Abstract
Background
Gadoteric acid is a paramagnetic gadolinium macrocyclic contrast agent approved for use in MRI of cerebral and spinal lesions and for body imaging.
Objective
To investigate the safety and efficacy of gadoteric acid in children by extensively reviewing clinical and post-marketing observational studies.
Materials and methods
Data were collected from 3,810 children (ages 3 days to 17 years) investigated in seven clinical trials of central nervous system (CNS) imaging (n = 141) and six post-marketing observational studies of CNS, musculoskeletal and whole-body MR imaging (n = 3,669). Of these, 3,569 children were 2–17 years of age and 241 were younger than 2 years. Gadoteric acid was generally administered at a dose of 0.1 mmol/kg. We evaluated image quality, lesion detection and border delineation, and the safety of gadoteric acid. We also reviewed post-marketing pharmacovigilance experience.
Results
Consistent with findings in adults, gadoteric acid was effective in children for improving image quality compared with T1-W unenhanced sequences, providing diagnostic improvement, and often influencing the therapeutic approach, resulting in treatment modifications. In studies assessing neurological tumors, gadoteric acid improved border delineation, internal morphology and contrast enhancement compared to unenhanced MR imaging. Gadoteric acid has a well-established safety profile. Among all studies, a total of 10 children experienced 20 adverse events, 7 of which were thought to be related to gadoteric acid. No serious adverse events were reported in any study. Post-marketing pharmacovigilance experience did not find any specific safety concern.
Conclusion
Gadoteric acid was associated with improved lesion detection and delineation and is an effective and well-tolerated contrast agent for use in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
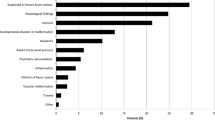
Magnetic resonance imaging (MRI) is being increasingly used in children as advances in technology address many of the inherent challenges of pediatric imaging, including the small size of anatomical structures, limited breath-holding capability and motion artifacts [1]. The benefits of paramagnetic contrast agents for improving the sensitivity and specificity of MR imaging in children have been recognized for some time [2–7], and there are numerous clinical indications for post-contrast MR imaging in children [8]. The examination of known or suspected central nervous system (CNS) tumors is a common indication for MRI in children, and MRI has become the primary imaging modality for both initial diagnosis and treatment follow-up of established tumors [9, 10]. The use of contrast material in evaluating pediatric CNS tumors leads to enhanced lesion delineation, additional characterization of internal lesion morphology, and improved differentiation of post-treatment changes from disease recurrence. Post-contrast MRI is also very useful in diagnosing the leptomeningeal spread of tumor, which otherwise would require repeated, invasive lumbar punctures. Another important clinical use for post-contrast MR imaging in young children is to assist in the diagnosis and assessment of complications from CNS infections. Similarly, because of its facilitation in visualizing abnormalities of bone and soft-tissue structures, MRI is becoming increasingly important in the evaluation of thoracic, abdominal, pelvic and musculoskeletal disorders in children [11].
The need to balance the clinical benefits of using contrast agents against the effects of drug administration during an otherwise noninvasive procedure is particularly relevant in children [5, 12]. As such, the use of gadolinium-based contrast agents (GBCAs) that are effective and well-tolerated is especially important in young children and adolescents [5, 13]. Ideally a contrast agent for use in children should have high stability given that children have a lifetime to express any potential delayed adverse event, a concern particularly relevant in children who undergo multiple examinations with exposure to large cumulative doses of contrast agents.
Gadoteric acid (gadoterate meglumine) (Dotarem®; Guerbet, Villepinte, France) is a paramagnetic gadolinium macrocyclic chelate. It has been marketed in Europe since 1989 and was approved by the U.S. Food and Drug Administration (FDA) in March 2013 for use in imaging of cerebral and spinal lesions and associated tissues with disrupted blood–brain barrier or abnormal vascularity in adults and children older than 2 years. Because of its unique chemical structure as a macrocyclic, ionic gadolinium complex, gadoteric acid has the highest thermodynamic and kinetic stability among the GBCAs [14]. Pre-clinical studies in rat models [15] demonstrated that there was neither a detectable release of dissociated gadolinium, nor skin or systemic lesions, and no long-term gadolinium retention [16]. Although people given GBCAs are known to be at risk for nephrogenic systemic fibrosis (NSF) [17], no single-agent reports of NSF have been reported or published for gadoteric acid (gadoterate meglumine full prescribing information available on FDA website http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/204781s000lbl.pdf. Accessed 5 May 2015). The safety and efficacy of gadoteric acid were first evaluated in adults [18–20], and based on favorable results a number of studies have since evaluated the safety and efficacy of gadoteric acid in children from neonates up to 17 years old. GBCAs are approved and commonly used in all age groups, including children younger than 2 years, throughout the world [21]. Gadoteric acid is approved for use in children without age restrictions in 70 countries. However, in the United States GBCAs are not approved by the FDA for use in children younger than 2 years, and this is also the case for gadoteric acid. This article summarizes the findings of the FDA submission data, which include data from the use of gadoteric acid in clinical trials in a pediatric population of 141 children and post-marketing observational studies in 3,669 children, along with an evaluation of the post-marketing pharmacovigilance experience.
Materials and methods
Trial designs and pediatric populations
This investigation was performed with the aid of the Guerbet company. Data from published and unpublished studies and from post-marketing pharmacovigilance studies were provided to the authors by Guerbet. These clinical studies and post-marketing observational studies are listed in Table 1.
