Abstract
Background
Musculoskeletal US is a noninvasive imaging method for diagnosing and monitoring inflammatory rheumatic diseases.
Objectives
To develop age- and gender-related arthrosonographic reference intervals for the hip joint of healthy children and adolescents.
Materials and methods
In a cross-sectional US study, we examined both hip joints of 445 children and adolescents with an age range of 1 year to 18 years. We measured the distance between the bone surface and the outer margin of the joint capsule to define the bone-capsule distance, the joint capsule and cartilage thickness, and the capsule layer thickness. Reference values were calculated. The shape of the joint capsule and bone-capsule junction zone were analyzed qualitatively. An intraobserver analysis was performed.
Results
Bone-capsule distance, capsule thickness and the anterior capsule layer increase with age. In contrast, joint cartilage decreases. The posterior capsule layer exhibited constant thickness across all age groups. The difference between both body sides and gender was collectively less than 0.5 mm. The intraobserver variations were within the calculated reference intervals. The insertion of the capsule to the bone was mostly a peaked one. The capsule shape had a convex or straight configuration in a neutral position and a concave position during outward rotation. The intraobserver analysis revealed good to very good concordance.
Conclusion
We propose age- and gender-related reference intervals for the bone-capsule distance, joint capsule and cartilage thickness of the hip.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal US has been shown to be one of the best imaging modalities for diagnosing and monitoring inflammatory rheumatic diseases in children and adolescents with juvenile idiopathic arthritis [1] and for evaluating joint effusions and septic arthritis. This method has several obvious advantages to other imaging methods when applied in paediatric patients, such as its noninvasive nature, lack of ionizing radiation, lack of need for sedation, possibility of a real-time assessment of an arbitrary number of joints and feasibility of a bedside examination [2]. Compared with MRI, US exhibits acceptable agreement when measuring hyaline articular cartilage in healthy children and adolescents [2].
Arthrosonography is superior in detecting joint inflammation and in assessing the extent of joint involvement, and therefore it has the ability to modify a patient’s disease classification. Subclinical disease activity can be discovered better with arthrosonography than with clinical examination, especially in the hip joint [3,4,5,6,7,8,9], as clinical examination reaches its limits by virtue of the deeper localization of the hip joint in contrast to other joints [10, 11]. However, in contrast to adults, there is a lack of age-specific reference values for children and adolescents [3, 12]. Because the adult skeleton is different, varying degrees of unossified hyaline cartilage and secondary ossification centres can be found in the epiphysis. With increasing age, there are age-dependent relations between the unossified hyaline cartilage in the epiphyses and the growing secondary ossification centres that are present from 1 year of age [13, 14]. At the age of 17-19 years, at the end of the ossification process in the femoral head, only a small portion of the hyaline cartilage is left, which forms the articular cartilage. As these age-specific changes impede the interpretation and differentiation of physiological and pathological imaging findings, normal values are needed [3, 11]. Therefore, the aim of our study was to establish age-related normal values for the hip joint by a multicentre arthrosonography study.
Materials and methods
All procedures performed in studies involving humans were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study obtained ethical approval by the ethics committee of the Justus-Liebig University Giessen, Department of Medicine, Giessen, Hessen, Germany (file number 114/12). Informed consent was obtained from all participants included in the study. Additional informed consent was obtained from all participants for whom identifying information is included in this article. The Imaging Working Group of the German Society of Rheumatology in Childhood and Adolescence performed this prospective, multicentre arthrosonography study of the hip joint in healthy children and adolescents.
Study sample
Children were recruited among family and friends of the investigators, children who visited the outpatient clinics to receive vaccinations or school medical check-ups and from patients of children’s hospitals who did not have a rheumatic disease or any other disease with signs or symptoms of arthritis or arthralgia in their clinical history. The caregivers and children were questioned concerning any joint pain in the last 6 months. A positive answer resulted in exclusion from the study. None of the children had received nonsteroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen or indomethacin) or corticosteroids for at least 6 months before the arthrosonography was performed. A paediatrician with a minimum of 10 years of experience as a rheumatologist performed a joint evaluation to exclude any joint pathology before the US examination.
