Abstract
Background
Colonic volvulus is rare in children and associated with colonic dysmotility. Diagnosis of colonic volvulus on radiographs in these patients can be challenging. The purpose of the study was to identify the accuracy of abdominal radiographs and findings suggestive of colonic volvulus.
Materials and methods
A retrospective (2003- 2014) study of all children with colonic volvulus proven surgically or endoscopically reviewed their medical charts for underlying disease and clinical presentation as well as their original radiograph reports. Two pediatric radiologists (reader 1 and reader 2) independently reviewed the radiographs. The kappa test was used to evaluate interobserver variability.
Results
There were 19 cases of colonic volvulus in 18 patients (11 males) a mean age 14 years. Cecal volvulus was the most common finding at 14/19 cases (74%). Sixteen of 18 (89%) patients had neurological impairment and 10 of 18 (56%) had intestinal dysmotility. The most common presentation was abdominal distension (14/19 [74%]) and pain (11/19 [58%]). Colonic volvulus was diagnosed in only 7/16 (44%) of the abdominal radiographs. The specific finding of a coffee-bean sign was retrospectively observed only by reader 2 in two cases. Absence of rectal gas and focal colonic loop dilation were the most common findings by the readers (average 73.5% and 87%, respectively) with Kappa values of 0.3 and 0.38, respectively.
Conclusion
Diagnosis of colonic volvulus in children can be challenging. Radiologists should be alerted to the possibility of colonic volvulus when there is focal colonic loop distention or absent rectal gas.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In adults, colonic volvulus was reported in 1.9% of all cases of bowel obstructions in the United States [1]. However, colonic volvulus is only rarely seen in children. In 1994, Mellor and Drake [2] reported only 14 cases of colonic volvulus in children from their institution over 37 years (1955-1992). Prompt diagnosis is necessary because, if untreated, colonic volvulus may result in bowel wall necrosis, perforation, peritonitis and possibly death [3].
In adults, colonic volvulus is thought to be secondary to a long mesentery with a narrow base of fixation to the retroperitoneum and elongated, redundant bowel with the sigmoid colon most commonly affected [4]. Other etiologies include prolonged recumbency and chronic constipation as seen in nursing home patients and those with neuropsychiatric disease [5, 6].
Few small series on children demonstrated the association between colonic volvulus and neurological and intestinal motility disorders [5, 6]. From our experience, most of the children with colonic volvulus had predisposing intestinal motility disorders typically from neurological problems. It is particularly challenging for patients with neurological disorders and mental disability to verbalize their symptoms [7]. These children commonly present with abdominal symptoms and are typically evaluated first with abdominal radiographs. In many of these patients, the baseline abdominal radiographs are abnormal and demonstrate various degrees of bowel distension [5]. The diagnosis of colonic volvulus with abdominal radiography in these children can, therefore, be challenging.
We were interested in sharing our experience with diagnosing colonic volvulus in children and evaluating the accuracy of abdominal radiography in suggesting the diagnosis. We also wanted to determine if there are any radiographic signs that could help radiologists reliably differentiate between intestinal dysmotility and colonic volvulus.
Materials and methods
Patient population
This was a HIPAA-compliant retrospective study approved by our institutional review board with waiver of informed consent. At a tertiary-care pediatric hospital, we retrospectively reviewed the surgical records utilizing the Current Procedural Terminology (CPT) code for volvulus from 2003 to 2014.
We reviewed medical records for diagnoses that may increase the risk of volvulus, including underlying neurological diseases (cerebral palsy, myelomeningocele, ventriculoperitoneal shunt, developmental delay, ability to ambulate), gastrointestinal diseases (constipation, known colonic dysfunction, gastrostomy and/or gastrojejunostomy tube, Malone antegrade continence enema [access site to facilitate colon washout]) and other gastrointestinal surgeries.
Clinical presentation was evaluated for abdominal pain, vomiting, constipation, abdominal distension, abdominal tenderness, fever >38C, and white blood cell count (WBC) >10,000cells/mL.
Surgical reports were reviewed to document the site of colonic volvulus (defined by visualized twisting of the cecum, sigmoid, ascending colon, transverse colon or descending colon) as well as the treatment (decompression by rectal tube, decompression by endoscopy, surgical derotation, resection of bowel, fixation of bowel to parietal peritoneum).
Imaging
All available abdominal imaging and reports at baseline and at presentation of colonic volvulus, including radiography, CT studies and fluoroscopic contrast enema studies, were reviewed by the authors.
