Abstract
Intravascular ultrasound (IVUS) is used as a diagnostic adjunct to angiography and has become a valuable diagnostic and interventional tool with a well-documented safety profile. The American College of Cardiology and the European Society of Cardiology have published guidelines regarding the use of IVUS in the setting of percutaneous coronary intervention. IVUS has gained popularity in the interventional radiology (IR) community in recent years; however, there are no consensus guidelines for utilization. Furthermore, IVUS remains an infrequently used modality in pediatric IR, likely because of unfamiliarity with the equipment and techniques, as well as concerns over the compatibility of these instruments with pediatric anatomy. IVUS can be safely used as a helpful and sometimes necessary tool for pediatric interventions in appropriately selected patients. The utility of IVUS for reducing both fluoroscopy time and contrast agent volume makes it particularly valuable in pediatric practice. This article presents an overview of both the rotational and phased-array IVUS types and an in-depth discussion on the most common applications of these techniques in the pediatric setting across multiple procedure categories.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intravascular ultrasound (IVUS) was first described as a diagnostic adjunct to coronary angiography [1,2,3]. Intravascular imaging, including IVUS and intracardiac echocardiography), has since proved to be a valuable diagnostic and interventional tool with an established safety profile [4]. Intracardiac echocardiography is a distinct modality referring to the use of endovascular US probes for visualizing cardiac structures. Various endovascular US probes can be used for visualizing intra- and/or extracardiac structures. For the purposes of this discussion, we focus on the extracardiac uses of these probes and use the term “IVUS” to refer to the general concept of imaging with intravascular US catheters including both radial/rotational and phased-array/“side-firing” types (Fig. 1).
The American College of Cardiology (ACC) and the European Society of Cardiology (ESC) have published guidelines regarding the use of IVUS in the setting of percutaneous coronary intervention [5,6,7]. Data support the use of IVUS for coronary interventions with a demonstrated reduction in major adverse events and mortality with its application [8,9,10]. There is also evidence that IVUS-guided peripheral vascular interventions are associated with improved outcomes and comparable overall cost, relative to angiography alone [8, 11]. IVUS utilization is also associated with decreased procedural time, contrast dose and patient radiation exposure [12]. Relative to cardiac interventions, however, data pertaining to the efficacy and safety of IVUS for extracardiac interventions are limited and consist of case reports, small case series and topical reviews.
Intravascular US guidance for the creation of a direct intrahepatic portosystemic shunt (DIPS) was first described in 2001 [13], and the utility and safety of IVUS has been described for extracardiac procedures, including portal interventions (e.g., transjugular intrahepatic portosystemic shunt (TIPS) [14, 15] catheter-directed portal vein thrombolysis [16]), aortic and peripheral arterial interventions [2, 11], venous interventions (e.g. bedside inferior vena cava filter placement [17], stent reconstruction for iliac vein compression syndromes [12], sharp recanalization with total venous reconstructions for iliocaval occlusion [18,19,20]), transbiliary biopsies in people with complex post-surgical anatomy [21] and neurovascular interventions (e.g., cerebral venous sinus stent placement [22], carotid artery stent placement [23]). There is, however, no consensus or standardized guideline for interventional radiologists on the use of IVUS.
While the use of IVUS has become increasingly prevalent in adult interventions [12], it remains an infrequently used modality in the pediatric setting. The reason for low IVUS utilization rates among pediatric interventional radiologists is likely multifactorial. Because IVUS utilization is less common in pediatric IR, it might be difficult for some institutions to justify the cost of the equipment and training necessary to implement IVUS in a meaningful way. Because pediatric-specific safety profiles have not been established, some radiologists might avoid IVUS when risks related to IVUS equipment access (particularly size relative to accessed vessel) subjectively outweigh the benefits of its inclusion. Pediatric interventionalists might be unfamiliar with the equipment, and there might be concerns about the compatibility of the equipment with pediatric anatomy. For this reason, we present a review of the equipment, techniques and potential clinical applications of IVUS for pediatric interventionalists.