Ultrasound examination
The US setting and the procedure for the examination were standardized in all participating centres. In some study centres, both clinical and US examinations were performed by the same paediatric rheumatologist. To exclude any bias, all investigators were trained together to gain a nearly uniform US examination prior to the beginning of the study. All US examinations were performed by paediatric rheumatologists are: Hartwig Lehmann (HL), Daniel Windschall (DW), Gerd Ganser (GG), Rainer Berendes (RB), Maria Haller (MH), Manuela Krumrey-Langkammerer (MKL), Katharina Palm-Beden (KPB), Antje Nimtz-Talaska (ANT), Christine Nirschl (CN), Phillip Schoof (PS), Ralf Trauzeddel (RT) with a minimum of 10 years of experience in arthrosonography. Standard scans were chosen as described in the literature [10]. All measurements were performed in real time. All acquired images were stored on a picture archiving communication system workstation at each centre. The archived pictures and measurements were reviewed by two paediatric rheumatologists are Ralf Trauzeddel (RT) and Daniel Windschall (DW) with more than 10 years of experience in arthrosonography. Only those measurements that achieved a consensus were considered for final analysis. We used different US machines: Philips HD 11 (L12-5 MHz, Amsterdam, Netherlands), GE Logiq S8 (L6-15, Boston, Massachusetts, USA), Toshiba Xario XG (PLT-1204AX, Minato, Tokio, Japan), Siemens Acuson S2000 (L9-4, 18 L6, Erlangen, Bavaria, Germany), Siemens Sonoline G40 (L9-5) and Esaote MyLab 60 (LA522E, Genova, Liguria, Italy). Grey-scale B-mode US examinations were performed with linear probes with a minimum of 7 MHz. In most examinations, a minimum of 9 MHz was used. It was sometimes necessary in obese patients to reduce the frequency to 7 MHz. Not all parameters could be examined because not all anatomical structures could be displayed in all age groups or due to termination of the examination by the study participants or the legal guardians.
Standard sonograms
Using an anterior longitudinal scan, the joint cavity dimension was determined by measuring the maximum distance between the bone surface and outer border of the joint capsule perpendicular to the bone surface in a neutral position as well as an outward rotation of the hip joint. We defined this parameter as the bone-capsule distance. Previous studies defined this anatomical structure as the anterior capsular distance [15, 16]. Additionally, the anterior and posterior capsule thicknesses were measured if they were definable. The insertion of the capsule to the bone was qualitatively evaluated as peaked or round. The shape of the capsule was classified as convex, concave or straight using the neutral position as well as an outward rotation of the hip joint. The cartilage and capsule thicknesses were measured on an anterior transverse scan. The position of the transducer and the landmarks of measurements are shown in Figs. 1 and 2.
Standard longitudinal hip sonograms and measurements in a 13-year-old girl. a Anterior longitudinal scan of the hip joint in an outward rotation demonstrates the joint capsule (arrowheads), the capsule-bone distance (double arrow), the posterior capsule (arrow), the anterior capsule (open arrowhead) and insertion of the capsule to the bone (asterisk). b Anterior longitudinal scan of the hip joint in a neutral position shows the joint capsule (arrowheads) and the capsule-bone distance (double arrow)
Intra- and interobserver analysis
One investigator examined ten children on two consecutive days with no knowledge of the child’s measurements the day before. The ten children were examined after closing the reference value survey and were therefore not included. A small interobserver analysis was performed by three observers were Ralf Trauzeddel (RT), Daniel Windschall (DW) and Hartwig Lehmann (HL) with 15 years of experience each examining three children. Because of the small sample size in this analysis we decided not to report the results.