The abdominal radiographs were reviewed in a randomized fashion using our PACS workstations (Synapse, Fuji, Valhalla, NY). Two pediatric radiologists (L.R.D. and M.L.C., with 8 and 1.5 years’ experience, respectively), blinded to type of colonic volvulus and to additional imaging studies, independently reviewed the radiographs. Study data were collected and managed using REDCap (Version 6.10.19, 2016; Vanderbilt University, Nashville, TN) electronic data capture tools [8].
Abdominal radiographic abnormalities were classified as intestinal (small bowel, colon, bowel uncertain) and extraluminal (pneumatosis, portal venous gas, free air, mass effect). Small bowel abnormalities were specified as right upper quadrant, right lower quadrant, left upper quadrant and left lower quadrant. Colon abnormalities were localized as cecum, ascending colon, transverse colon, descending colon, sigmoid colon or unclear location, and specifically evaluated for distension, coffee-bean sign, inverted U-shape, loss of haustra and pneumatosis. The presence or absence of rectal gas was also noted.
Abdominal CT scans and fluoroscopic contrast enema studies and reports, when available, were evaluated for the final diagnosis of colonic volvulus as described in the report.
Statistical analysis
Surgical and colonoscopic confirmation of colonic volvulus was used as the gold standard. Weighted kappa was calculated to assess interobserver agreement, defined as: fair, 0.21-0.40; moderate, 0.41-0.60; good, 0.61-0.80, and very good, 0.81-1.00. P-value <0.05 was considered statistically significant.
Results
Patient population
Our study group included 18 patients (7 females and 11 males) with a mean age of 14 years (range: 7 to 19 years). One patient had two episodes of volvulus, for a total of 19 cases.
Sixteen patients had significant neurological impairment. Ten patients had colonic dysmotility or chronic constipation. The most common neurological diseases included cerebral palsy (n=8), CHARGE (coloboma, heart defects, choanal atresia, retardation of growth/development, genital anomalies, ear anomalies) syndrome (n=4) and myelomeningocele (n=2) (Table 1). One patient with neurological impairment (CHARGE syndrome) had two episodes of colonic volvulus. Three patients had a Malone antegrade continence enema (surgical access site to facilitate colon washout). Two other patients developed colonic volvulus after abdominal surgeries: One patient had a recent history of partial colectomy and a second patient was a previously healthy child postoperative day 5 from appendectomy, which reportedly revealed a normal-appearing appendix, performed at an outside hospital.
Among the colonic volvulus patients, the most common clinical presentations were abdominal distension (n=14), abdominal pain (n=11) and emesis (n=9).
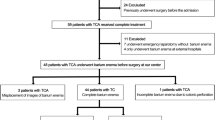
Cecal volvulus was most common (n=14), followed by sigmoid volvulus (n=4) and transverse colon volvulus (n=1) (Fig. 4). Seventeen of 19 (89.5%) cases of colonic volvulus were treated with surgery; 13/17 (76%) involved bowel resection and 2/19 (10.5%) cases with sigmoid volvulus were reduced by colonoscopy.
Imaging
All patients had supine abdominal radiographs. Sixteen of 19 (84%) had additional radiographs, left lateral decubitus radiograph (n=15) and/or upright radiograph (n=3). We excluded from analysis three reports; two outside reports (not available) and a report that was dictated after the enema study. Only 7/16 (44%) cases had the correct diagnosis of colonic volvulus in the radiology report. In 4/16 (25%) cases, the radiologist suggested colonic obstruction. Other diagnoses included ileus (n=4) and abdominal mass (n=1).
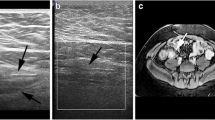
In our retrospective review of the abdominal radiographs, the coffee-bean sign specific to colonic volvulus was seen in only two cases (reader 2). Dilated loop of colon was seen in 18/19 (95%, reader 1) and 15/19 (79%, reader 2) cases (Figs. 1, 2, 3 and 4). Rectal gas was absent in 16/19 (84%, reader 1) and 12/19 (63%, reader 2) cases. Kappa value for dilated colonic loop was 0.38. Kappa value for absent rectal gas was 0.30.