Equipment and techniques
Compared to the two-dimensional projection of a vessel provided by conventional angiography, IVUS provides superior anatomical detail with real-time cross-sectional imaging from inside the vessel, which allows for an accurate depiction of the vessel wall and lumen morphology, measurements of vessel dimensions, and guidance for stent placement. It also allows for imaging of adjacent extravascular structures (e.g., other vessels, solid organs), which can provide an invaluable perspective for procedural guidance. Two types of IVUS catheters are available: radial/rotational IVUS catheters and phased-array/“side-firing” IVUS catheters. Several widely available systems are summarized in Table 1. IVUS catheters contain a piezoelectric transducer that produces sound waves. Radial IVUS uses a single-element, rotating piezoelectric transducer. Phased-array IVUS uses a 64-element stationary transducer. In both types of catheters, the transducer is mounted at the end of the catheter [24].
In radial IVUS catheters, a rotating transducer is driven by a flexible drive cable to create cross-sectional images in a 360° radial plane perpendicular to the long axis of the catheter. These transducers operate at higher imaging frequencies and allow for high near-field resolution (up to 6–8 cm), but have more limited depth penetration relative to the phased-array counterparts [24]. Phased-array IVUS consists of a transducer mounted on the end of an 8–10-French steerable catheter. Wedge-shape images, similar to those of conventional US with a curvilinear probe, are produced with a greater depth of penetration (up to 21 cm), allowing for high-quality far-field imaging of adjacent vessels and extravascular structures. In addition to greater depth of penetration, other traditional advantages of phased-array IVUS include increased maneuverability secondary to the steerable nature of the transducer and the ability to acquire color Doppler imaging [24]. While a rotational-type catheter is typically positioned over a guidewire, a phased-array catheter is usually advanced via a vascular sheath positioned in the area of interest.
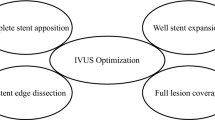
Rotational IVUS allows for a tomographic assessment of the vessel wall and also offers automated pullback, which facilitates accurate measurement of lesion length and selection of an appropriate-size stent [5]. IVUS can identify significant lesions that might be subtle or obscured on planar angiography. Catheters with pulse-tracing capabilities allow for further evaluation of hemodynamic significance. Three-dimensional assessment might reveal areas of extrinsic compression or intraluminal pathology, such as vascular webs, that might be occult on venography [25]. Systems typically offer intraprocedural multi-directional diameter, circumference, and cross-sectional area measurements. IVUS can lead to significantly larger luminal diameter measurements when compared to angiography alone in both pediatric and adolescent patients [26]. Therefore, IVUS usage might allow for more accurate balloon and stent selection (Fig. 2). Conversion of cross-sectional area to cylindrical diameter and stent selection is provided in Table 2. Once the stent is placed, IVUS allows for direct visualization of the stent struts and their relationship to the vessel wall, as well as the radial expansion of the stent. Appropriate stent size is paramount in maintaining stent patency because suboptimal stent wall apposition is a well-documented cause of in-stent thrombosis [12, 27].
Cavernous transformation of the portal vein and splenorenal shunt stenosis in a 2-year-old girl. a Anteroposterior digital subtraction venogram demonstrates severe stenosis at the anastomosis of the splenic and renal veins (arrow). b Rotational intravascular ultrasound (IVUS) shows a patent splenic vein upstream to the splenorenal anastomosis (luminal cross-sectional diameter of 5–5.7 mm was measured prior to selection of an appropriate-size angioplasty balloon). c IVUS image at the anastomosis demonstrates significant luminal narrowing. d Anteroposterior spot image demonstrates inflation of a 5-mm balloon catheter performed across the anastomosis
While rotational IVUS enables precise measurement of lumen size and other vascular characteristics, phased-array IVUS can be used to guide extravascular needle positioning for various procedures with components outside the vessel within which the IVUS catheter resides.
Arterial diseases
Intravascular US guidance can be useful in myriad arterial interventions. At our institution, it has been utilized in the treatment of renovascular hypertension. Percutaneous transluminal renal artery angioplasty can be a safe and effective treatment of pediatric renovascular hypertension in appropriately selected patients [28]. IVUS allows for precise identification of luminal narrowing, and vessel diameter measurements obtained with IVUS are significantly larger when compared to angiography alone [26]. Therefore, IVUS might allow for selection of a more accurate-size angioplasty balloon. Additionally, pulse tracing capabilities might confirm the hemodynamic significance of the lesion prior to treatment (Fig. 3).