Statistical analysis
MedCalc Statistical Software version 14.12.0 (MedCalc Software bvba, Ostend, Belgium) and SPSS version 22 (IBM, Armonk, US) were used for statistical analysis. Categorical data are expressed as the means, and nominal and ordinal data are expressed as absolute values and percentages. Data were reviewed for outliers by visualization of box plots and were tested using the method described by Reed et al. [17]. Any outliers were excluded from further analysis. The Kolmogorov-Smirnov test was used to test for normal distribution. If the data were not normally distributed, a logarithmic transformation was applied. We calculated 95% reference intervals using a robust method described in the Clinical and Laboratory Standards Institute guidelines [18]. To calculate age-related reference intervals, we applied a weighted polynomial regression model. For the polynomial model, we selected a power of 1 for the mean and standard deviation. We plotted the graphs using the mean and the 2.5 and 97.5 centiles. The intraobserver analysis of categorical data was calculated for the capsule-bone distance in neutral position for the left and right hip joint using average measures in a two-way mixed model with absolute agreement. The mean and standard deviations are given. Nominal and ordinal data were assessed using the kappa method. To compare the joints on both sides in the study population, we used a Wilcoxon test with non-parametric data sets and a paired samples t-test in parametric data sets. To compare the joints between both genders, we used a Mann-Whitney U test in non-parametric data sets and an independent samples t-test in parametric data sets. A correlation analysis was performed using Spearman’s correlations. A P-value <0.05 was statistically significant.
Results
The study participants were 1 year to 18 years old. A total of 445 children (201 boys, 244 girls) and, therefore, 890 joints were examined with B-mode grey-scale sonography in 9 participating centres across Germany.
Normative values
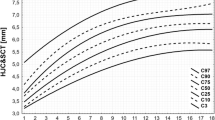
Age-related reference intervals are displayed in Fig. 3 for girls and in Fig. 4 for boys. Boys and girls differed significantly in the bone-capsule distance in a neutral position on the left and right-side (P=0.0026 and P=0.0278, respectively), the cartilage thickness on the left and right-side (P<0.0001) and the capsule thickness and bone-capsule distance in an outward rotation on the left-side (P=0.0211 and P=0.0122, respectively). The left and the right body side differed significantly in cartilage thickness (P=0.0003) and bone-capsule distance in an outward rotation (P=0.0002). The difference between both body sides and both genders was collectively less than 0.5 mm.
Age-related reference intervals of the hip joint in girls. The upper and lower lines indicate the 5th and 95th centiles. The middle line indicates the mean. a Capsule-bone distance in a neutral position of the left hip joint. b Capsule-bone distance in an external rotation of the left hip joint. c Capsule thickness of the left hip joint. d Cartilage thickness of the left hip joint. e Capsule-bone distance in a neutral position of the right hip joint. f Capsule-bone distance in an external rotation of the right hip joint. g Capsule thickness of the right hip joint. h Cartilage thickness of the right hip joint
Age-related reference intervals of the hip joint in boys. The upper and lower lines indicate the 5th and 95th centiles. The middle line indicates the mean. a Capsule-bone distance in a neutral position of the left hip joint. b Capsule-bone distance in an external rotation of the left hip joint. c Capsule thickness of the left hip joint. d Cartilage thickness of the left hip joint. e Capsule-bone distance in a neutral position of the right hip joint. f Capsule-bone distance in an external rotation of the right hip joint. g Capsule thickness of the right hip joint. h Cartilage thickness of the right hip joint
The bone-capsule distance in a neutral position was significantly larger than in an outward rotation (P<0.0001) by approximately 1 mm. The difference in thickness of the anterior and posterior capsule was also significant (P<0.0001). The posterior capsule thickness was not correlated on the left-side (P=0.2932) and only a marginal correlation on the right-side (r=0.148, P=0.0450).
We conducted correlation analyses to test for change across age. The anterior capsule thickness (left: r=0.445 and right: r=0.415), the overall capsule thickness (left: r=0.265 and right: r=0.276) and the bone-capsule distance in a neutral position (left: r=0.458 and right: r=0.421) and in an outward rotation (left: r=0.478 and right: r=0.479) had low positive correlations with age (all P<0.0001). The cartilage thickness had an inverse high correlation with age (left: r=−0.791 and right: r =−0.746, both P<0.0001).
Qualitative grading of joint anatomy
The qualitative grading of the capsule shape and the insertion of the capsule to the bone are shown in Fig. 5. In most children, the insertion of the capsule to the bone was peaked. In a neutral position, the shape of the capsule in girls and boys was mostly convex or straight. This shape changed to concave when the hip joint was placed in an outward rotation.
