Abstract
There is little current literature on the augmented-pressure distal colostogram, the single most important diagnostic study performed in boys with imperforate anus prior to definitive repair. Accurate understanding of the anatomy of the anorectal malformation including an associated fistulous communication between the rectum and the urogenital tract is essential for optimal surgical management. Specifically, the position of the rectal pouch and recto-urinary fistula relative to posterior sagittal structures of the perineum, especially the sacral spine, dictates the operative approach. This pictorial essay is a guide for those who encounter such children with relative infrequency to become more comfortable with the technique. We report how to perform this radiologic exam and the potential pitfalls from our experience of performing the technique in our large pediatric colorectal practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of anorectal malformation is approximately 1 in 5,000 births. Children with anorectal malformation usually present at birth with distal bowel obstruction and absent anal opening on newborn physical exam. These children often have associated abnormalities including vertebral or other musculoskeletal anomalies, esophageal atresia, duodenal atresia, renal anomalies, tethered spinal cord and cardiac anomalies. The most common anomalies associated with anorectal malformation are renal anomalies, spinal cord tethering and congenital heart disease. In some newborns with esophageal atresia and all with duodenal atresia, the atretic segment prevents swallowed air from accumulating in the colon; therefore the obstructive bowel pattern typical of anorectal malformation is absent in these cases, and if the absence of the anal opening is not noted on clinical exam the anorectal malformation could go undetected, delaying treatment [1].
Many newborns with imperforate anus undergo a diverting colostomy after the first 24–48 h of age. Definitive surgical repair is usually performed at 6–8 weeks of age or later depending on the presence of associated congenital anomalies and the clinical status of the child. The most common way to repair an anorectal malformation is by the posterior sagittal approach that involves (a) a midline incision between both buttocks; (b) division of parasagittal fibers, anal sphincter muscle complex and levator muscle fibers in the midline, and identification of the rectum; (c) enterotomy of the distal rectum in the midline with identification, and isolation of the rectourinary fistula; (d) mobilization of the rectum and careful separation of the rectum from the anteriorly located urethra (which is the source of the most serious complications during the repair); (e) closure of the fistula; (f) circumferential perirectal dissection to gain enough tension-free rectal length to reach the perineum; (g) electrical confirmation of the anterior limits of the sphincter mechanism, which are marked with sutures, with closure of the anterior perineal body; (h) electrical confirmation of the posterior limit of the sphincter mechanism, and loose stitching of the rectum in front of it and the muscle complex brought together behind it; (i) closure of the posterior limit of the muscle complex, including the parasagittal fibers, behind the rectum, including part of the rectal wall to help avoid rectal prolapse; (j) anoplasty followed by closure of the ischiorectal fossa and subcutaneous tissues (Fig. 1) [2]. Through this approach, the surgeon can find the rectum and its connection with the male urethra in 90% of cases; in 10% of cases, those with recto-bladder-neck fistula, the rectum can only be reached by laparotomy or laparoscopy because the rectum is anterior to the sacrum, unreachable by the posterior sagittal approach [1]. Therefore it is essential for the surgeon to know the location of the rectum preoperatively as related to the most distal portion of the sacrum or coccyx. Looking for the rectum in the wrong place is the reason for most surgical misadventures in these children, a common cause of operative complications [3].