Renovascular hypertension in a 16-year-old girl. a Anteroposterior digital subtraction angiogram depicts the area of focal narrowing in the left renal artery (arrow). b Rotational intravascular ultrasound (IVUS) image with transducing element within the angiographic stenosis confirms luminal narrowing to 1.5–2 mm within the left renal artery. c IVUS image demonstrates post-stenotic dilation with cross-sectional measurements of the luminal diameter at 4.8–4.9 mm. d Pulse tracing feature used to obtain spectral Doppler waveforms in the post-stenotic segment of the left renal artery (Eagle Eye; Philips, San Diego, CA). The waveforms show low resistance and delayed systolic upstrokes, consistent with post-stenotic flow dynamics. e, f Despite modest angiographic luminal diameter in the anteroposterior projection following balloon angioplasty (e), completion pulse tracing demonstrates waveform normalization (f)
Venous interventions and vascular compression syndromes
Iliac vein compression syndrome (May–Thurner syndrome)
May–Thurner syndrome is caused by compression of the left common iliac vein between the right common iliac artery and spine with resultant venous congestion and/or deep vein thrombosis (DVT). Researchers have tried to determine the optimal size for iliac venous stents and made recommendations regarding stent sizing for the adult and pediatric populations [25, 29]. Anticipating the “normal” venous caliber, however, is patient-specific and varies depending on patient age, body habitus and other anatomical factors. Therefore, it is important to accurately measure the vessel lumen and choose the appropriate stent size on a case-by-case basis. This requires an accurate assessment of lesion location, length and severity. In the setting of pediatric and adolescent vascular compression syndromes, IVUS provides a more accurate representation of vessel compression and diameter compared to angiography [26]. In one study of 155 limbs with iliofemoral venous stenosis, the authors found that venography, when compared to IVUS, substantially missed significant stenotic lesions, underestimated their severity, and misidentified the location of the iliocaval confluence and distal landing zone [30]. Murray’s law might be used to estimate the expected diameter of daughter vessels based on the parent vessel diameter, and this concept might be applied in iliac vein stenting [31, 32]. This method is dependent on accurate measurement of the parent vessel, which can be done with greater accuracy with IVUS guidance (Fig. 4). Additionally, IVUS assessment of the unaffected common iliac vein can guide optimal stent selection, assuming symmetry. Determining normal venous diameter with anteroposterior projection angiographic measurement of a vein that is compressed in the same axis leads to overestimation of the vessel size, inappropriate stent sizing and associated morbidity (Fig. 5).
Iliac vein compression syndrome post thrombolysis of left lower extremity deep venous thrombosis in an 11-year-old girl. a Anteroposterior (AP) digital subtraction venogram demonstrates effacement of the central left common iliac vein (arrowhead) with collateral outflow (arrows). b, c Rotational intravascular ultrasound (IVUS) positioned at the level of the stenosis of the left common iliac vein (arrow in b; AP projection) provides fluoroscopic demarcation and confirms compression of the left common iliac vein (arrows in c) beneath the aortic bifurcation (L left, R right). d, e AP fluoroscopic image shows repositioning of the catheter to the unaffected segment (arrow in d) assists stent length selection and corresponding IVUS assesses nominal diameter of the common iliac vein (e). f Dual-injection AP iliac venography following placement of the 14 × 60-mm self-expanding bare metal stent confirms both appropriate diameter and cephalad extent (arrows)
Iliac vein compression syndrome in a 16-year-old boy. a Anteroposterior (AP) venogram from the left external iliac vein demonstrates prior stent placement with fluoroscopic guidance alone that resulted in inappropriately large diameter (20-mm) and cephalad extension of a left common iliac vein stent contacting the right lateral wall of the inferior vena cava (IVC) (arrow), resulting in in-stent stenosis (star) and contralateral deep venous thrombosis. b AP dual-injection venogram following reconstruction with bilateral 12-mm stent extending from bilateral external iliac veins (gray arrows) into the IVC in a double-barrel configuration (white arrows) demonstrates re-established normal venous diameter
Intravascular US is frequently used in the management of iliac vein compression syndrome because it allows for assessment of the vessel wall and valves as well as the proximity of adjacent arteries and the degree of associated venous compression [12, 33]. Additionally, it can be helpful in determining the acuity of the lesion [12, 34].