Intraobserver analysis
The mean and two standard deviations for the left and right-side are wli=0.4±0.72 mm and wre=0.5±0.78 mm, respectively. The intraobserver variations were within the reference intervals. The quadratic mean of the left and right-side is 6.6±1.3 mm with a relative difference of 20%.
Discussion
To the best of our knowledge, this study is the first to include age-dependent reference values of hip joint anatomy of healthy children for fixed age intervals. Previous studies have also published reference values for the bone-capsule distance and the anterior and posterior capsule layers. These studies summarized their respective reference values over a wide range of ages [6, 15, 19, 20] and only grouped large age variances together in different groups [16, 21] or correlated anatomical measurements with body height and not age [22].
Previous studies summarizing their measurements over all ages were in good agreement with our bone-capsule distance results [15, 19, 20]. However, Friedman and colleagues [6] found a mean bone-capsule distance of 0.43±0.08 cm in healthy children and of 0.60±0.16 cm in patients with juvenile rheumatoid arthritis. The study participants had a mean age of 10.2 and 10.4 years, respectively. These values are out of range for our established references. However, the authors measured the distance between the femoral neck and posterior border of the capsule, whereas we chose the anterior border. Rohrschneider et al. [22] already noted this discrepancy and proposed the use of the anterior border as it seems to be more distinct than the posterior border due to the attachment of the synovial membrane.
Terjesen and colleagues [16] examined 58 patients with one-sided transient synovitis and combined them into three age groups (2-3 years, 4-7 years and ≥8 years). They measured the affected and unaffected body sides and used the latter to obtain reference values. The first two age groups described and clearly defined were in agreement with our results. Collado et al. [21] described wider age groups (2-5 years, 6-10 years and 11-16 years). Likewise, Friedman et al. [6] and Robben et al. [19] also found no correlation between the bone-capsule distance and age. This result contrasts our results and others published in the literature [16, 22].
We tried to differentiate the anterior and posterior layers of the joint capsule as others have tried before [19]. However, we only could discriminate these two structures up to the age of 12 years old in most cases. The anterior layer was significantly thicker than the posterior layer. Robben and colleagues [19] have described this finding before. However, they could not show that an increase in layer thickness was evident in symptomatic hip joints. Further research is needed to determine the value of these structures in disease assessment.
Previous descriptions of reference values have been inconsistent as to whether to measure the bone-capsule distance and whether to assess the capsule shape in neutral position or external rotation. Rohrschneider et al. [22] performed their measurements in both positions and found a mean difference of 1 mm for the bone-capsule distance, which is consistent with our results. They found no significant difference between both measurements in contrast to our study.
Their capsule shape was always convex in a neutral position and changed to a concave shape when the hip was rotated externally [22]. The majority of the capsule shapes were also convex in a neutral position in our study. Therefore, we think that the hip should be rotated externally during a US examination to avoid the impression of an effusion as a bulging joint capsule.
Limitations of the study
One limitation is the use of different US systems, which resulted in different image quality. This shortcoming was minimized by the extensive review process described in the methods. A major limitation is the small interobserver analysis, which is therefore not documented in this article.
Conclusion
We propose age- and sex-related reference intervals for the bone-capsule distance and joint capsule and cartilage thicknesses in 445 children (890 joints).