Posterior sagittal anorectoplasty. a Midline incision from coccyx posteriorly to the base of the scrotum anteriorly. b Division of parasagittal fibers. c Division of sphincter muscle complex and levator muscle fibers in the midline and identification of the rectum. d Enterotomy of the distal rectum in the midline with identification of the rectourinary fistula. e Isolation of the rectourinary fistula. f Mobilization of the rectum and careful separation of the rectum from the anteriorly located urethra (which is the source of the most serious complications during the repair). g Closure of the fistula. h The anterior limits of the sphincter mechanism are electrically confirmed and marked with sutures, with closure of the anterior perineal body. i The posterior limits of the sphincter mechanism are electrically confirmed and marked with sutures and rectum is brought within the muscle complex. j The posterior limit of the muscle complex is closed behind the rectum, including part of the rectal wall to help avoid rectal prolapse. Reprinted with kind permission of Springer Nature [2]
In 1982 the first posterior sagittal exploration of a child with an anorectal malformation was performed, allowing the first direct observation of the intrinsic anatomy of these defects. It was found that the “puborectalis muscle,” traditionally considered an important landmark, actually was not the “rectal sphincter” [4]. Instead, it was found that these children have a funnel-like muscle structure surrounding the rectum that represents the pelvic floor and sphincter muscles. The upper limit of this funnel is the pubococcygeal line. This anatomical concept has been confirmed during thousands of surgical explorations during the last 35 years and with the images provided by more accurate imaging techniques such as MRI, the traditional old classification of these defects into “high,” “intermediate” and “low” [5] has proved to be fictitious and misleading [6]. In the last few years, MRI has been used for preoperative surgical planning [7], although if the lumen of the mucous fistula to the distal rectal pouch is not distended during the MRI, then the anorectal malformation can be misinterpreted as high. Figure 2 shows diagrams of anorectal malformations in boys including perineal fistula, bulbar urethral fistula, prostatic urethral fistula, bladder neck fistulae and no fistula. The surgical repair of these defects depends on the preoperative knowledge of the precise location of the rectum and the fistula, which is present in 95% of cases anywhere from the perineum to the bladder neck, except in children with Down syndrome, in whom only 5% have a fistula [8]. Specifically the location of the rectal pouch in relation to the tip of the spine is paramount in deciding the surgical approach. Inherent in the anatomy and function of the rectum, it is extremely important in this regard to understand that the lowest part of the rectum is usually collapsed from the muscle tone of the funnel-like striated muscle mechanism that surrounds the rectum in 90% of cases (in 10% of cases, mostly bladder-neck fistulae, the fistula is above the sphincter muscles). In order to fill the distal rectum and force contrast material through a fistula, it is necessary to exert a significant amount of hydrostatic pressure to overcome the tone of the funnel-like muscle mechanism, for a concept emphasized in the name of this essay with the term “augmented pressure.” Gross, Wolfson and Peña [9] in 1991 reported the first description of the augmented-pressure distal colostogram as a diagnostic tool in three children with imperforate anus and recto-urinary fistula. Since then, two articles have concerned the distal colostogram, one by Mickelson et al. [10] in 2007 and one by Rahalkar et al. [11] in 2010.
Perineal fistula anorectal malformation. a Rectum (R) has orifice that is on the perineum (solid arrow) but is anterior to the anal sphincter (dashed arrow), which is usually well formed. Note that the urethra (curved arrow) is normal. b Recto-bulbar urethral fistula anorectal malformation. Rectum fistulizes to the urethra where the mucosa is bulbar spongiosum, usually at or distal to the bend of the urethra (solid arrow). Note that the anal sphincter is well-formed (dashed arrow). c Recto-prostatic urethral fistula anorectal malformation. Rectum fistulizes to the urethra where mucosa is prostatic epithelium, above the bend of the urethra (solid arrow), usually proximal to the urethral sphincter. Note attenuated anal sphincter (dashed arrow). d Recto-bladder-neck urethral fistula anorectal malformation. Rectum fistulizes to the bladder neck (solid arrow). Note anal sphincter is very attenuated (dashed arrow). e No-fistula anorectal malformation. Rectum is blind-ending in the pelvis (solid arrows) usually at the bulbar urethral level. Note well-developed anal sphincter (dashed arrow). Reprinted with kind permission of Springer Nature [2]
Instillation of the contrast material by gravity through a balloon-tipped catheter within the distal stoma (mucous fistula), or by a catheter with the inflated balloon outside the stoma held against the stoma manually to prevent leakage, most frequently results in leakage of the contrast material through the stoma and a characteristic image of the contrast material ending in a horizontal line or convex superior configuration that corresponds to the pubococcygeal line (Fig. 3), the cephalad portion of the muscle funnel. To overcome the muscle tone of the rectum requires significant hydrostatic pressure provided by a closed system accomplished by occluding the distal stoma with a balloon-tipped catheter inside, subjected to traction during injection. When the pressure is high enough, the contrast material fills the most distal part of the rectum and the fistula. A rounded appearance of the distal rectal pouch suggests adequate pressure; when there is no fistula, this appearance persists. When a fistula is present, usually there is a tapered configuration at the anterior aspect of the distal rectal pouch prior to filling the fistula and opacification of the bladder or urethra. Figure 4 shows the same colostogram as in Fig. 3 but with augmented pressure.