Nutcracker syndrome
Nutcracker syndrome results from compression of the left renal vein between the superior mesenteric artery and spine leading to elevated venous pressures, back pain and hematuria. Left renal vein stenting has emerged as an alternative to renal venous bypass and autotransplant [35]. Similar to iliac vein compression syndrome, anteroposterior compression makes measurement via planar venography problematic. Furthermore, stent migration to the IVC and heart is more common than previously thought, up to 6.7% in one large series where stent undersizing might have been a causative factor [35]. The procedure can be effectively and safely performed in an adolescent population, but with meticulous attention to appropriate stent sizing. Cronan and colleagues [36] demonstrated excellent clinical efficacy and no instances of stent migration in 10 adolescents for whom stents were sized on the basis of both venographic and rotational IVUS measurements. When possible, the renal vein should be assessed without and with Valsava maneuver [37].
Portomesenteric interventions
A DIPS can be created utilizing IVUS guidance as described by Petersen and colleagues [13, 38]. Early experience with DIPS involved IVUS probes capable only of producing images in a transaxial plane; however, subsequent advances in IVUS technology enabled visualization of the entire needle path by a side-firing probe capable of depicting cross-sectional images of the liver. This allows for direct visualization of the portal vein and needle along its entire course, thus facilitating difficult transhepatic portal access (Fig. 6). Central hepatic artery and biliary branches can be identified for avoidance.
Direct intrahepatic portosystemic shunt (DIPS) creation for a 19-year-old man with Budd–Chiari syndrome and failing hepatic venous outflow stent. a Phased-array intravascular ultrasound (IVUS) image in an oblique coronal plane shows the portal vein target (arrowhead) and trans-caudate needle approach (arrow). The IVUS catheter was positioned in the intra-hepatic inferior vena cava (IVC) to obtain this image. b Anteroposterior (AP) projection digital subtraction portal venogram following DIPS access confirms portal venous access. c AP completion venogram confirms successful DIPS creation from right portal vein (white arrow) to the IVC (open arrow)
These same concepts are applied when utilizing IVUS to assist in creating TIPS (Fig. 7). IVUS guidance has been shown to reduce the number of access attempts, procedure time and radiation dose [39, 40]. While IVUS guidance is not always used in TIPS creation for adults, in a review of pediatric TIPS creation the authors strongly recommended routine use of IVUS because of the inherently small patient size and other anatomical challenges [15]. Additional benefits of IVUS cited in that review included the utility of IVUS for confirming wire access into the portal vein, obviating the need for the dual-injection portogram by fluoroscopically marking the hepatic vein confluence for stent measurement, and evaluating stent positioning before complete deployment. In a review of the clinical effectiveness of TIPS creation in 59 pediatric and adolescent patients, the overall technical success rate was 93.4%. IVUS was used in 21 of these patients with 100% technical success [41].
Transjugular intrahepatic portosystemic shunt (TIPS) creation for a 15-year-old girl with idiopathic hepatic fibrosis. a Phased-array intravascular ultrasound (IVUS) image in an oblique coronal plane shows the portal vein target (arrowhead) and the needle (arrow). b In the same plane, the needle is visualized along its entire course as it enters the portal vein (arrowhead). c Anteroposterior (AP) fluoroscopic image shows successful wire passage into the portal vein with the IVUS catheter (arrow) positioned appropriately from a femoral approach. d AP completion venogram confirms successful TIPS creation with reversal of flow in the left portal vein (arrow) and brisk portal diversion through the TIPS from the main portal vein to the right atrium (star)
Catheter-directed thrombolysis is effective and safe treatment for portomesenteric venous thrombosis [42]. Selecting a transjugular intrahepatic approach for portal venous access can mitigate bleeding risk when compared to a transhepatic approach [16]. IVUS reduces access attempts and provides confirmation of portal venous access when blood aspiration confirmation is infeasible because of thrombus (Fig. 8).