We reviewed and summarized data from seven clinical trials, including four children aged 12–17 years who were inadvertently included in three adult studies (DGD-3-4, DGD-3-5, DGD-3-21), and six post-marketing observational studies evaluating the use of gadoteric acid in children (Table 1). These were open, non-randomized studies in children who required MRI of the central nervous system; the most recent was an international multicenter investigation. All studies were conducted in France and other countries in accordance with the Declaration of Helsinki and the regulations of the respective countries and institutions at the time the studies were conducted.
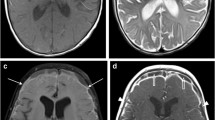
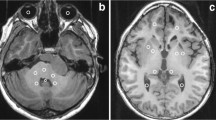
The DGD-3-15 study in 29 children, 3 of whom were younger than 2 years, and the DGD-3-16 study in 20 children, 2 of whom were younger than 2 years, were designed to determine the clinical safety and diagnostic efficacy of gadoteric acid in children undergoing CNS MR imaging who had already had unenhanced MR examinations. The DGD-3-15 study investigated the etiological diagnosis in 8 cases, lesion staging in 14 cases and tumor recurrence in 7 cases. The follow-up time was 2 h and 24 h after contrast administration. Similarly, the DGD-3-16 study, in which 13 boys and 7 girls received an average dose of 0.1 mmol/kg gadoteric acid, investigated the etiological diagnosis in 7 cases, tumor staging in 8 cases and tumor recurrence in 5 cases. Children were followed up for 20 min. The DGD-3-29 study assessed the safety and efficacy of gadoteric acid in 50 children, including two younger than 2 years of age, who required an MR examination for CNS tumors or for the diagnosis or surveillance of CNS diseases, and children were followed up for 45 min. The Sentio study (DGD-44-050) included 38 children who were undergoing MR imaging for the visualization of known or suspected CNS lesions in the pediatric arm. The radiologist assessed children immediately after the MR investigation and at 24 h post-injection during a follow-up visit. The study design allowed direct efficacy comparison of both MR imaging conditions (with and without gadoteric acid injection) in adults and children, and internal validation of gadoteric acid as an effective MR contrast agent in adults by comparing it with gadopentetic acid (Magnevist®; Bayer Schering Pharma, Berlin, Germany).
Post-marketing observational studies were conducted based on routine contrast-enhanced MRI using gadoteric acid. The first study was published by Neiss et al. [22] and involved a pediatric population of 305 children, 6 of whom were younger than 2 years. The second study was conducted by Briand et al. [23] and investigated the safety and efficacy of gadoteric acid in 402 children, 26 of whom were younger than 2 years. CNS evaluations accounted for the majority of the MRI procedures. These open, non-drug comparative trials followed a similar protocol. Children (0–17 years old) who had undergone MRI without contrast medium were eligible after obtaining written consent from both parents to participate.
Maurer et al. [19] conducted a large study (n = 84,621) in Germany that included 1,760 children (ages 5 weeks to 17 years) with CNS, whole-body and musculoskeletal MRI and MR angiography. Each child was monitored for adverse reactions during the MR examination and for 30–60 min after the MR examination. The study described by Pathkar [26] was an interim analysis (n = 24,961) of the SECURE trial conducted in France, Germany, India, Saudi Arabia, China, Austria, Spain and the United Kingdom as of April 1, 2012. This international study investigated the safety profile of 0.1 mmol/kg gadoteric acid and included 1,057 children ages 0–17 with CNS or other conditions. This pediatric population included 86 children younger than 2 years [24]. In children with renal insufficiency, a follow-up of at least 3 months was established to record any signs of nephrogenic systemic fibrosis (NSF).
Emond and Brunelle [25] conducted a single-center, open-label study in France that included 104 children younger than 18 months; children were followed up on site for 2 h post-injection. Finally, the Ishiguchi and Takahashi [20] study was conducted in Japan and included 41 children, 2 of whom were younger than 2 years. Children undergoing MR imaging of the brain/spinal cord or trunk/limbs were followed up for at least 2 h on-site. After gadoteric acid administration, 13 baseline characteristics were used to investigate factors that might predict a greater likelihood of acute non-renal adverse reactions [20].
In addition, cumulative post-marketing pharmacovigilance data for gadoteric acid were compiled in the Guerbet safety database using Register software version 5.3 (ArisGlobal, Stamford, CT) and were reviewed. Safety data were received by the Guerbet Pharmacovigilance Department from worldwide sources, beginning with the initial European Marketing Authorization in France on March 8, 1989, and continuing through March 31, 2012. More than 30 million patients, including more than 51,000 children younger than 2 years, are estimated to have been exposed to gadoteric acid (Guerbet source data).
Contrast agent administration and MR imaging
Gadoteric acid contrast medium was injected through an intravenous cannula to achieve a mean dose of approximately 0.1 mmol/kg of a 0.5 mol/L solution, i.e. 0.2 ml/kg, at an injection rate of 1–3 ml/min for slow infusion or 1–2 ml/s for rapid bolus injection. MR scanners, most often 1.5-T field-strength, were used in all studies to obtain T1-W and T2-W spin-echo or gradient-echo sequences before the administration of gadoteric acid. T1-W spin-echo sequences were then repeated in the same section planes as pre-contrast sequences.