Distal colostogram with inadequate pressure. a Distal colostogram in a 4-month-old boy performed with inadequate pressure shows contrast agent infused by gravity from a bag. Black line denotes the rectal sphincter, which is flat, closed and not distended because of inadequate pressure. b Distal colostogram in a 2-month-old boy shows rectal sphincter that is closed (black arrows) because of inadequate pressure, likely because the retention balloon is outside the patient (white arrows) rather than inside. Contrast agent was also infused by gravity from a bag
Most surgical explorations resulting in poor outcomes in children with anorectal malformations occur when the surgeon opens from the posterior sagittal approach without the indispensable information provided by the augmented-pressure distal colostogram [12]. This is the reason our team considers this study the most valuable diagnostic tool from the therapeutic point of view.
Technique and findings
Materials needed for an augmented-pressure distal colostogram include an 8- or 10-French balloon-tipped catheter (priming of the catheter balloon by inflation and deflation is usually performed outside the patient prior to insertion), lubricant jelly, a catheter-tip or luer-lock syringe with catheter-tip adapter, water-soluble contrast material (preferably isosmotic to body fluids), small radiodense marker or BB, tape and a fluoroscopy unit, preferably one configured for pediatric low-dose technique. Specifically, a 60-mL leur-lock syringe is loaded aseptically with 50 mL iodixanol 320 isosmotic water-soluble contrast agent and fitted with a catheter-tipped adapter on the leur-lock end. Alternatively, one can use a 60-mL catheter-tipped syringe, although this type of syringe is more difficult to load aseptically. The more dense the contrast agent, the better the visualization of very narrow fistulae and other structures that might fill, such as a subtle utricle or subtle vesicoureteral reflux; we prefer contrast agent with at least 300 mg iodine/mL. The performance of the augmented-pressure distal colostogram is straightforward; however it is extremely important to know the complete history of the child and review prior radiologic studies before performing the procedure. One pitfall sometimes encountered at the beginning of the study is spontaneous closure of the mucous fistula resulting in no access to place a catheter into the distal colonic segment for injection of contrast agent. In these cases, the surgeon might opt to delay the definitive repair and re-open the mucous fistula, in order to perform the high-pressure distal colostogram prior to repair. If the child is older than 1–2 years, the value of having a child life specialist to distract the child during the procedure cannot be over-emphasized because these exams are performed (in our department) without sedation. Proper immobilization can be attained by the radiology technologist and it is imperative to position child optimally to obtain diagnostic images. Placing the child in a papoose or on an octagon board for immobilization is an option, but we have found that holding the child is more comforting to the child; the fluoroscopist can then manually correct the child’s position with the right hand while acquiring images with the left hand.