Trichobezoar complicated by portal venous thrombosis in a 12-year-old girl. a Axial contrast-enhanced CT of the abdomen demonstrates portal thrombosis (arrow). b Phased-array intravascular ultrasound (IVUS) with Doppler in an oblique coronal plane demonstrates echogenic thrombus within the main portal vein (arrows). c In the same plane, IVUS-guided transjugular intrahepatic portosystemic shunt (TIPS) approach to portal venous access, from the middle hepatic vein (arrowhead) to left portal vein (arrow), is performed. d Anteroposterior (AP) portal venogram confirms portal venous entry and abrupt cessation of flow from the main portal vein (star) to the portal bifurcation and intrahepatic branches (arrowheads). The IVUS probe is situated within the intrahepatic inferior vena cava (arrow). e AP digital subtraction portal venogram following single-session pharmaco-mechanical thrombolysis demonstrates residual nonobstructive thrombus adjacent to the portal vein bifurcation (arrow) but improved intrahepatic portal venous flow
Endovascular aspiration and biopsy
Image-guided percutaneous biopsy is one of the procedures most frequently performed by the interventionalist. Ultrasound-, CT- and less frequently MRI-guided biopsies are commonplace. In the case of thoracic lesions requiring biopsy, endobronchial US-guided biopsy and mediastinoscopy capabilities are limited in some pediatric centers. For lesions inaccessible by these approaches but abutting or within large venous structures, IVUS-guided technique might be considered (Fig. 9) [43, 44]. One study of 50 IVUS-guided transvenous biopsies of perivascular targets showed high diagnostic accuracy, although the authors noted that complication rates might be slightly higher compared to percutaneous needle biopsy [45]. IVUS guidance might facilitate endovascular liver biopsy when a transcaval approach is necessitated by Budd–Chiari syndrome or post-surgical anatomy precluding hepatic vein access [46].
Transvenous biopsy performed with intravascular ultrasound (IVUS) guidance in a 17-year-old girl with a mediastinal mass. a Axial contrast-enhanced CT of the chest demonstrates a large central mass (arrow) insinuating between the azygos veins and ascending aorta and effacing the superior vena cava (SVC). b Phased-array IVUS from a femoral approach with the tip positioned in the SVC in an oblique coronal plane identifies the mass (arrowheads) and a safe transvascular approach. c, d Hybrid oblique coronal IVUS (c) and anteroposterior fluoroscopic imaging (d) monitors the femoral approach passage of a 19-gauge endovascular biopsy needle (arrows). Biopsy confirmed non-Hodgkin lymphoma
Conclusion
The use of IVUS has become increasingly prevalent in adult interventional radiology and has proved to be a safe and effective tool a myriad of situations. While IVUS is not as commonly employed in the pediatric setting, it can be used effectively to expand the procedural repertoire of the pediatric interventionist. Use of IVUS is feasible and safe in various procedures in children, with distinct advantages that extend beyond the standard angiographic techniques. Further study is needed to obtain longitudinal data regarding patient outcomes and overall costs.
References
Yock PG, Linker DT, Thapilyal HV et al (1988) Real-time two-dimensional catheter ultrasound: a new technique for high-resolution intravascular imaging. J Am Coll Cardio 11:130A
Belkin N, Jackson BM, Foley PJ et al (2020) The use of intravascular ultrasound in the treatment of type B aortic dissection with thoracic endovascular aneurysm repair is associated with improved long-term survival. J Vasc Surg 72:490–497
Tsujita K, Maehara A, Mintz GS et al (2008) Comparison of angiographic and intravascular ultrasonic detection of myocardial bridging of the left anterior descending coronary artery. Am J Cardiol 102:1608–1613
Nissen SE, Yock P (2001) Intravascular ultrasound: novel pathophysiological insights and current clinical applications. Circulation 103:604–616
Shlofmitz E, Kerndt CC, Parekh A, Khalid N (2020) Intravascular ultrasound. StatPearls, Treasure Island. http://www.ncbi.nlm.nih.gov/books/NBK537019/. Accessed 21 Sep 2021
