Abstract
Appendicitis is the most common pediatric surgical emergency. Ultrasound (US) receives the highest appropriate rating scale in children with right lower quadrant pain suspected to have appendicitis. The US exam of the appendix has improved since Puylaert pioneered the technique of graded compression in 1986. In this article, we review ultrasonography of the pediatric appendix as it pertains to the normal appendix, acute appendicitis and the different sonographic manifestations. We also briefly describe technical optimization of image acquisition, common pitfalls and differential diagnoses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Zero radiation profile, zero sedation requirement, and relative low cost make ultrasound (US) the preferred initial imaging study of choice over CT or MRI for the pediatric population. Identifying the normal appendix with US can vary in the pediatric population from 5% to 72% [1, 2]. Variable challenges in the US diagnosis include but are not limited to operator dependency/skill level and patient-specific factors like pain, bowel gas and body mass index (BMI). Having a strong foundation for understanding the technical parameters necessary to optimize quality diagnostic images is, therefore, quite important. When reporting these imaging findings, a US reporting system that incorporates additional and secondary signs is critical, especially in equivocal cases.
Technique
US examination of the appendix is best performed with a 5- to 12-MHz linear transducer. With the child supine, it is helpful to first have the child identify the point of maximal tenderness. One suggestion is to ask the child “Where does it hurt?” just prior to placing the transducer on the child rather than asking the child to “point to where it hurts.” If the child does point, which is more often the case with acute appendicitis, the sonographer should then localize that point as to where to begin the US examination. Rather than point, if the child broadly sweeps his or her hand across the abdomen, appendicitis is less likely to be the source of the discomfort [3]. The sonographer should then gently apply anterior graded compression with the transducer to displace air-filled bowel loops and reduce the distance from the transducer to the appendix, and facilitate identification of the inflamed appendix [3,4,5]. Compression of the transducer should be slowly applied and more pressure can be applied on expiration. In the transverse plane, the psoas muscle and iliac vessels are important landmarks to identify that appropriate compression is being applied [1, 6].
The appendix is most often seen draped over the iliac vessels and located retro-ileal (53%) or subcecal (33%) [7, 8]. If the aforementioned techniques are not successful in visualizing the appendix, one should then identify the non-peristalsing haustrated ascending colon, and then move the probe inferiorly to identify the much smaller compressible peristalsing terminal ileum [1]. The appendix might then be seen separate from the ileum, approximately 10–20 mm inferiorly [1, 6]. If the appendix is still not readily identified, posterior manual compression should be considered and can be helpful in children with large body habitus. This latter technique might further reduce the distance from the transducer to the appendix and improve visualization from 85% with anterior graded compression alone to 95% with both methods [1, 8]. Placing the child in left lateral decubitus position to facilitate placing the cecum and terminal ileum medially can be an additional helpful approach to visualizing the appendix. The sonographer can add cine images to further and more globally illustrate anatomy and areas of interest. At our institution, we also provide routine documentation of the pelvic cul-de-sac and Morrison’s pouch for fluid.
Increased body mass index (BMI), as previously noted, is one of the technical challenges that can limit US visualization of the appendix. The sensitivity in visualizing the appendix decreases from 76% in patients with BMI <25 to 37% in BMI >25 [9]. Hörmann et al. [10] found the appendix in 21% of overweight children, 67% of normal-weight children and 75% of underweight children [9, 10]. Lower-frequency transducers can be helpful by increasing depth penetrance of the ultrasound waves.
Normal appendix
At US, the normal appendix appears as a compressible, blind-ending tubular structure with bowel wall signature and classically measures <6 mm in diameter. This gut signature consists of five distinct layers: outermost echogenic serosal layer, hypoechoic muscularis propria layer, hyperechoic submucosal layer, hypoechoic muscularis mucosal layer, and the innermost hyperechoic mucosal interface (Fig. 1). The hypoechoic mucosal layer contains lymphoid tissue.
