB, Sahin V et al (2013) Carotid and popliteal artery intima-media thickness in patients with poor oral hygiene and the association with acute-phase reactants. Cardiovasc J Afr 24:308–312
Dietz SM, Tacke CE, Gort J et al (2015) Carotid intima-media thickness in patients with a history of Kawasaki disease. Circ J 79:2682–2687
Gursel O, Kurekci AE, Tascilar E et al (2012) Premature atherosclerosis in children with β-thalassemia major. J Pediatr Hematol Oncol 34:630–634
Khandelwal P, Murugan V, Hari S et al (2016) Dyslipidemia, carotid intima-media thickness and endothelial dysfunction in children with chronic kidney disease. Pediatr Nephrol 31:1313–1320
Lande MB, Carson NL, Roy J, Meagher CC (2006) Effects of childhood primary hypertension on carotid intima media thickness: a matched controlled study. Hypertension 48:40–44
Fusaro MFGS, Zanini JLSS, Silva IN (2016) Increased carotid intima-media thickness in Brazilian adolescents with type 1 diabetes mellitus. Diabetol Metab Syndr 8:74
Farghaly HS, Metwalley KA, Raafat DM et al (2021) Association between vascular endothelial dysfunction and the inflammatory marker neopterin in patients with classic congenital adrenal hyperplasia. Atherosclerosis 328:38–43
Metwalley KA, Farghaly HS, Abdelhamid A et al (2018) Homocysteine level in children with classic congenital adrenal hyperplasia: relationship to carotid intimal wall thickness and left ventricular function. Horm Res Paediatr 90:228–235
Del Giudice E, Dilillo A, Tromba L et al (2018) Aortic, carotid intima-media thickness and flow-mediated dilation as markers of early atherosclerosis in a cohort of pediatric patients with rheumatic diseases. Clin Rheumatol 37:1675–1682
Satija M, Yaday TP, Sachdev N et al (2014) Endothelial function, arterial wall mechanics and intima media thickness in juvenile idiopathic arthritis. Clin Exp Rheumatol 32:432–439
Krawczuk-Rybak M, Tomczuk-Ostapczuk M, Panasiuk A, Goscik E (2017) Carotid intima-media thickness in young survivors of childhood cancer. J Med Imaging Radiat Oncol 61:85–92
Aggoun Y, Sidi D, Levy BI et al (2000) Mechanical properties of the common carotid artery in Williams syndrome. Heart 84:290–293
Magnussen CG, Koskinen J, Juonala M et al (2012) A diagnosis of the metabolic syndrome in youth that resolves by adult life is associated with a normalization of high carotid intima-media thickness and type 2 diabetes mellitus risk: the Bogalusa heart and cardiovascular risk in young Finns studies. J Am Coll Cardiol 60:1631–1639
Reinehr T (2013) Calculating cardiac risk in obese adolescents before and after onset of lifestyle intervention. Expert Rev Cardiovasc Ther 11:297–306
Masquio DC, de Piano A, Sanches PL et al (2013) The effect of weight loss magnitude on pro-/anti-inflammatory adipokines and carotid intima-media thickness in obese adolescents engaged in interdisciplinary weight loss therapy. Clin Endocrinol 79:55–64
Kavey REW, Allada V, Daniels SR et al (2006) Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association Expert Panel on Population and Prevention Science; the Councils on Cardiovascular Disease in the Young, Epidemiology and Prevention, Nutrition, Physical Activity and Metabolism, High Blood Pressure Research, Cardiovascular Nursing, and the Kidney in Heart Disease; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. Circulation 114:2710–2738
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El Jalbout, R., Levy, E., Pastore, Y. et al. Current applications for measuring pediatric intima-media thickness. Pediatr Radiol 52, 1627–1638 (2022). https://doi.org/10.1007/s00247-021-05241-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-05241-2