Efficacy assessments in children during clinical trials
The open, non-drug comparative trials DGD-3-15, DGD-3-16 and DGD-3-29 implemented similar protocols to evaluate CNS MRIs; these evaluations were based on image quality, diagnostic performance, and effects on treatment approach. The quality of images obtained post-contrast versus pre-contrast was assessed overall and with respect to improvements in localization or delineation of various anatomical structures. Diagnostic improvement was evaluated by comparing MR images obtained before and after gadoteric acid administration, and it was noted whether gadoteric acid led to modifications in treatment or management. The Sentio study was designed to demonstrate the superiority of gadoteric acid-enhanced vs. unenhanced MR imaging in terms of CNS lesion visualization (border delineation, visualization of internal morphology, and degree of contrast enhancement) in “pre” (unenhanced) vs. “paired” (unenhanced + enhanced) images for each patient. Three off-site, blinded readers independently reviewed all images from pre and paired MR imaging modalities and rated each lesion up to a limit of the five largest representative lesions identified using a 3-point scale (0 = not evaluable, 1 = seen but imperfectly, 2 = seen completely/perfectly). Mean image quality and diagnostic confidence were also assessed. Image quality was evaluated for each lesion according to a 3-point scale (1 = poor, 2 = fair, 3 = good), and an overall score per patient was calculated. Diagnostic confidence when evaluating MRI modalities was graded using a 5-point scale (1 = nil, 2 = poor, 3 = moderate, 4 = high, 5 = excellent).
Efficacy assessments in children during post-marketing observational studies
The study conducted by Briand et al. [23] was a continuation of the study by Neiss et al. [22]. Prior to gadoteric acid injection, a score on a 3-point scale (1 = worse, 2 = identical, 3 = better) was assigned to evaluate the T2-W vs. T1-W MR images. After injection, the T1-W MR imaging was compared in the same way (scored on a 3-point scale) with the pre-injection T1-W and T2-W MR images. The post-injection diagnosis was rated as worse, identical to, better than, or complementary to the pre-injection diagnosis. The radiologist was also asked to indicate whether the use of gadoteric acid resulted in a change in treatment strategy and the reasons for any such change. The post-gadoteric acid MR imaging was compared with pre-injection T1-W and T2-W MR images with respect to lesion/edema limit, lesion/central necrosis limit, lesion/healthy tissue limit, edema/surrounding tissue limit, evaluation of vascularization, and detection of other lesions inside or outside or on the border of the organ examined.
In the Maurer et al. study [19], which included 1,760 children, radiologists from 129 German centers completed standardized questionnaires for their patients who were undergoing MR imaging exams with the administration of gadoteric acid from January 2004 through January 2010. These questionnaires included patient data, any risk factor for contrast administration such as renal impairment, type and indication of MR imaging examination being performed (neurological, body or musculoskeletal), amount and mode of contrast injection, and any premedication given. Image quality was assessed as excellent, good, moderate, poor or very poor (no noticeable signal enhancement). Finally, the radiologist identified the number and type of adverse events and any possible association with contrast medium administration.
In the Emond and Brunelle study [25], image quality was assessed with a 5-point scale (excellent, good, average, poor, nil) and diagnostic contribution with a 5-point scale (definitely normal, probably normal, indecisive, probably abnormal, definitely abnormal); consequences for therapeutic decisions were defined according to four items (choice of initial treatment, continuation of treatment, change of treatment, no treatment). The SECURE [24] and Ishiguchi and Takahashi [20] studies also evaluated whether images were of diagnostic quality for CNS indications. The SECURE study was a safety evaluation, although efficacy was assessed as a secondary endpoint as image quality [24]. In the Ishiguchi and Takahashi study [20], the efficacy of gadoteric acid as an image-enhancing agent was assessed by the physician’s appraisal according to the following grades: 1 = very effective, i.e. diagnostic performance highly improved; 2 = effective, i.e. diagnostic performance improved, and 3 = ineffective.
Safety assessments in children during clinical trials and post-marketing observational studies
The study investigator monitored adverse events, including injection-associated discomfort. The investigator recorded the type of event, outcome and whether it was related to gadoteric acid. Follow-up usually ranged from 20 min to 2 h post-gadoteric acid injection, based on local clinical practices, but was as long as 3 months in patients with renal failure in the SECURE study [24]. The severity and duration of adverse events were also reported in some studies. In the DGD-3-15 study, safety was also assessed using a battery of laboratory safety tests, including liver and renal function tests, routine hematology and urinalysis. In the Sentio study electrocardiograms (ECGs) were recorded in addition to standard safety assessments, e.g., injection site reactions, laboratory tests and vital signs. In this study, standard blood tests were obtained at baseline and after 24 h, and ECGs were recorded in a subset of 12 children exposed to gadoteric acid at baseline.
To complete the safety assessment, the post-marketing pharmacovigilance experience — based on more than 30 million doses given (as of March 31, 2012) and including >51,000 children younger than 2 years — was reviewed by Guerbet from the company safety database. A total of 1,791 spontaneous case reports involving 3,947 adverse drug reactions were recorded in either adults or children who were exposed to all dosages of gadoteric acid from the launch in 1989 to the cut-off date of March 31, 2012. Adverse drug reactions were coded in the safety database according to the MedDRA dictionary (version 15.0; MedDRA MSSO, Mclean, VA). Analysis was performed on both qualitative and quantitative assessment. We only considered case reports in the pediatric population for this review.