Normal appendix. a, b Transverse gray-scale US images with (a) and without (b) compression (COMP) in a 9-year-old girl show the appendix is normal size and compressible. c, d Magnified longitudinal (c) and transverse (d) gray-scale US views of the normal appendix in a 12-year-old boy show alternating echogenicities of the normal layers of the appendiceal wall, including echogenic mucosa (a), hypoechoic muscularis mucosa (b), echogenic submucosa (c), hypoechoic muscularis propria (d) and echogenic serosa (e)
Many studies have evaluated the expected maximal outer diameter measurement of the normal appendix in children. In general, the appendiceal diameter increases by 0.4 mm each year until 6–7 years old and then remains stable [11]. Variability does seem to exist, however, among different studies designed to determine the maximal outer diameter of the normal appendix in pediatric patients [12, 13]. Trout et al. [5] have questioned the utility of having a uniform diameter cutoff for the entire pediatric population by showing that the normal maximal outer diameter of the appendix can measure up to 8.7 mm, with 39% having appendiceal maximal outer diameter measuring >6 mm. Moreover, in children with cystic fibrosis, intraluminal filling of the normal appendix with mucoid content can result in a maximal outer diameter up to 14 mm [14, 15].
An additional US measurement that can supplement data for overall appendiceal measurement is maximal mural thickness (Fig. 2). The maximal mural thickness of the normal appendix is 1.1 mm to 2.7 mm, as compared to normal thickness for small bowel (<2.5 mm) and for colon (<2 mm) [4, 13, 16, 17]. A maximal mural thickness <3 mm should be considered normal in children <6 years [16].
Acute appendicitis, periappendiceal findings and perforation
The etiology of the acutely inflamed appendix is likely multifactorial, the result of a combination of bacterial overgrowth, luminal obstruction and ischemic mucosal damage. Escherichia coli is the most common bacterial culprit, although viral infection such as adenovirus has been reported [18]. The lifetime risk of developing appendicitis is estimated to occur in 8.6% of males and 6.7% of females [4]. Varying reports put the highest incidence of appendicitis at 10–19 years of age [4, 19,20,21]. Multiple studies have shown the specificity of US diagnosis of acute appendicitis to be greater than 90%; however the sensitivity is highly variable, from 40% to 90% [22, 23]. The prevalence of a disease in specific populations changes the positive predictive value of a test, which is reported to be 98%, and the negative predictive value of US for appendicitis, which is 99% [2, 3, 22].
At US, a thickened noncompressible appendix with maximum outer wall diameter greater than 6 mm has 98% sensitivity and specificity of being positive for acute appendicitis (Fig. 3) [2, 11, 23]. The lack of appendiceal compressibility is 96% sensitive and specific for acute appendicitis [2]. Hyperemia is an important marker of inflammatory disease and the inflamed appendiceal wall is variably hyperemic at color Doppler, only 52% sensitive and 96% specific (Fig. 4) [1, 2]. Additionally, diminished flow is specific for ischemia, though not sensitive [24, 25].
Inflammation that rarely localizes to the distal third portion of the appendix is known as tip appendicitis (Fig. 5). The true prevalence of tip appendicitis is unknown but case reports of pathologically proven tip appendicitis suggest the prevalence is as high as 5% [26, 27]. Tip appendicitis can be treated conservatively in a subset of patients with low clinical suspicion for acute appendicitis. Because tip or focal appendicitis can be a cause for false-negative US diagnoses of acute appendicitis, the entire length of the appendix should be carefully evaluated in every case.
Distal tip appendicitis in a 13-year-old girl. a–c Longitudinal linear gray-scale (a), color Doppler (b) and transverse (c) US images show enlarged distal appendix (arrows) with hyperemia at the tip. Note portion of the normal-appearing proximal appendix (arrowheads). Periappendiceal hyperechogenic tissue (asterisks) is also seen
Increased thickening and hyperechogenicity of periappendiceal mesenteric fat is an important and highly specific (98% specificity; 73% sensitivity) recognizable finding for inflammatory disease in the right lower quadrant [7]. Kessler et al. [2] reported that the most accurate periappendiceal finding for acute appendicitis at US was changes in periappendiceal fat, with 91% negative predictive value (NPV) and 76% positive predictive value (PPV). Moderate to large volumes of free abdominopelvic fluid can be specific (98%) for appendicitis but have low sensitivity [1].