A small radiodense BB marker is placed in the expected location of the anal sphincter, (usually demarcated by oval discoloration of the skin in the midline intergluteal region posterior to the inferior scrotal raphe and anterior to the sacral dimple if one is present), and taped in place (Fig. 5) to facilitate digital measurements. Alternatively, one can additionally place a radiopaque ruler beneath the child that is visible on all images; however with the sophisticated measuring tools on most picture archiving and communication systems, digital measuring is the most accurate and preferred method to measure radiographically. When placing the BB, one shouldn’t mistake the sacral dimple, which is more posterior on the perineum (Fig. 5), for the region of the anal sphincter. Sometimes there is a dimple or band of extra skin in the region of the anal sphincter. With the child lying supine on the fluoroscopy table, the abdomen is exposed and the location of the mucous fistula ostomy is identified (Fig. 6). The region of the stoma is cleaned and a small amount of lubricant jelly is placed on the stoma prior to cannulation; the tip of the primed, balloon-tipped catheter is then inserted into the stoma far enough so that the balloon is into the proximal lumen of the ostomy of the mucous fistula (Fig. 6). The balloon is then carefully inflated with 1–2 mL of air, just enough to occlude the stoma but not over-distend the bowel lumen. One can feel with the thumb on the plunger of the syringe when the balloon is meeting resistance to inflation. Prior to high-pressure injection, a small amount of contrast agent is injected through the catheter under fluoroscopy to make sure the balloon caliber is not more than the caliber of the lumen of the mucous fistula, and the balloon is then pulled back against the stoma to prevent leakage of contrast agent during injection (Fig. 7). If the balloon caliber is too large, the bowel can be perforated near the stoma (Fig. 8). In the lateral view, contrast agent is slowly injected during fluoroscopy to fill the colon to the level of the rectal pouch; the femoral heads must be superimposed (true lateral position) and the anterior abdominal wall with intraluminal balloon up against it, the sacrum, and the anal marker must be in view; contrast injection under fluoroscopy is continued until the flat or convex-superior appearance of the rectal pouch caused by a closed/contracted rectal sphincter is overcome by the pressure of injection and results in rounding or convex-inferior distention of the rectal pouch (Fig. 9). With continued injection there is either prompt filling of the fistula from the rectum to the bladder (Fig. 10) or development of a tapered appearance of the anterior aspect of the rectal pouch and filling of a fistula to the urethra (Fig. 11) or no filling of a fistula with a persistently rounded appearance of the rectal pouch despite adequate distention (Fig. 12). If the bladder fills fairly easily either directly via a recto-vesical fistula or indirectly via a proximal urethral fistula, filling can be continued until voiding occurs, denoting where the fistula enters the urethra, which allows most precise classification the anorectal malformation. An image in the true lateral view includes the ossified sacrum, the colon from the mucous fistula of the abdominal wall to the rectal pouch, the fistula, the contrast-filled bladder, urethra and any other genitourinary structures, and the anal dimple (BB) on one image (Fig. 13). If one observes vesicoureteral reflux (VUR), oblique views of the ureterovesical junction in relation to bladder neck could be performed to assess the location of the ureteral insertion because it could be ectopic (Fig. 14), not uncommonly seen in children with anorectal malformations, especially if there is hydronephrosis or hydroureteronephrosis on the initial renal and bladder ultrasound. If there is filling of the vas deferens or ejaculatory ducts, these structures should also be documented given the higher than normal incidence of tethered spinal cord in children with anorectal malformation; these findings might be related to higher-than-normal tone of the urethral sphincter resulting in high-pressure voiding and vas deferens or ejaculatory duct reflux, signs of neurogenic bladder. Sometimes, these structures fill on a voiding cystourethrogram (VCUG; Fig. 15) but not on the colostogram of the same child (Fig. 16). The child is then turned to his back and an anteroposterior view (Fig. 17 is obtained for an accurate estimation of the length of this segment of colon for mobilization to the anal sphincter region for pull-through. The other measurement of importance is the length of the rectal pouch to the BB on the anal sphincter region.