Statistical analysis
Descriptive statistics were used for each study.
Results
Data were collected from 3,810 pediatric patients (ages 3 days to 17 years) exposed to gadoteric acid in 7 clinical trials of CNS imaging (n = 141) and six post-marketing observational studies of CNS, musculoskeletal and whole-body imaging (n = 3,669) (Table 1). Of these, 3,569 children were 2–17 years of age and 241 were younger than 2 years. Data from all patients were assessed for safety and efficacy (although efficacy results from the SECURE study were not available at the time of the interim analysis).
Efficacy in children during clinical trials
The diagnostic efficacy of gadoteric acid was investigated in 7 clinical studies involving 141 children (DGD-3-4, DGD-3-5, DGD-3-21, Sentio, DGD-3-15, DGD-3-16 and DGD-3-29). The Sentio study and three open-label, single group, non-randomized trials (DGD-3-15, DGD-3-16 and DGD-3-29) were conducted for CNS indications, and children exposed to gadoteric acid were present in all age ranges (7 younger than 24 months, 33 ages 2–6 years, 58 ages 6–12 years and 43 ages 12–17 years). Globally, in these clinical studies efficacy results were consistent with those obtained in the adult population. Gadoteric-acid-enhanced MR imaging produced significant improvement in the detection and visualization of CNS lesions, with more accurate delineation of the lesion/normal tissue or lesion/edema borders. Gadoteric-acid-enhanced MR imaging provided a good diagnostic contribution and allowed better patient management.
In the Sentio study mean image quality and diagnostic confidence were higher with paired (unenhanced and enhanced) images vs. pre (unenhanced) imaging scores (mean image quality score ranges were 2.91–3.0 vs. 1.55–2.32, respectively, and mean diagnostic confidence score ranges were 3.94–4.74 vs. 2.71–3.24, respectively). Because a relatively small number of children were included in the study according to the study design, only descriptive analysis of efficacy in this population was presented and no statistical tests were performed. Gadoteric acid was found to improve the visualization of CNS lesions over unenhanced MR imaging alone, with the paired images being superior to the pre images for all three co-primary endpoints (border delineation, internal morphology, contrast enhancement) reported by all three off-site readers. The mean lesion visualization endpoint across three variables (lesion border delineation, internal morphology and contrast enhancement) for paired images ranged from 1.36 to 3.51, whereas it ranged from 0 to 1.42 for pre images. Descriptive statistics for the efficacy evaluation in the Sentio study were of an order of magnitude similar to those reported in the adult population.
In the DGD-3-15 and DGD-3-16 studies, the image quality of gadoteric acid-enhanced T1-W MR imaging sequences was considered better than that of unenhanced T1-W sequences in 69% and 84% of cases, respectively, and better than unenhanced T2-W sequences in 62% and 24% of cases, respectively. More specifically, the diagnostic contribution was considered better than or complementary to pre-contrast diagnostic performance in 94% of cases in the DGD-3-16 study and resulted in a change in treatment in 15% of cases. The DGD-3-15 and DGD-3-16 studies also assessed specific criteria where gadoteric acid provided improved image quality; gadoteric acid was associated with improvement in lesion/edema delineation in 16% and 21% of cases, respectively, lesion/normal tissue delineation in 26% and 55% of cases, respectively, visualization of blood supply in 42% and 41% of cases, respectively, and visualization of other lesions in 11% and 14% of cases, respectively.
In the DGD-3-29 study, gadoteric acid markedly improved the diagnostic quality of MR imaging examinations, providing more accurate diagnosis in 40 of 50 patients (80%) and modifying the diagnosis in eight patients (16%). Gadoteric acid enhancement improved tumor visualization and facilitated localization of lesions. Post-contrast sequences were considered to be of good (8%) or excellent (92%) image quality in all patients, which was significantly better than pre-contrast sequences (50% and 48%, respectively). Post-contrast images influenced the therapeutic approach in 96% of patients (48/50), including modification of initial treatment in 5 patients (10%), change in choice of initial treatment in 6 patients (12%), a decision not to initiate treatment in 23 patients (46%) and a decision to continue of treatment in 15 patients (30%).
Efficacy in children found in post-marketing observational studies
Because of the variability of efficacy endpoints, efficacy results cannot be pooled for the total population (n = 3,669) enrolled in these studies [19, 20, 22–25].
Of these, two open post-marketing observational studies were conducted in France involving 402 children [22, 23]. Among this pediatric population, 81% was 15 years or younger and 6.5% was 2 years or younger. CNS investigations accounted for 82.4% of MR imaging exams and bone and soft-tissue imaging for 11.4%. Mean gadoteric acid injected dose was 0.22 ml/kg (range 0.10–0.80 ml/kg). Overall, diagnostic evaluation was considered to be improved post contrast administration in 85% of neuroradiologic exams and 95% of musculoskeletal investigations. Improved diagnostic performance resulted in treatment modifications in 15–34% of patients.