Appendiceal perforation, an unfortunate sequela of acute appendicitis, is important to recognize and diagnose early. US performance in detecting perforation has a very low sensitivity (44%) and high specificity (93%) [28]. Rates of perforation tend to be significantly higher in children younger than 8 years (62.5%) than in older children (29.5%) [29]. The mortality rate of appendicitis is close to zero, whereas morbidity rate is 2.7% for nonperforated appendicitis and 16% for perforated appendicitis [30]. Recognizing perforated appendicitis not only changes the clinical management but also the surgical approach. The utility of US in accurately characterizing the severity of disease has been constantly challenged since recent interest in the nonsurgical management of uncomplicated (nonperforated) acute appendicitis has become more prevalent. Diagnosing perforated appendicitis can be particularly challenging when the appendix decompresses as it perforates before a well-defined abscess collection is formed [21]. At US, in addition to periappendiceal fluid, the loss of echogenic submucosal layer is an ancillary sign that can suggest perforation (100% sensitive, 72.7% specific), particularly in children younger than 8 years. Marked mesenteric inflammatory changes and a walled-off fluid collection with mobile internal echoes, with or without foci of gas, would be consistent with abscess (Fig. 6) [29]. The longer the duration of symptoms, presence of appendicolith, increased maximal outer diameter, and periappendiceal fluid are all US findings associated with perforated appendicitis. The presence of complex periappendiceal fluid, however, is the highest predictive US finding associated with perforation [28].
Abscess in a 6-year-old boy with perforated acute appendicitis. Linear gray-scale US shows an enlarged appendix (calipers), with mucosal/submucosal discontinuity at the tip (arrowheads) and localized periappendiceal abscess (ab) containing foci of extra-luminal gas (arrows). Thickened periappendiceal hyperechogenic tissue is again noted (asterisk)
Variable appearances of the appendix at US: differential considerations
To avoid pitfalls it is important to be cognizant of several conditions or findings that can alter the appearance of the appendix at US. The maximal outer diameter of the appendix might be distended secondarily from (a) air, (b) fecal debris, (c) appendicolith, (d) inspissated mucoid content such as in cystic fibrosis patients, (e) mucocele or (f) reactive lymphoid hyperplasia.
Air
Air within the lumen of the appendix with an intact wall and no periappendiceal abnormalities is, in most cases, a normal finding that helps to rule out acute appendicitis (Fig. 7). Alternatively, if periappendiceal abnormalities also exist, air within the appendix can result from communication with a contiguous (air-containing) periappendiceal abscess (Fig. 8). Conversely, the absence of intraluminal air might be helpful to confirm presence of acute appendicitis, especially in cases where US findings are insufficient or misleading [31].
Abscess secondary to perforated appendicitis in an 8-year-old boy. a Transverse color Doppler US of the right lower quadrant shows irregular complex hypoechoic fluid collection containing hyperechoic foci of air along its perimeter (arrows). b Corresponding contrast-enhanced CT, sagittal view, of the lower abdomen shows irregular, rim-enhancing, air-containing abscess (ab) in continuity with enlarged appendix, along with air and appendicolith at its tip (arrow). Bladder (bl)
Fecal debris
Fecal debris within the appendiceal lumen at US is described as heterogeneous hyperechoic intraluminal material without posterior shadowing (Fig. 9) [8, 21, 32]. The appendiceal lumen might be filled entirely, focally, or in a skipped pattern with the fecal matter [21]. Fecal matter in the lumen can increase maximal outer diameter >6 mm and lead to misdiagnosis of acute appendicitis, particularly if maximal outer diameter is the only criterion used. Fecal debris can spontaneously empty but stasis can lead to appendiceal colic.