A 17-year-old girl with cerebral palsy, constipation and increased abdominal distension. a Anteroposterior (AP) radiograph of the abdomen shows new focal right hemiabdominal distension (arrows) as compared to prior baseline AP abdominal radiograph (b) obtained 16 months earlier. Also, note the lack of rectal gas (star) in the presence of the focal right hemiabdominal distension (a). c AP view from a contrast enema demonstrates obstruction and beaking (arrow). Sigmoid volvulus was reduced in the operating room
A 13-year-old boy with Pierre-Robin syndrome and a history of tethered cord, chronic constipation, Malone antegrade continence enema (MACE) and increased distension. a Anteroposterior (AP) radiograph of the abdomen shows new focal left upper quadrant dilation (arrows) compared to prior baseline AP abdominal radiograph (b) obtained 17 months earlier. Rectal gas isn’t definitely appreciated in either study. (c) AP view from a contrast enema through MACE access site demonstrates volvulized cecum (arrows) in the left upper quadrant, which was confirmed at surgery
A 19-year-old boy with mosaic trisomy 9 and increased abdominal distension. a Anteroposterior (AP) radiograph of the abdomen shows new focal mid-abdominal dilated loop (arrows) and lack of rectal gas (star) compared to prior baseline AP abdominal radiograph (b) obtained 11 months earlier. c Coronal CT reformat image demonstrates swirling in the right hemiabdomen (arrow). d Coronal CT reformat image shows dilated air-filled cecum centrally (arrows). Cecal volvulus was reduced in the operating room
A 7-year-old previously healthy boy post-operative day 5 from appendectomy (pathology demonstrates normal appendix) with persistent pain and vomiting. a Anteroposterior (AP) radiograph of the abdomen shows dilated colon in the left hemiabdomen (arrows) with a lack of left lower quadrant bowel gas. Lateral (b) and AP (c) views from a contrast enema demonstrate an inability to reflux contrast past splenic flexure (arrows). Transverse colon volvulus was resected in the operating room
Fluoroscopic contrast enema study was performed in 9/19 (47%) cases, in which the diagnosis of colonic volvulus was suggested in 8/9 (89%) of the cases. Eight of 19 (42%) cases had CT studies; in 7/8 (88%), the diagnosis of colonic volvulus or closed loop obstruction was suggested.
Discussion
Colonic volvulus is rare in children and was described in case reports and small series [9]. Folaranmi et al. [9] in a 45-year (1965-2010) systemic review of the literature found 36 cases and reported on an additional 6 cases. They found that the most common underlying cause was neurodevelopmental delay in 29/42 (69%). There are no details on underlying neurological diseases [9]. In our series of 18 children, neurological disease was the most common (16/18 [89%]) predisposing condition for colonic volvulus. The most common neurological condition was cerebral palsy (8/16 [50%]). Constipation and colonic dysmotility are common (26-50%) in children with severe disabilities. Constipation and longer transit time are more common in non-ambulatory patients. Other factors include ketogenic diet often used to treat refractory epilepsy; use of anticonvulsants, opioids and antispasmodic medications, and lower intake of fiber and water in disabled children [10]. Altaf et al. [5] described the association of colonic abnormal motility in 8/18 (44%) of the children who developed colonic volvulus. The authors did not provide any details on any underlying neurological condition [5].
The most common presentation of colonic volvulus in children in our series was abdominal pain and abdominal distention without specific clinical features. This concurs with other series [9]. Timely diagnosis of colonic volvulus is critical as complications such as bowel gangrene, sepsis and death may develop if diagnosis is delayed [11]. Our study centered on the abdominal radiography findings in children with colonic volvulus. Abdominal radiography (specifically supine and left lateral decubitus views) is typically the initial imaging study obtained in children who present with abdominal pain and/or abdominal distention. Suggestion of colonic volvulus based on the abdominal radiograph can lead to prompt management of these patients and performance of a diagnostic study, either fluoroscopic colonic enema or abdominal CT scan. In our series, the diagnosis of colonic volvulus was suggested in only 7/16 (44%) of the cases in the radiology report. In our retrospective review of the radiographs, the specific finding of the coffee-bean sign was observed in two patients by only one radiologist. Absence of rectal gas and a focal dilated colonic loop were the most common findings in children with colonic volvulus (average: 73.5% and 87%, respectively). These findings were also described in other series in colonic volvulus in children [9].
In our series, the cecum was most common with 14/19 (74%) affected. Other series in adults and children demonstrated that the sigmoid is most commonly involved [1, 2, 12]. The reason for this difference is not clear. Interestingly, 3/19 (16%) had prior Malone antegrade continence enema (surgical access site at cecum to facilitate colon washout), for which the significance is unclear. Literature review demonstrates a prior reported case of cecal volvulus following Malone antegrade continence enema in which 127 young patients were followed a mean of 26.9 months after surgery [13].