In the Maurer study [19] efficacy assessments were simple but demonstrated that approximately half of the images were rated either excellent (49%) or good (47%), and almost all (99.7%) were of diagnostic grade in the total population, including the 1,760 children. At-risk patients also had slightly, but significantly, poorer image quality: good or excellent image quality was achieved in 95.7% of at-risk patients vs. 97.5% of patients without known risk factors. The proportion was 93.2% in patients with renal failure and 94.2% in patients with liver dysfunction.
In the Emond and Brunelle study [25], image quality was rated “excellent/good” for gadoteric-acid-enhanced MR imaging in 102 (98.0%) children. The diagnostic contribution was assessed as optimal (definitely abnormal/normal diagnosis) in 101 children (97.1%). The examination with gadoteric-acid-enhanced MR imaging confirmed the choice of initial treatment in 50 children (48.1%).
The Ishiguchi and Takahashi study [20] showed that in a large majority of cases (99.5%) the efficacy of gadoteric acid was rated “effective” or “very effective.” An analysis of the factors that affected efficacy revealed that the presence of kidney disorders was associated with a greater likelihood of inefficacy (2.1% vs. 0.4% for patients without kidney disorders); however, no further information was provided by the authors as to the reason for inefficacy associated with kidney disorders. Other patient characteristics, including gender, age, weight, indications, liver disorder and gadoteric acid dose, were not associated with any significant differences in efficacy.
Safety in children during clinical trials and post-marketing observational studies
The safety of gadoteric acid was assessed in 3,810 children (Table 2). In the 141 children from clinical trials, who were exposed to gadoteric acid, 7 were ages 1–24 months, 33 were ages 2–6 years, 58 were ages 6–12 years and 43 were ages 12–17 years. Gadoteric acid was well-tolerated overall. There were no treatment-related serious adverse events and no treatment-related adverse events that required treatment withdrawal. As shown in Table 3, treatment-related adverse events included headache, dizziness, hematuria, pruritus, vomiting, asthenia, injection site urticaria and nausea.
No related adverse events occurred in children in the youngest age group (1–24 months). In 2- to 6-year-olds pruritus was the only related adverse event reported, in one child. Headache in two children and dizziness, hematuria and vomiting (each in one patient) were the only related adverse events reported in the 6- to 12-year-olds. Asthenia, injection site urticaria and nausea were the only related adverse events reported in 12- to 17-year-olds. A single adverse event was observed in the DGD-3-16 study, which was a brief episode of vomiting in one child who was also receiving sodium oxybate. This adverse event could be a result of gadoteric acid, sodium oxybate or the combination of both. In addition, no adverse events were reported with previous gadoteric acid injections in the 50 children from the DGD-3-29 study, including one child who had received four previous gadoteric acid administrations. In the DGD-3-15 study, in which safety was assessed using routine laboratory tests, no clinically significant changes were related to gadoteric acid administration, which was found to be safe in both laboratory and clinical terms.
The Sentio study showed evidence of occasional mild to moderate adverse events in 10 (26.3%) of 38 children exposed to gadoteric acid. Of these, treatment-emergent adverse events were reported in eight patients, six (15.8%) of whom exhibited adverse events considered treatment-related: dizziness in one child, vomiting and injection site urticaria in one child, nausea and urticaria in one child, injection site pruritus in one child and headache in two children. No related serious adverse events were recorded, and all children recovered without any specific treatment. Similar adverse event profiles were seen in the pediatric and adult populations. Data are descriptive-only and no statistical comparisons were performed in these children. However, no clinically relevant changes were detected with respect to laboratory tests, vital signs or ECG recordings. A small increase in mean QTc (using both Fridericia and Bazett QT correction formulas) was observed with gadoteric acid in adults and children when comparing baseline ECGs to recordings at 30 min post injection (the mean change in QTc Fridericia from baseline to 30 min post injection was 7.25 ms). In the adults who were exposed to the comparable contrast agent gadopentetic acid, an equivalent increase in mean QTc was observed (mean change in QTc Fridericia from baseline to 30 min post injection was 10.32 ms).
Post-marketing observational studies in 3,669 children revealed that gadoteric acid also had an excellent safety profile in clinical use. In the Briand et al. study [23], a single mild and transient adverse event was reported: a 16-year-old girl developed a papule at the injection site, which resolved without treatment. In the Maurer et al. [19] study, involving a population of 1,760 children, 9 children (0.4%) experienced adverse events (mainly nausea). No serious adverse events were observed. Ten children from the Maurer study [19] were younger than 2 years and none developed adverse events. The same was true in the SECURE [24], Emond and Brunelle [25] and Ishiguchi and Takahashi [20] studies, in which no children developed adverse events.