Normal stool-filled appendix in a 13-year-old boy. a, b Transverse gray-scale US images without (a) and with (b) compression (COMP) show a mildly enlarged, noncompressible appendix containing echogenic stool that distends the mid and distal segments of its lumen. c Longitudinal color Doppler US view shows echogenic stool filling the lumen of the mid and distal appendix. Note absence of appendiceal hyperemia, periappendiceal inflammation or thickened periappendiceal tissue
Appendicolith
Appendicolith is a strongly hyperechogenic structure with posterior shadowing (Fig. 10) within or outside the appendiceal lumen, the latter occurring in instances of perforation. They represent calcified deposits that coalesce and can be seen in both normal and abnormal appendices; hence, when an appendicolith is found, the presence or absence of secondary signs becomes ever so important as part of the overall US evaluation. The presence of an appendicolith and the increased risk of appendicitis is still debated [33]. Blumfield et al. [29] found the presence of an appendicolith in children <8 years of age to be 68% sensitive and 92% specific for acute appendicitis with perforation.
Appendicolith. a US in a 9-year-old boy with acute appendicitis containing an appendicolith. Longitudinal gray-scale US shows enlarged appendix with a large echogenic intraluminal appendicolith (calipers). Note the thickened periappendiceal hyperechogenic tissue (asterisks). b US in a 5-year-old boy with perforated appendicitis with abscess. Gray-scale sagittal US view of lower abdomen shows abscess (ab) containing appendicolith (arrow). BL bladder
Cystic fibrosis
Children with cystic fibrosis, as mentioned, might have an enlarged appendix if inspissated mucoid material distends the lumen; appendiceal diameters average 8.3 mm and extend up to 14.5 mm, with approximately 83% of patients having appendiceal diameters greater than 6 mm (Fig. 11) [14]. The lifetime incidence of acute appendicitis in children with cystic fibrosis is much lower than that of the general population: 2% versus 7%, respectively [14, 34, 35]. However when appendicitis does occur, there is a higher rate of appendiceal perforation and abscess formation in children with cystic fibrosis than in the general population [14, 34].
Enlarged appendix in an 11-year-old girl with cystic fibrosis. a–c Longitudinal linear gray-scale (a) and transverse (b, c) US views without (b) and with (c) compression (com) show an enlarged 1-cm (arrows) noncompressible appendix (calipers), with heterogeneous echogenic mucoid material distending the lumen (L). Note absence of periappendiceal inflammation or thickened periappendiceal tissue
Mucocele
Mucocele of the appendix is rare (seen in 0.25% of appendectomy specimens) and commonly found incidentally in elective cases [33, 36] but can arise from benign (e.g., simple mucocele) to malignant (e.g., mucinous cystadenocarcinoma) etiology. These are rarely seen in children and more often in adults with persistent fluid-filled appendix on multiple US or CT scans (Fig. 12). Rarely, mucocele of the appendiceal stump develops in children with a history of appendectomy presenting with right lower quadrant pain.
Reactive lymphoid hyperplasia
Reactive lymphoid hyperplasia of the appendix can affect the appendix in similar fashion to lymphoid tissue elsewhere in the body in response to infections (e.g., mononucleosis, upper respiratory infection). In children ages 1–10 years, mucosa-associated lymphoid tissue occupies up to 30% of the appendiceal wall and later diminishes. At US, lymphoid hyperplasia of the appendix characteristically results in thickening of the hypoechoic mucosal layer that contains lymphoid tissue (Fig. 13) [21, 37].
Differential considerations for non-appendiceal right lower quadrant pain
When right lower quadrant pain is not attributable to the appendix, further evaluation for the surrounding structures is warranted. The differential list can be lengthy and should be age-specific as well as gender-specific. Entities within the scope of this discussion are (a) primary mesenteric adenitis, (b) inflammation and infection and (c) Meckel diverticulum. Other considerations for right lower quadrant pain include typhlitis, intussusception, pyelonephritis, urolithiasis, foreign body ingestion and gender-specific entities (e.g., pelvic inflammatory disease, ovarian cyst, ovarian torsion or ovarian mass), and these are not discussed here.