References
Ramos PC, Ceccarelli F, Jousse-Joulin S (2012) Role of ultrasound in the assessment of juvenile idiopathic arthritis. Rheumatology (Oxford) 51:vii10–vii12
Spannow AH, Stenboeg E, Pfeiffer-Jensen M et al (2011) Ultrasound and MRI measurements of joint cartilage in healthy children: a validation study. Ultraschall Med 32:S110–S116
Colebatch-Bourn AN, Edwards CJ, Collado P et al (2015) EULAR-PReS points to consider for the use of imaging in the diagnosis and management of juvenile idiopathic arthritis in clinical practice. Ann Rheum Dis 74:1946–1957
Eich GF, Halle F, Hodler J et al (1994) Juvenile chronic arthritis: imaging of the knees and hips before and after intraarticular steroid injection. Pediatr Radiol 24:558–563
Frosch M, Foell D, Ganser G, Roth J (2003) Arthrosonography of hip and knee joints in the follow up of juvenile rheumatoid arthritis. Ann Rheum Dis 62:242–244
Friedman S, Gruber MA (2002) Ultrasonography of the hip in the evaluation of children with seronegative juvenile rheumatoid arthritis. J Rheumatol 29:629–632
Silva VB, Faquin G, Nicacio A et al (2013) Association between the ultrasonographic and clinical findings in the hips of patients with juvenile idiopathic arthritis. Rev Bras Reumatol 53:322–327
Collado P, Jousse-Joulin S, Alcalde M et al (2012) Is ultrasound a validated imaging tool for the diagnosis and management of synovitis in juvenile idiopathic arthritis? A systematic literature review. Arthritis Care Res (Hoboken) 64:1011–1019
Haslam KE, McCann LJ, Wyatt S, Wakefield RJ (2010) The detection of subclinical synovitis by ultrasound in oligoarticular juvenile idiopathic arthritis: a pilot study. Rheumatology (Oxford) 49:123–127
Backhaus M, Burmester G-R, Gerber T et al (2001) Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis 60:641–649
Magni-Manzoni S, Collado P, Jousse-Joulin S et al (2014) Current state of musculoskeletal ultrasound in paediatric rheumatology: results of an international survey. Rheumatology (Oxford) 53:491–496
Schmidt WA, Schmidt H, Schicke B, Gromnica-Ihle E (2004) Standard reference values for musculoskeletal ultrasonography. Ann Rheum Dis 63:988–994
Roth J, Jousse-Joulin S, Magni-Manzoni S et al (2015) Definitions for the sonographic features of joints in healthy children. Arthritis Care Res (Hoboken) 67:136–142
Kemperdick H (1996) Skelettentwicklung (Wachstum, Reifung des Skeletts, Knochenalter- und Endgrößenbestimmung. In: Kinderradiologie, vol 2. Springer Berlin Heidelberg, Berlin Heidelberg, pp 79–99
Laurell L, Hochbergs P, Rydholm U, Wingstrand H (2002) Capsular distance in the hip of the healthy child - normal values with sonography and MR imaging. Acta Radiol 43:213–216
Terjesen T, Osthus P (1991) Ultrasound in the diagnosis and follow-up of transient synovitis of the hip. J Pediatr Orthop 11:608–613
Reed AH, Henry RJ, Mason WB (1971) Influence of statistical method used on the resulting estimate of normal range. Clin Chem 17:275–284
Clinical and Laboratory Standards Institute (2008) Defining, establishing and verifying reference intervals in the clinical laboratory; approved guideline - third edition. CLSI document C28-A3. Clinical and Laboratory Standards Institute, Wayne, PA
Robben SG, Lequin MH, Diepstraten AF et al (1999) Anterior joint capsule of the normal hip and in children with transient synovitis: US study with anatomic and histologic correlation. Radiology 210:499–507
Egund N, Wingstrand H, Forsberg L et al (1986) Computed tomography and ultrasonography for diagnosis of hip joint effusion in children. Acta Orthop 57:211–215
Collado P, Naredo E, Calvo C, Crespo M (2007) Assessment of the joint recesses and tendon sheaths in healthy children by high-resolution B-mode and power Doppler sonography. Clin Exp Rheumatol 25:915–921
Rohrschneider WK, Fuchs G, Tröger J (1996) Ultrasonographic evaluation of the anterior recess in the normal hip: a prospective study on 166 asymptomatic children. Pediatr Radiol 26:629–634
Acknowledgements
We thank the children and adolescents and their parents who took part in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
This study was supported by a grant from Pfizer Pharma. The funder had no involvement in the study design, in the collection, analysis and interpretation of the data, in the writing of the report or in the decision to submit the paper for publication. The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Trauzeddel, R.F., Lehmann, H., Windschall, D. et al. Age-dependent arthrosonographic reference values of the hip joint in healthy children and adolescents – a cross-sectional multicenter ultrasound study. Pediatr Radiol 47, 1329–1336 (2017). https://doi.org/10.1007/s00247-017-3862-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-3862-5