Anatomical features that may predispose to volvulus include a long redundant colon with a narrow mesenteric attachment. It is hypothesized that chronic fecal overloading from constipation and dysmotility causes elongation and dilatation of the colon predisposing patients to volvulus [7, 14]. Colonic volvulus progresses to bowel obstruction, which can lead to ischemia, necrosis and perforation [1]. In our series, 13/17 (76%) cases of colonic volvulus were complicated with bowel necrosis necessitating bowel resection.
Our study has several limitations related to the retrospective nature of the study. In addition, our study group included only 19 cases of colonic volvulus. Although this is the largest series on colonic volvulus in children, it remains a small series that limits the study for only descriptive statistics.
Fluoroscopic contrast enema study and/or abdominal CT study can provide definitive diagnosis of colonic volvulus. As we have demonstrated in our study, specific signs of colonic volvulus are uncommonly observed on radiographs in children. In the case of colonic volvulus, CT can provide visualization of the twisted, obstructed colonic loops with swirling of the mesentery. When there are other diagnostic considerations, including other types of bowel obstruction, CT scan of the abdomen may be the most appropriate option. When the radiographs show specific signs, a fluoroscopic enema may be the more appropriate imaging to demonstrate the colonic volvulus as it involves less cost and radiation [15].
Conclusion
Children with neurological impairment are at risk for colonic volvulus. They usually present with abdominal pain and distention and diagnosis is challenging and often delayed. Radiologists should be alert to the possibility of colonic volvulus when an abdominal radiograph demonstrates focal colonic distention and absent rectal gas. Directing further evaluation with CT scan or fluoroscopic enema will facilitate earlier diagnosis and better outcome.
References
Halabi WJ, Jafari MD, Kang CY et al (2014) Colonic volvulus in the United States: trends, outcomes, and predictors of mortality. Ann Surg 259:293–301
Mellor MF, Drake DG (1994) Colonic volvulus in children: value of barium enema for diagnosis and treatment in 14 children. AJR Am J Roentgenol 162:1157–1159
Brothers TE, Strodel WE, Eckhauser FE (1987) Endoscopy in colonic volvulus. Ann Surg 206:1–4
Hiltunen KM, Syrja H, Matikainen M (1992) Colonic volvulus. Diagnosis and results of treatment in 82 patients. Eur J Surg 158:607–611
Altaf MA, Werlin SL, Sato TT et al (2009) Colonic volvulus in children with intestinal motility disorders. J Pediatr Gastroenterol Nutr 49:59–62
Husain K, Fitzgerald P, Lau G (1994) Cecal volvulus in the Cornelia de Lange syndrome. J Pediatr Surg 29:1245–1247
De Betue CT, Boersma D, Oomen MW et al (2011) Volvulus as a complication of chronic intestinal pseudo-obstruction syndrome. Eur J Pediatr 170:1591–1595
Harris PA, Taylor R, Thielke R et al (2009) Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Folaranmi SE, Cho A, Tareen F et al (2012) Proximal large bowel volvulus in children: 6 new cases and review of the literature. J Pediatr Surg 47:1572–1575
Park ES, Park CI, Cho SR et al (2004) Colonic transit time and constipation in children with spastic cerebral palsy. Arch Phys Med Rehabil 85:453–456
Pahlman L, Enblad P, Rudberg C et al (1989) Volvulus of the colon. A review of 93 cases and current aspects of treatment. Acta Chir Scand 155:53–56
Samuel M, Boddy SA, Nicholls E et al (2000) Large bowel volvulus in childhood. Aust N Z J Surg 70:258–262
Herndon CD, Rink RC, Cain MP et al (2004) In situ Malone antegrade continence enema in 127 patients: a 6-year experience. J Urol 172:1689–1691
Asabe K, Ushijima H, Bepu R et al (2002) A case of transverse colon volvulus in a child and a review of the literature in Japan. J Pediatr Surg 37:1626–1628
Image Gently (2014) Image Gently and SPR. http://imagegently.org/. Accessed 9 May 2016
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Marine, M.B., Cooper, M.L., Delaney, L.R. et al. Diagnosis of pediatric colonic volvulus with abdominal radiography: how good are we?. Pediatr Radiol 47, 404–410 (2017). https://doi.org/10.1007/s00247-017-3781-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-3781-5