Primary mesenteric adenitis
Primary mesenteric adenitis is a common alternative diagnosis in children imaged for appendicitis [38, 39]. While the entity is a diagnosis of exclusion, it is also a controversial diagnosis. Enlarged mesenteric lymph nodes can be seen secondarily in a multitude of reactive, inflammatory and infectious processes. Mesenteric lymph nodes are borderline to mildly enlarged (>5 mm short axis) and clustered (more than three) in the small-bowel mesentery or anterior to the psoas muscle without identifiable acute inflammatory condition [40,41,42]. Some authors consider lymphadenopathy as pathological if the longest diameter measures >10 mm or short axis >8 mm [42, 43].
Inflammation and infection
Inflammation and infection incorporate entities that can locally involve the ileocecal region and result in secondary appendiceal inflammation. Pelvic inflammatory disease can secondarily inflame the appendix. Acute flares of Crohn disease involving the terminal ileum and cecum can lead to secondary appendiceal enlargement and inflammation (Fig. 14); however isolated involvement of the appendix in the setting of a Crohn flare is uncommon [33]. Infectious ileocolitis is a common clinical condition with symptoms similar to viral gastroenteritis. These symptoms can present acutely, making it indistinguishable from appendicitis, particularly if the infection is by Yersinia enterocolitica, Campylobacter jejuni or Salmonella enteritidis [41].
Differential diagnosis: Crohn disease in a 16-year-old girl. a–c Longitudinal (a) and transverse (b, c) gray-scale US images without (b) and with (c) compression of the appendix (arrows) show noncompressibilty of the thickened, enlarged (1.2 cm) appendix (calipers) containing a small amount of intraluminal air. TI terminal ileum. d, e Corresponding oral-contrast-enhanced CT images in the coronal reconstructed view show thickened terminal ileum (arrowheads) and ileocecal valve (arrows) with narrowing of the ileal lumen; (e) also note the thickened, enlarged appendix (arrows) anterior to iliac vessels
Meckel diverticulum
Meckel diverticulum classically presents as painless rectal bleeding but can mimic appendicitis when inflamed. Meckel diverticulitis can have similar findings to those of acute appendicitis — as a blind-ending, noncompressible hyperemic structure with diameters of 8–12 mm but arising from the distal ileum [38, 44]. At US, a normal appendix should be separately found.
Reporting the right lower quadrant ultrasound examination
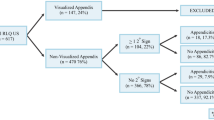
Binary US interpretation of the appendix as being either normal or acute appendicitis is not often experienced in day-to-day practice and accuracy might not be as high as reported in clinical studies [3, 45, 46]. When the examiner fails to identify the appendix, appendicitis is present in up to 33% of equivocal cases and 3% of negative cases [45]. Clinical suspicion based on history and physical diagnosis then plays a more important role in these equivocal cases. Additional imaging might be warranted if clinical suspicion is intermediate to low. Having a non-binary interpretive reporting scheme increases diagnostic accuracy of acute appendicitis [45].
A multivariate interpretive scheme that includes periappendiceal findings can increase the diagnostic accuracy from 94.1% to 96.8% [45]. These findings include mesenteric fat hyperechogenicity, free fluid, thickened terminal ileum or cecum, fluid collection and hypoperistalsis. The secondary signs alone, such as pericecal fat inflammatory changes, might be enough to diagnose acute appendicitis [13]. An example of the reporting document provided at our institution is shown (Fig. 15).
Conclusion
Graded-compression US is a valuable tool to diagnose acute appendicitis. Visualizing the appendix by techniques, along with an awareness of the variations in the US appearance of the appendix detailed in this paper, greatly increases the negative predictive value in diagnosing acute appendicitis. Having a reporting system that includes both appendiceal and periappendiceal findings increases diagnostic accuracy and improves communication with referring clinical services.