Levine GN, Bates ER, Blankenship JC et al (2011) 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines and the Society for Cardiovascular Angiography and Interventions. JACC 58:e44-122
Neumann J, Sousa-Uva M, Ahlsson A et al (2019) 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 40:87–165
Sheikh AB, Anantha-Narayanan M, Smolderen KG et al (2020) Utility of intravascular ultrasound in peripheral vascular interventions: systematic review and meta-analysis. Vasc Endovasc Surg 54:413–422
Elgendy IY, Mahmoud AN, Elgendy AY, Bavry AA (2016) Outcomes with intravascular ultrasound-guided stent implantation: a meta-analysis of randomized trials in the era of drug-eluting stents. Circ Cardiovasc Interv 9:e003700
Ahn J-M, Kang S-J, Yoon S-H et al (2014) Meta-analysis of outcomes after intravascular ultrasound–guided versus angiography-guided drug-eluting stent implantation in 26,503 patients enrolled in three randomized trials and 14 observational studies. Am J Cardiol 113:1338–1347
Loffroy R, Falvo N, Galland C et al (2020) Intravascular ultrasound in the endovascular treatment of patients with peripheral arterial disease: current role and future perspectives. Front Cardiovasc Med 7:551861
Marteslo JP, Makary MS, Khabiri H et al (2020) Intravascular ultrasound for the peripheral vasculature — current applications and new horizons. Ultrasound Med Biol 46:216–224
Petersen B, Uchida BT, Timmermans H et al (2001) Intravascular US-guided direct intrahepatic portacaval shunt with a PTFE-covered stent-graft: feasibility study in swine and initial clinical results. J Vasc Interv Radiol 12:475–486
Pillai A, Andring B, Iyamu I (2016) Conventional vs. intravascular ultrasound (IVUS) guided transjugular intrahepatic portosystemic shunt (TIPS) creation: a comparison of success, efficiency, complications, and radiation dose. J Vasc Interv Radiol 27:S194
Monroe EJ, Shin DS, Shivaram GM, Koo KSH (2017) Pediatric transjugular intrahepatic portosystemic shunts. Dig Dis Interv 1:277–285
Koo KSH, Lamar DL, Shaw DWW et al (2018) Catheter-directed thrombolysis for portal vein thrombosis in children: a case series. J Vasc Interv Radiol 29:1578–1583
Hodgkiss-Harlow K, Back MR et al (2012) Technical factors affecting the accuracy of bedside IVC filter placement using intravascular ultrasound. Vasc Endovasc Surg 46:293–299
McDevitt JL, Srinivasa RN, Hage AN et al (2019) Total endovenous recanalization and stent reconstruction for naïve non-inferior vena cava filter-associated chronic iliocaval occlusive disease: placement of 352 venous stents in 69 debilitated patients. Vasc Med 24:349–358
Chick JFB, Jo A, Meadows JM et al (2017) Endovascular iliocaval stent reconstruction for inferior vena cava filter–associated iliocaval thrombosis: approach, technical success, safety, and two-year outcomes in 120 patients. J Vasc Interv Radiol 28:933–939
McDevitt JL, Srinivasa RN, Gemmete JJ et al (2019) Approach, technical success, complications, and stent patency of sharp recanalization for the treatment of chronic venous occlusive disease: experience in 123 patients. Cardiovasc Intervent Radiol 42:205–212
Chick JFB, Roush BB, Khaja MS et al (2017) Transbiliary intravascular ultrasound-guided diagnostic biopsy of an inaccessible pancreatic head mass. Radiol Case Rep 12:323–326
Yan F, Rajah G, Ding Y et al (2019) Safety and efficacy of intravascular ultrasound as an adjunct to stenting for cerebral venous sinus stenosis-induced idiopathic intracranial hypertension: a pilot study. J Neurosurg 132:749–754
Clark DJ, Lessio S, O’Donoghue M et al (2004) Safety and utility of intravascular ultrasound-guided carotid artery stenting. Catheter Cardiovasc Interv 63:355–362
Enriquez A, Saenz LC, Rosso R et al (2018) Use of intracardiac echocardiography in interventional cardiology: working with the anatomy rather than fighting it. Circulation 137:2278–2294
Raju S, Buck WJ, Crim W, Jayaraj A (2018) Optimal sizing of iliac vein stents. Phlebology 33:451–457
Gill AE, Ciszak T, Braun H, Hawkins CM (2017) Intravascular ultrasound versus digital subtraction angiography: direct comparison of intraluminal diameter measurements in pediatric and adolescent imaging. Pediatr Radiol 47:450–457