The post-marketing pharmacovigilance experience is based on more than 30 million doses given (as of March 31, 2012), including doses to >51,000 children younger than 2 years (Guerbet source data). In the Guerbet safety database, a total of 1,791 case reports involving 3,947 adverse drug reactions were recorded in either adults or children exposed to all dosages of gadoteric acid. Spontaneous reports of adverse reactions from the launch in 1989 to March 2012 are consistent with the adverse drug reactions observed in clinical trials and the known safety profile of gadoteric acid. Guerbet analyzed the pharmacovigilance data obtained through March 31, 2012, and found eight case reports in children younger than 2 years (one girl, seven boys) that correspond to 10 adverse drug reactions. Two cases were serious (including one case of tremors in a baby breastfeeding with a mother previously exposed to gadoteric acid and one case of a decrease in heart rate in an infant who underwent concomitant administration of gadoteric acid and sedation medications) and six were non-serious. Adverse events observed in these children younger than 2 years were most frequently a result of medication errors, such as overdose or extravasation, with no associated adverse outcome. All cases for which the outcome was available are reported as having recovered. There were no fatal outcomes. As of March 31, 2012, there were 88 case reports in children (46 girls, 41 boys, 1 unknown) ages 2–16 years that correspond to 197 adverse drug reactions, i.e. 5% of the total number of cases cumulatively. Thirty-five of these cases were serious and 53 were non-serious. In most cases, patients recovered. Among the serious cases, there was one fatal outcome (a 3.5-year-old girl who died of the underlying disease, a posterior fossa tumor with meningeal metastasis). Most cases in this pediatric population of 2- to 16-year-olds were associated with hypersensitivity reactions (anaphylaxis; vascular reactions including swelling of the dermis, subcutaneous tissue, mucosa and submucosal tissues; urticaria/hives, and skin rash). This analysis of post-marketing pharmacovigilance data concluded that the reactions observed in all pediatric age groups were similar to those reported in the general population of patients in terms of nature, intensity and outcome [19].
Discussion
Considerable advances have been made in pediatric body, CNS, cardiac and musculoskeletal MR imaging that enable high-quality imaging of even the smallest children and expand the range of indications amenable to MRI [1, 13]. Major advances have also occurred in the investigation of children with suspected brain tumors, with MRI becoming the primary imaging modality. MRI is recognized as the procedure of choice in pediatric neuroimaging because it provides high sensitivity for the detection and characterization of disease, avoids childhood exposure to ionizing radiation (repeated CT scans can result in in excess risk for cancer in childhood and early adolescence [10, 27]) and requires smaller volumes of contrast agent compared with the typical volumes of iodinated contrast agent used with CT [27, 28]. However, even considering the small volume of MR contrast agent required for an imaging procedure, the clinical benefits must be balanced against the potential risks of administering a drug, particularly in the pediatric population.
In the CNS studies presented here, gadoteric acid enhancement markedly improved the diagnostic quality of the MR examination and frequently influenced the therapeutic approach. Furthermore, gadoteric acid was associated with improvements in delineation between lesion and edema or normal tissue, and improved visualization of the blood supply compared to unenhanced sequences. In summary, the results from CNS indications demonstrate that gadoteric acid is clinically effective, providing images of good or excellent quality that improve diagnostic information, help guide treatment, and detect recurrence. Gadoteric acid also had an excellent safety profile, and no clinically significant abnormalities in the safety laboratory tests were considered to be related to gadoteric acid. These findings are consistent with studies of other contrast agents in children, many of whom had CNS presentations [5–7, 10, 29]. A limitation of the present review is that it used only descriptive statistics for each study. A meta-analysis was not possible because the studies had different objectives (efficacy and safety) and different assessment criteria. On the other hand, the scope of this review is broader than that of the clinical trials alone, because post-marketing observational studies and pharmacovigilance experience were analyzed together.
In addition to the studies including the musculoskeletal imaging already mentioned [3, 11], gadoteric acid enhancement was found to be useful in four published studies of pediatric musculoskeletal imaging [2, 4, 30, 31]. Contrast enhancement with gadoteric acid has been shown to provide a reliable method for the early detection and monitoring of juvenile rheumatoid arthritis [2], considerably improving patient management. Gadoteric acid enhancement also proved useful in the evaluation of Legg–Calvé–Perthes disease, which can be difficult to diagnose and stage radiographically [4, 30, 31]. Gadoteric acid permitted accurate staging of Legg–Calvé–Perthes disease, which may help in the determination of the optimal time for surgery. Another study evaluated the role of gadoteric acid in the management of painful osseous crises, which occur frequently in children with sickle cell anemia [3]. Although gadoteric acid-enhanced imaging could not differentiate between acute infarcts or acute osteomyelitis as causes of the crises, enhanced imaging helped to determine the anatomical site and extent of acute infarcts or acute osteomyelitis, and contributed to the planning of orthopedic treatment. Whenever feasible, contrast enhancement is recommended in the evaluation of suspected infectious or neoplastic conditions that affect the pediatric CNS, visceral organs and musculoskeletal systems.
Similarly, cardiac MR imaging has been found to be appropriate for the assessment of complex congenital heart disease, including anomalies of the coronary circulation, great vessels, cardiac chambers and valves. Cardiac MR imaging is particularly useful in this regard in children in whom exposure to ionizing radiation is to be avoided [32].
Results from the post-marketing observational studies confirm the safety and efficacy of gadoteric acid in clinical practice. Efficacy results showed a high level of diagnostic improvement obtained with gadoteric acid versus unenhanced imaging, with 95–100% of scans rated good or excellent for image quality. Few adverse events were recorded among the large cohort of children in the post-marketing observational studies, which included children with an allergic history, those requiring an anesthetic and those receiving concomitant treatment.
Adverse events observed in children younger than 2 years were most frequently a result of medication errors, such as overdose or extravasation (without associated adverse outcome), and the majority of cases in the 2- to 16-year-old population were associated with hypersensitivity reactions. Experience in children did not find any specific safety concern. Post-marketing pharmacovigilance experience of more than 20 years of clinical radiology practice was consistent with the known safety profile of gadoteric acid, as obtained during clinical trials.