References
Janitz E, Naffaa L, Rubin M, Ganapathy SS (2016) Ultrasound evaluation for appendicitis focus on the pediatric population: a review of the literature. J Am Osteopath Coll Radiol 5:5–14
Kessler N, Cyteval C, Gallix B et al (2004) Appendicitis: evaluation of sensitivity, specificity, and predictive values of US, Doppler US, and laboratory findings. Radiology 230:472–478
Strouse PJ (2010) Pediatric appendicitis: an argument for US. Radiology 255:8–13
Puig S, Staudenherz A, Felder-Puig R et al (2008) Imaging of appendicitis in children and adolescents: useful or useless? A comparison of imaging techniques and a critical review of the current literature. Semin Roentgenol 43:22–28
Trout AT, Sanchez R, Ladino-Torres MF et al (2012) A critical evaluation of US for the diagnosis of pediatric acute appendicitis in a real-life setting: how can we improve the diagnostic value of sonography? Pediatr Radiol 42:813–823
Sivitz AB, Cohen SG, Tejani C (2014) Evaluation of acute appendicitis by pediatric emergency physician sonography. Ann Emerg Med 64:358–364
Min WL, Kim YJ, Hae JJ et al (2009) Sonography of acute right lower quadrant pain: importance of increased intraabdominal fat echo. AJR Am J Roentgenol 192:174–179
Lee JH, Jeong YK, Park KB et al (2005) Operator-dependent techniques for graded compression sonography to detect the appendix and diagnose acute appendicitis. AJR Am J Roentgenol 184:91–97
Josephson T, Styrud J, Eriksson S (2000) Ultrasonography in acute appendicitis. Body mass index as selection factor for US examination. Acta Radiol 41:486–488
Hörmann M, Scharitzer M, Stadler A et al (2003) Ultrasound of the appendix in children: is the child too obese? Eur Radiol 13:1428–1431
Trout AT, Towbin AJ, Zhang B (2014) The pediatric appendix: defining normal. AJR Am J Roentgenol 202:936–945
Ozel A, Orhan UP, Akdana B et al (2011) Sonographic appearance of the normal appendix in children. J Clin Ultrasound 39:183–186
Wiersma F, Toorenvliet BR, Bloem JL et al (2009) US examination of the appendix in children with suspected appendicitis: the additional value of secondary signs. Eur Radiol 19:455–461
Lardenoye SW, Puylaert JB, Holscher HC (2004) Appendix in children with cystic fibrosis: US features 1. Radiology 232:187–189
Menten R, Lebecque P, Saint-Martin C et al (2005) Outer diameter of the vermiform appendix: not a valid sonographic criterion for acute appendicitis in patients with cystic fibrosis. AJR Am J Roentgenol 184:1901–1903
Simonovský V (2002) Normal appendix: is there any significant difference in the maximal mural thickness at US between pediatric and adult populations? Radiology 224:333–337
Anupindi SA, Halverson M, Khwaja A et al (2014) Common and uncommon applications of bowel ultrasound with pathologic correlation in children. AJR Am J Roentgenol 202:946–959
Lamps LW (2010) Infectious causes of appendicitis. Infect Dis Clin N Am 24:995–1018
Flum D (2015) Clinical practice: acute appendicitis — appendectomy or the “antibiotics first” strategy. N Engl J Med 20372:1937–1943
Harris A, Bolus NE (2011) Appendicitis imaging. Radiol Technol 77:111–117
Park NH, Oh HE, Park HJ et al (2011) Ultrasonography of normal and abnormal appendix in children. World J Radiol 3:85–91
Baldisserotto M, Marchiori E (2000) Accuracy of noncompressive sonography of children with appendicitis according to the potential positions of the appendix. AJR Am J Roentgenol 175:1387–1392
Taylor GA (2004) Suspected appendicitis in children: in search of the single best diagnostic test. Radiology 231:293–295
Maturen KE, Wasnik AP, Kamaya A et al (2011) Ultrasound imaging of bowel pathology: technique and keys to diagnosis in the acute abdomen. AJR Am J Roentgenol 197:1067–1075
Ripollés T, Martínez MJ, Morote V et al (2006) Appendiceal involvement in Crohn’s disease: gray-scale sonography and color Doppler flow features. AJR Am J Roentgenol 186:1071–1078