BB placement for distal colostogram in a 3½-month-old boy. Clinical photograph of a radiopaque BB placed on the expected location of the anal sphincter denoted by a dimple surrounded by a darker ring of skin approximately halfway between the scrotum and sacral dimple (arrow), which is usually at the level of the coccyx
Mucous fistula identification. a Clinical photograph of the same boy as in Fig. 5, who had a separated colostomy performed at birth. The smaller medial one (solid arrow) is the mucous fistula, the opening to the distal colonic segment; the lateral one is the end colostomy (dashed arrow). b Foley catheter (F) is placed into the mucous fistula
Image-hold image performed during distal colostogram in a 3-month-old boy. Foley catheter balloon (black arrows) is inflated less or equal to the caliber of the segment noted by contrast agent within it. Also, note that balloon is pulled up against the abdominal wall (white arrows) to avoid contrast agent leakage
Overinflated retention balloon during distal colostogram in an 8-month-old boy. a Foley catheter balloon (solid arrows) is over-inflated relative to the caliber of the distal segment (dashed arrows), increasing risk of local perforation with high-pressure injection. b Anteroposterior view of same boy shows extraluminal contrast agent (dashed arrows) from local perforation at the level of mucous fistula in the region of the overinflated Foley balloon
Distal colostogram in a 3½-month-old boy with no fistula. Filled distal colonic segment shows a caudal bulging or rounded appearance of the rectal pouch (arrows), suggesting adequate distention of the rectal sphincter. The rectal pouch without fistula, as in this case, is typically at the bulbar urethral level, well below the coccygeal tip
Distal colostogram in a 3-month-old boy shows a recto-bladder-neck fistula (arrow). The fistula is located anterior to the sacrum rather than distal to sacral tip, which affects the surgical approach, requiring abdominal approach in addition to the posterior sagittal approach, a longer and more complex operation. Note the distal colonic segment is too short to reach the perineum
Distal colostogram in a 4½-month-old boy shows recto-bulbar urethral fistula (solid arrow) with contrast agent filling the bulbous and penile urethra (dashed arrows). There is no filling of the proximal urethra because the fistula is likely beyond the urethral sphincter, which is suggested by the low position of the rectal pouch in relation to the anal sphincter (BB). If the radiologist fails to distend the rectum adequately and fails to opacify the fistula, he or she could erroneously conclude there is no fistula. The surgeon would encounter the rectum and bring it down to the anus, pulling through with the fistula intact, an unwanted surgical outcome
Distal colostogram in a 1-month-old boy shows the recto-prostatic urethral fistula (dashed black arrows), which is proximal to the bend of the urethra (solid white arrow) and below the presumed bladder neck (solid black arrow), although the bladder is not that well distended and the bladder neck might be slightly more caudad than shown. Note the entire distal colon segment, distal spine (dashed white arrow) and BB are all in view in this true lateral image (femurs overlapping)
Voiding phase of voiding cystourethrogram in a 3-month-old boy with anorectal malformation. There is reflux of contrast agent into the ejaculatory duct (arrows), suggesting high-pressure voiding. This is not uncommonly seen in children with anorectal malformation and neurogenic bladder (note there are only four sacral segments, consistent with sacral hypoplasia)
Distal colostogram on same boy as in Fig. 15. Study failed to show similar findings because contrast entered the urethra distal to the urethral sphincter in this child with recto-bulbar urethral fistula
Anteroposterior (AP) view from distal colostogram of the patient illustrated in Fig. 7. In the lateral view shown in Fig. 7, the filled segment appears short. However, in the AP view of the same colostogram shown here, there is adequate length to reach the perineum, which demonstrates how the distal colonic segment can appear short from overlap or redundancy of the segment on lateral view and demonstrates the utility of obtaining both views of the filled distal colonic segment
The location of fistula insertion into the urinary tract is important information to classify the type of anorectal malformation. In a case in which there is a tiny fistulous communication with only a small amount of contrast agent passing through it, one might need to catheterize the bladder via the urethra and fill the bladder until voiding occurs, thus defining the relationship between the region of the fistula and the urethra in relation to the bladder neck (Fig. 18). At the completion of the study, one could aspirate as much contrast agent as possible from the distal limb of the colon, especially if using hyperosmotic contrast agent, to avoid fluid shifts that could cause dehydration.