Gadolinium use has been associated with the development of a serious, potentially fatal, adverse reaction, i.e. nephrogenic systemic fibrosis (NSF), in patients with impaired renal function [17]. According to European and American guidelines, patients most at risk for NSF are those with chronic kidney disease stages 4 or 5. Patients with chronic kidney disease stage 3 and children younger than 1 year are considered at moderately increased risk [33]. The European guidelines classify GBCAs into three categories regarding NSF risk: high risk, medium risk and low risk. All macrocyclic GBCAs, including gadoteric acid, are classified as low risk. The European guidelines also recommend that high-risk GBCAs be avoided in neonates and the minimum dose of GBCA is to be used in infants up to 1 year of age, as well as in patients with chronic kidney disease stage 3. In the United States, no GBCA is approved for use in children younger than 2 years. An update on NSF and its guidelines has been published [34]. Although there is no evidence that children are at greater risk for NSF than adults, there are reports of NSF in children with severe renal failure [35], and one recent report identified 23 non-redundant pediatric cases of NSF, most with chronic kidney disease; however none of these cases received gadoteric acid [36].
At the time of this report no non-confounded case of NSF had been reported with gadoteric acid in adults or children (gadoterate meglumine full prescribing information on FDA website http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/204781s000lbl.pdf. Accessed 5 May 2015). In 2011, among 17 NSF cases 1 adult case was attributed to gadoteric acid, but that patient received another GBCA, as noted in a table in that article, thus ruling out the possibility of a non-confounded case [37]. Subsequently the same author published an update of the Danish NSF cases, and there was no mention of gadoteric acid when patients were exposed to only one GBCA [38]. Furthermore, although the follow-up was limited to 3 months and in a population not at risk, no case of NSF has been reported in the ongoing SECURE study [24]. A new study, NSsaFe, has begun to evaluate the long-term safety of gadoteric acid in an at-risk population with renal insufficiency, with a longer follow-up period of up to 2 years (Available via https://clinicaltrials.gov/ct2/show/NCT01467271?term=NCT01467271&rank=1. Accessed 5 May 2015).
Conclusion
The experience gained from clinical trials and post-marketing observational studies in 3,810 children, including infants, children and adolescents, indicates that gadoteric acid has both clinical efficacy and a well-established safety profile in MR imaging examinations of the CNS and other body parts. The use of gadoteric acid resulted in contrast enhancement of regions of interest, improved image quality, provided additional diagnostic information compared with non-enhanced sequences and often led to changes in patient management. In addition, based on clinical trials, post-marketing observational studies and pharmacovigilance analysis, experience in children did not find any safety concern, thus confirming the excellent safety profile of gadoteric acid.
References
MacKenzie JD, Vasanawala SS (2010) State-of-the-art in pediatric body and musculoskeletal magnetic resonance imaging. Semin Ultrasound CT MR 31:86–99
Hervé-Somma CM, Sebag GH, Prieur AM et al (1992) Juvenile rheumatoid arthritis of the knee: MR evaluation with Gd-DOTA. Radiology 182:93–98
Bonnerot V, Sebag G, de Montalembert M et al (1994) Gadolinium-DOTA enhanced MRI of painful osseous crises in children with sickle cell anemia. Pediatr Radiol 24:92–95
Ducou le Pointe H, Haddad S, Silberman B et al (1994) Legg–Perthes–Calve disease: staging by MRI using gadolinium. Pediatr Radiol 24:88–91
Hanquinet S, Christophe C, Greef DD et al (1996) Clinical evaluation of gadodiamide injection in paediatric MR imaging. Pediatr Radiol 26:806–810
Lundby B, Gordon P, Hugo F (1996) MRI in children given gadodiamide injection: safety and efficacy in CNS and body indications. Eur J Radiol 23:190–196
Lowe LH, Kearns GL, Wible JH Jr (2006) The safety and efficacy of neuroimaging with gadoversetamide injection in pediatric patients. Curr Med Res Opin 22:2515–2524
Barkovich A, Raybaud C (2011) Pediatric neuroimaging, 5th edn. Lippincott Williams & Wilkins, Philadelphia
Rao P (2008) Role of MRI in paediatric neurooncology. Eur J Radiol 68:259–270
Colosimo C, Demaerel P, Tortori-Donati P et al (2005) Comparison of gadobenate dimeglumine (Gd-BOPTA) with gadopentetate dimeglumine (Gd-DTPA) for enhanced MR imaging of brain and spine tumors in children. Pediatr Radiol 35:501–510
Balassy C, Hörmann M (2008) Role of MRI in paediatric musculoskeletal conditions. Eur J Radiol 68:245–258
Riccabona M (2008) MRI in neonates, infants and children — overuse or still insufficient availability for paediatric needs? Eur J Radiol 68:189–190
Dagia C, Ditchfield M (2008) 3T MRI in paediatrics: challenges and clinical applications. Eur J Radiol 68:309–319
Port M, Idée JM, Medina C et al (2008) Efficiency thermodynamics and kinetic stability of marketed gadolinium chelates and their possible clinical consequences: a critical review. Biometals 21:469–490