Mazeh H, Epelboym I, Reinherz J et al (2009) Tip appendicitis: clinical implications and management. Am J Surg 197:211–215
Johansson EP, Rydh A, Riklund KA (2007) Ultrasound, computed tomography, and laboratory findings in the diagnosis of appendicitis. Acta Radiol 48:267–273
Carpenter JL, Orth RC, Zhang W et al (2016) Diagnostic performance of US for differentiating perforated from nonperforated pediatric appendicitis: a prospective cohort study. Radiology 282:160–175
Blumfield E, Nayak G, Srinivasan R et al (2013) Ultrasound for differentiation between perforated and nonperforated appendicitis in pediatric patients. AJR Am J Roentgenol 200:957–962
Hartwich J, Luks FI, Watson-Smith D et al (2016) Nonoperative treatment of acute appendicitis in children: a feasibility study. J Pediatr Surg 51:111–116
Rettenbacher T, Hollerweger A, Macheiner P et al (2000) Presence or absence of gas in the appendix: additional criteria to rule out or confirm acute appendicitis –– evaluation with US. Radiology 214:183–187
Rioux M (1992) Sonographic normal and detection abnormal of the appendix. AJR Am J Roentgenol 158:773–778
Dietz KR, Merrow AC, Podberesky DJ et al (2013) Beyond acute appendicitis: imaging of additional pathologies of the pediatric appendix. Pediatr Radiol 43:232–242
McCarthy VP, Mischler EH, Hubbard VS et al (1984) Appendiceal abscess in cystic fibrosis. A diagnostic challenge. Gastroenterology 86:564–568
Chaudry G, Navarro OM, Levine DS et al (2006) Abdominal manifestations of cystic fibrosis in children. Pediatr Radiol 36:233–240
Pickhardt PJ, Levy AD, Rohrmann CA et al (2003) Primary neoplasms of the appendix: radiologic spectrum of disease with pathologic correlation. Radiographics 23:645–662
Xu Y, Brooke Jeffrey R, DiMaio MA et al (2016) Lymphoid hyperplasia of the appendix: a potential pitfall in the sonographic diagnosis of appendicitis. AJR Am J Roentgenol 206:189–194
Sung T, Callahan MJ, Taylor GA (2006) Clinical and imaging mimickers of acute appendicitis in the pediatric population. AJR Am J Roentgenol 186:67–74
Carty HML (2002) Paediatric emergencies: non-traumatic abdominal emergencies. Eur Radiol 12:2835–2848
Fox JC, Boysen M, Gharahbaghian L et al (2011) Test characteristics of focused assessment of sonography for trauma for clinically significant abdominal free fluid in pediatric blunt abdominal trauma. Acad Emerg Med 18:477–482
Purysko AS, Remer EM, Filho HML et al (2011) Beyond appendicitis: common and uncommon gastrointestinal causes of right lower quadrant abdominal pain at multidetector CT. Radiographics 31:927–947
Karmazyn B, Werner EA, Rejaie B et al (2005) Mesenteric lymph nodes in children: what is normal? Pediatr Radiol 35:774–777
Sanchez TR, Corwin MT, Davoodian A et al (2016) Sonography of abdominal pain in children: appendicitis and its common mimics. J Ultrasound Med 35:627–635
Peletti AB, Baldisserotto M (2006) Optimizing US examination to detect the normal and abnormal appendix in children. Pediatr Radiol 36:1171–1176
Larson DB, Trout AT, Fierke SR et al (2015) Improvement in diagnostic accuracy of ultrasound of the pediatric appendix through the use of equivocal interpretive categories. AJR Am J Roentgenol 204:849–856
Godwin BD, Drake FT, Simianu VV et al (2015) A novel reporting system to improve accuracy in appendicitis imaging. AJR Am J Roentgenol 204:1212–1219
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no financial interests, investigational or off-label uses to disclose.
Rights and permissions
About this article
Cite this article
Gongidi, P., Bellah, R.D. Ultrasound of the pediatric appendix. Pediatr Radiol 47, 1091–1100 (2017). https://doi.org/10.1007/s00247-017-3928-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-3928-4