Distal colostogram in a 2-month-old boy initially shows a very small fistula (solid arrow) with little contrast agent in the proximal urethra, so the relationship of the fistula to the bladder neck is unclear; therefore the catheter is placed (dashed arrows) and bladder filled to locate the bladder neck (arrowhead). This child was diagnosed with recto-bulbar urethral fistula
Sometimes instead of a separated colostomy and mucous fistula, a surgeon performs a loop colostomy and the distal limb of the colon is found inside or immediately adjacent to a single stomal opening. This is not optimal because the mucous fistula resides within the colostomy bag, allowing for contamination of the urinary tract by spillage of feces into the distal limb. However this type of colostomy might be encountered in a referral practice. Cannulation of the distal limb via the mucous fistula can be tricky in these children. Inserting the catheter into the single opening, pointing in the direction toward the anus, and injecting a small amount of contrast agent frequently shows whether the catheter is in the distal limb; if not, redirecting the catheter and reinjecting can enable manipulation of the catheter into the correct position. The retention balloon of the catheter is then carefully inflated inside the lumen. If one cannot cannulate the distal limb of the colon, requesting the help of the referring surgeon is recommended.
In children with a long segment of distal colon (those who have had a transverse colonic or more proximal colostomy) the colon proximal to the sigmoid might be small from non-use (Fig. 19). In addition, be aware that residual meconium in the distal rectum can prevent filling of the fistula during contrast injection and therefore can cause one to erroneously conclude there is no fistula or require more forceful injection to demonstrate the fistula, placing the colon at risk for perforation, more so than if the child had a rectosigmoid or descending colon colostomy.
The most important complication of the high-pressure distal colostogram is perforation. Despite this increased potential risk of perforation, only three perforations have occurred in our large series of patients, usually because of either (1) a very long, small, unused distal colonic segment or (2) meconium buildup against the distal rectal pouch of a very dilated rectosigmoid distal colonic segment (Fig. 20). These situations are associated with higher pressure and the volume of injection needed to opacify the fistula, or Foley balloon inflation larger than the caliber of the lumen of the mucous fistula (Fig. 8). If perforation occurs into the peritoneal space with an isosmotic contrast agent, no fluid shifts occur but the child is at risk to develop peritonitis and sepsis and this requires antibiotics and an operation to fix the colon. If hyperosmotic contrast agent is used, fluid shift into the peritoneal space from the intravascular space puts the child at added risk of intravascular volume depletion and potential hypotension and this requires intravascular volume resuscitation in an urgent manner.
Practical suggestions to avoid pitfalls when performing distal colostogram
Several pitfalls in performing the high-pressure distal colostogram technique can lead to erroneous conclusions. One important pitfall is the conclusion that there is no fistula, sometimes described as “high anorectal malformation with no fistula.” We have found this classification of “high versus low” malformations unhelpful and prefer to use a precise anatomical description. Often this error of failing to demonstrate the fistula results from incomplete distention of the rectal pouch during injection, which is characteristically seen as flattening or a convex superior configuration of the contrast head at the distal end of the rectal pouch (Fig. 3). There might be several reasons for this: (1) a catheter without a balloon tip is used for injection of contrast agent, resulting in failure to generate the necessary pressure to overcome the rectal sphincter tone, which is necessary to fill the distal-most aspect of the rectal pouch and fistula; (2) the balloon of the catheter is deep into the distal colonic segment, not occluding the mucous fistula at the skin, and stomal leakage of contrast agent results; again, the pressure generated by injection is insufficient to fully distend the rectal pouch and fails to fill the fistula (Fig. 21); (3) there is a very long segment from ostomy of mucous fistula to rectal pouch (transverse colon or more proximal colostomy), making it difficult to transmit high enough pressure to the rectal pouch. Additionally, if one inserts the catheter into the mucous fistula with the balloon inflated outside the stoma, holding it up against the stoma to prevent leakage, there is usually insufficient rectal distention and failure of opacification of the fistula (Fig. 3). In children without a fistula (Fig. 9), the distal rectal pouch is most commonly found at the bulbar urethral level, well below the level of the last ossified sacral segment [8]. If one concludes erroneously there is no fistula, the surgeon might have the incorrect perception that the rectal pouch is higher than it actually is. This can result in injury to adjacent structures while the surgeon searches for the rectum in the wrong place or can lead to leaving the distal rectum still attached to the urethra through a fistula.