Manninen HI, Räsänen H (2000) Intravascular ultrasound in interventional radiology. Eur Radiol 10:1754–1762
Zhao X, Zhao L, Wu L et al (2020) Efficacy of percutaneous transluminal renal angioplasty for pediatric renovascular hypertension: a meta-analysis. Zhonghua Er Ke Za Zhi 58:661–667
McDevitt JL, Srinivasa RN, Hage AN et al (2019) Lower extremity endovenous reconstruction for symptomatic occlusive disease in pediatric patients: techniques, clinical outcomes, and long-term stent patencies. Pediatr Radiol 49:808–818
Montminy ML, Thomasson JD, Tanaka GJ et al (2019) A comparison between intravascular ultrasound and venography in identifying key parameters essential for iliac vein stenting. J Vasc Surg Venous Lymphat Disord 7:801–807
Aslesen A (2019) Assessing venous disease for optimal endovascular stent placement. BackTable podcast. https://www.backtable.com/post/endovascular-stent-placement-venous-disease. Accessed 21 Sep 2021
Sherman TF (1981) On connecting large vessels to small. The meaning of Murray’s law. J Gen Physiol 78:431–453
Hager ES, Yuo T, Tahara R et al (2013) Outcomes of endovascular intervention for May-Thurner syndrome. J Vasc Surg Venous Lymphat Disord 1:270–275
Majdalany BS, Khaja MS, Williams DM (2017) Intravascular ultrasound-guided intervention for May-Thurner syndrome. Semin Interv Radiol 34:201–207
Wu Z, Zheng X, He Y et al (2016) Stent migration after endovascular stenting in patients with nutcracker syndrome. J Vasc Surg Venous Lymphat Disord 4:193–199
Cronan JC, Hawkins CM, Kennedy SS et al (2021) Endovascular management of nutcracker syndrome in an adolescent patient population. Pediatr Radiol 51:1487–1496
Syed MI, Yu B, Akhter T, Shaikh A (2011) Renal vein stenting via the right internal jugular approach with a provocative Valsalva maneuver to reduce the risk of stent migration. Perspect Vasc Surg Endovasc Ther 23:268–271
Petersen BD, Clark TWI (2008) Direct intrahepatic portocaval shunt. Tech Vasc Interv Radiol 11:230–234
Kew J, Davies RP (2004) Intravascular ultrasound guidance for transjugular intrahepatic portosystemic shunt procedure in a swine model. Cardiovasc Intervent Radiol 27:38–41
Kao SD, Morshedi MM, Narsinh KH et al (2016) Intravascular ultrasound in the creation of transhepatic portosystemic shunts reduces needle passes, radiation dose, and procedure time: a retrospective study of a single-institution experience. J Vasc Interv Radiol 27:1148–1153
Bertino F, Hawkins CM, Shivaram G et al (2019) Technical feasibility and clinical effectiveness of transjugular intrahepatic portosystemic shunt creation in pediatric and adolescent patients. J Vasc Interv Radiol 30:178–186
Chamarthy MR, Anderson ME, Pillai AK, Kalva SP (2016) Thrombolysis and transjugular intrahepatic portosystemic shunt creation for acute and subacute portal vein thrombosis. Tech Vasc Interv Radiol 19:42–51
Thakrar PD, Petersen BD, Kaufman JA (2013) Intravascular ultrasound for transvenous interventions. Tech Vasc Interv Radiol 16:161–167
RiChard J, Thornburg B, Desai S et al (2019) Intracardiac echocardiography (ICE)-guided external iliac transvenous needle biopsy of an extravascular retroperitoneal mass. Int J Clin Ski 13:259–263
Swenson C, Martin JG, Jaffe T et al (2021) Intravascular ultrasound guided transvenous biopsy of abdominal and pelvic targets difficult to access by percutaneous needle biopsy: technique and initial clinical experience. J Vasc Interv Radiol 32:1310–1318
Kaufman C, Gaumond J, Kaufman J (2017) Transjugular liver biopsy following orthotopic whole liver transplantation: challenges and solutions. A pictorial essay. J Clin Interv Radiol 1:107–112
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Jeffrey Forris Beecham Chick is a consultant and speaker for Inari Medical, Guerbet, C. R. Bard, Argon Medical Devices and Boston Scientific. Eric J. Monroe is a scientific adviser and speaker for Biogen.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weaver, J.J., Shin, D.S., Chick, J.F.B. et al. Intravascular ultrasound for endovascular precision in pediatrics. Pediatr Radiol 52, 559–569 (2022). https://doi.org/10.1007/s00247-021-05220-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-05220-7