Fretellier N, Idée JM, Bruneval P et al (2012) Hyperphosphataemia sensitizes renally impaired rats to the profibrotic effects of gadodiamide. Brit J Pharmacol 165:1151–1162
Haylor J, Schroeder J, Wagner B et al (2012) Skin gadolinium following use of MR contrast agents in a rat model of nephrogenic systemic fibrosis. Radiology 263:107–116
Grobner T (2006) Gadolinium — a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol Dial Transplant 21:1104–1108
Kang JW, Lim TH, Choi CG et al (2010) Evaluation of contrast-enhanced magnetic resonance angiography (MRA) using Gd-DOTA compared with time-of-flight MRA in the diagnosis of clinically significant non-coronary arterial disease. Eur Radiol 20:1934–1944
Maurer M, Heine O, Wolf M et al (2012) Tolerability and diagnostic value of gadoteric acid in the general population and in patients with risk factors: results in more than 84,000 patients. Eur J Radiol 81:885–890
Ishiguchi T, Takahashi S (2010) Safety of gadoterate meglumine (Gd-DOTA) as a contrast agent for magnetic resonance imaging: results of a post-marketing surveillance study in Japan. Drugs R D 10:133–145
Meng H, Grosse-Wortmann L (2012) Gadolinium in pediatric cardiovascular magnetic resonance: what we know and how we practice. J Cardiovasc Magn Reson 14:56
Neiss AC, Le Mignon MM, Vitry A et al (1991) Efficacy and safety of DOTA-Gd from a European multicenter survey. Preliminary results on 4,169 cases. Rev Im Med 3:383–387
Briand Y, Neiss AC, Vitry A et al (1992) Efficacy and safety of the macrocyclic complex Gd-DOTA in children: results of a multi-centre study. Proceedings of the 29th Congress of the European Society of Pediatric Radiology, 128
Pracros JP, de la Garanderie J (2012) The SECURE study: observational post-marketing study on the safety of meglumine gadoterate — interim analysis of 972 children. Pediatr Radiol 42:S511–S512
Emond S, Brunelle F (2011) Gd-DOTA administration at MRI in children younger than 18 months of age: immediate adverse reactions. Pediatr Radiol 41:1401–1406
Pathkar D (2012) SECURE study (abstract): observational post-marketing study on the safety of meglumine gadoterate (Gd-DOTA) — interim analysis on 21,447 patients. J Med Imaging Radiat Oncol 56:134
Pearce MS, Salotti JA, Little MP et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380:499–505
Ylänen K, Poutanen T, Savikurki-Heikkilä P et al (2013) Cardiac magnetic resonance imaging in the evaluation of the late effects of anthracyclines among long-term survivors of childhood cancer. J Am Coll Cardiol 61:1539–1547
Martí-Bonmatí L, Vega T, Benito C et al (2000) Safety and efficacy of Omniscan (gadodiamide injection) at 0.1 mmol/kg for MRI in infants younger than 6 months of age: phase III open multicenter study. Invest Radiol 35:141–147
Sebag G, Ducou Le Pointe H, Klein I et al (1997) Dynamic gadolinium-enhanced subtraction MR imaging — a simple technique for the early diagnosis of Legg–Calvé–Perthes disease: preliminary results. Pediatr Radiol 27:216–220
Dillman JR, Hernandez RJ (2009) MRI of Legg–Calve–Perthes disease. AJR Am J Roentgenol 193:1394–1407
Hundley WG, Bluemke DA, Finn JP et al (2010) ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance. A report of the American College of Cardiology foundation task force on expert consensus documents. Circulation 121:2462–2508
Reiter T, Ritter O, Prince MR et al (2012) Minimizing risk of nephrogenic systemic fibrosis in cardiovascular magnetic resonance. J Cardiovasc Magn Reson 14:31
Weller A, Barber JL, Olsen OE (2014) Gadolinium and nephrogenic systemic fibrosis: an update. Pediatr Nephrol 29:1927–1937
Mendichovszky IA, Marks SD, Simcock CM et al (2008) Gadolinium and nephrogenic systemic fibrosis: time to tighten practice. Pediatr Radiol 38:489–496
Nardone B, Saddleton E, Laumann AE et al (2014) Pediatric nephrogenic systemic fibrosis is rarely reported: a RADAR report. Pediatr Radiol 44:173–180
Elmholdt TR, Pedersen M, Jorgensen B et al (2011) Nephrogenic systemic fibrosis is found only among gadolinium-exposed patients with renal insufficiency: a case–control study from Denmark. Br J Dermatol 165:828–836
Elmholdt TR, Olesen ABB, Jorgensen B et al (2013) Nephrogenic systemic fibrosis in Denmark — a nationwide investigation. PLoSOne 8, e82037
Acknowledgments
The authors wish to thank all the participating sites from these clinical trials and post-marketing observational studies supported by the Guerbet Group.
Conflicts of interest
Drs. Balassy, Roberts and Miller were provided data from published and unpublished studies and post-marketing pharmacovigilance studies by Guerbet. Dr. Roberts has served as a paid consultant for Guerbet but did not receive any support related to this specific paper. Dr. Balassy has received honoraria from Guerbet for speaking engagements but did not receive any support related to this specific paper. Dr. Miller has not received financial support from Guerbet.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balassy, C., Roberts, D. & Miller, S.F. Safety and efficacy of gadoteric acid in pediatric magnetic resonance imaging: overview of clinical trials and post-marketing studies. Pediatr Radiol 45, 1831–1841 (2015). https://doi.org/10.1007/s00247-015-3394-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3394-9