Distal colostogram in a 1½-year-old boy shows the catheter retention balloon (arrowheads) deep into the colon segment just above the rectum. Contrast agent leaked from the mucous fistula during injection, preventing adequate pressure to overcome the rectal sphincter tone (arrows) to distend rectal pouch
Another important pitfall is erroneously reporting the level of the distal rectal pouch in relation to the last ossified sacral segment because this landmark is important in planning the surgical approach. Perineal, bulbar-urethral and select prostatic-urethral fistulae are repaired primarily by posterior sagittal approach only (because the rectal pouch is at or inferior to the ossified sacral tip), whereas select prostatic-urethral and bladder-neck fistulae (where the rectal pouch is anterior to the sacrum) are operated using a both posterior sagittal and abdominal approach, a more complex operation [1]. Therefore it is important to show the relationships of all structures in the proposed operative field. Specifically, one needs to show the expected location of the anus and the ossified sacral or coccygeal tip with the contrast-filled rectum and fistula on a true lateral image (Fig. 22). If the distal rectal pouch and fistula are above the ossified sacral tip, access to this structure is difficult from the posterior sagittal approach and likely necessitates an abdominal approach (laparotomy or laparoscopy) as well, a much more complex and time-consuming operation.
Discussion
Imperforate anus is caused by abnormal separation of the structures of the genitourinary system and hindgut early in embryogenesis [4]. Associated fistulous communications can extend from the atretic rectum to the bladder, prostatic or bulbar urethra, or perineum in boys. No fistula occurs in only about 5% of chromosomally normal boys with imperforate anus; however, in boys with Down syndrome about 95% have no fistulous communication [8]. Therefore in the context of proper technique, one should be able to demonstrate a fistulous connection by high-pressure distal colostogram in a normal-chromosome boy with anorectal malformation when it is present.
Historically, there have been a number of classification schemes for children with imperforate anus. The one that is most clinically useful is anatomically based [13]. In this scheme, initial classification and management is almost exclusively by clinical criterion. Initial operative management entails either definitive repair in the neonatal period, or a diverting colostomy in the neonatal period followed by a delayed definitive repair within the first year of age. Boys with perineal fistulae and those with a thin membrane between the rectal pouch and the skin at the perineum can be repaired primarily in the neonatal period. These children are diagnosed and evaluated clinically and do not typically require radiologic contrast studies of the malformation prior to neonatal or delayed repair. Children with more complex anatomy undergo a neonatal diverting colostomy (ideally a proximal sigmoid colostomy right after it comes off the left retroperitoneum) with creation of separate end-colostomy and mucous fistula giving access to the distal colonic segment for performing the distal colostogram. These children include boys with clinical evidence of a fistula to the urethra or bladder (meconium passed per urethra) and boys with no clinical evidence of a fistula but with a rectal pouch that is not close to the skin.
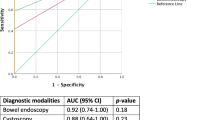
The fluoroscopic differentiation of the types of recto-urinary communication is helpful because recto-prostatic urethral fistulae have a poorer clinical prognosis than recto-bulbar urethral fistulae, and the operative approach, location of the rectum and extent of rectal mobilization differ significantly. Rarely one encounters no fistula in a boy with normal chromosomes (5%); the rectal pouch is usually inferior to the level of the last ossified sacral segment, which can be well delineated by the colostogram so the surgeon knows where to expect it during the dissection. In these children, the level of the distal rectal pouch is similar to that in children with a recto-bulbar urethral fistula. In boys with an abnormal (truncated, malformed, congenitally anomalous, or hemi-) sacrum, one should not be surprised to detect a recto-bladder-neck fistula; these are relatively more complex, higher malformations and usually require a more complex and time-consuming operation, a both posterior sagittal and abdominal approach, because the fistula is not reachable by only the posterior sagittal approach (Fig. 10). However if the sacrum is sufficiently hypoplastic that the rectal pouch and fistula are below the truncated spine, one can approach the repair by the posterior sagittal anorectoplasty only, a much less time-consuming operation. This same principle applies to some boys with a recto-prostatic urethral fistula in which the rectal pouch and fistula are at the level of the tip of the ossified sacrum or just above it; in this situation, the surgeon might resect the coccyx to increase exposure, which might avoid the need for an additional abdominal approach. An additional reason to resect the coccyx and part of the sacrum is the presence of a sacral mass, which can occur as part of the Currarino syndrome, defined by the presence of the triad of hemi-sacrum, anorectal malformation and presacral mass [14].
To summarize, in boys who have a recto-urethral fistula or no fistula with rectal pouches well below the last ossified spinal segment, these malformations usually can be approached operatively by the posterior sagittal approach only, the less complex operation. Boys with a recto-bladder-neck fistula are usually approached operatively by posterior sagittal and abdominal approach, the more complex, time-consuming operation. If the rectal pouch is higher than the last ossified sacral segment, the structure initially encountered by the surgeon might be the urethra, bladder neck, vas deferens, seminal vesicles, or ectopic ureter, which all can be injured inadvertently during the search for the rectum in a boy without a properly performed augmented-pressure distal colostogram. Alternatively, one of these structures could be mistaken for the rectum and dissected and brought to the perineum. This type of surgical misadventure can be avoided with a properly performed high-pressure distal colostogram.
Conclusion
A properly done augmented-pressure distal colostogram performed in boys prior to definitive repair of an anorectal malformation should provide the surgeon with the critical anatomical information necessary to plan for definitive operative repair of these potentially complex malformations, avoiding surgical misadventures that can occur when the anatomy of the recto-urinary connections are not adequately defined preoperatively.
References
Levitt MA, Peña A (2007) Anorectal malformations. Orphanet J Rare Dis 2:33
Peña A (1990) Atlas of surgical management of anorectal malformations. Springer-Verlag, Berlin
Hong AR, Acuna MF, Peña A et al (2002) Urologic injuries associated with repair of anorectal malformations in male patients. J Pediatr Surg 37:339–344
Peña A, Devries PA (1982) Posterior sagittal anorectoplasty: important technical considerations and new applications. J Pediatr Surg 17:796–811
Stephens FD, Smith ED, Paul NW, March of Dimes Foundation (1988) Anorectal malformations in children: update 1988. Liss, New York
Holschneider A, Hutson J, Peña A et al (2005) Preliminary report on the international conference for the development of standards for the treatment of anorectal malformations. J Pediatr Surg 40:1521–1526
Podberesky DJ, Towbin AJ, Eltomey MA et al (2013) Magnetic resonance imaging of anorectal malformations. Magn Reson Imaging Clin N Am 21:791–812
Torres R, Levitt MA, Tovilla JM et al (1998) Anorectal malformations and Down's syndrome. J Pediatr Surg 33:194–197
Gross GW, Wolfson PJ, Peña A (1991) Augmented-pressure colostogram in imperforate anus with fistula. Pediatr Radiol 21:560–562
Mickelson JJ, MacNeily AE, Blair GK (2007) The posterior urethra in anorectal malformations. J Pediatr Surg 42:585–587
Rahalkar MD, Rahalkar AM, Phadke DM (2010) Pictorial essay: distal colostography. Indian J Radiol Imaging 20:122–125
Levitt MAPena A (2014) Imperforate anus and clocal malformations. In: Holcomb GW, Murphy PJ, Ostlie DJ (eds) Ashcraft's pediatric surgery. Saunders Elsevier, Philadelphia, pp 492–514
Peña A (1995) Anorectal malformations. Semin Pediatr Surg 4:35–47
Martucciello G, Torre M, Belloni E et al (2004) Currarino syndrome: proposal of a diagnostic and therapeutic protocol. J Pediatr Surg 39:1305–1311
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Kraus, S.J., Levitt, M.A. & Peña, A. Augmented-pressure distal colostogram: the most important diagnostic tool for planning definitive surgical repair of anorectal malformations in boys. Pediatr Radiol 48, 258–269 (2018). https://doi.org/10.1007/s00247-017-3962-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-3962-2