Abstract
Mean dP/dtic is a quantitative measurement of ventricular function that can be obtained noninvasively by echocardiography. In adults with mitral regurgitation (MR), it has been shown to be a more sensitive predictor of postoperative left ventricular ejection fraction (EF). The utility of dP/dtic in pediatric congenital heart diseases with MR has been underexplored. Patients (0 to ≤ 19 years) with MR who underwent mitral valve (MV) repair or replacement from 2015 to 2021 were included. Echocardiographically derived mean dP/dtic, Tei index, and EF were used to assess and compare ventricular function prior to, shortly after, and late after MV surgery. Study cohort included 61 patients (age 4.5 [IQR 0.14, 18.7] years, 89% MV repair, 11% MV replacement). Median time intervals between surgery and preoperative, early postoperative, and late postoperative echocardiograms were 6 days, 6 days, and 350 days, respectively. Median EF was 62% (z-score − 0.40) preoperatively, 56% (z-score − 1.40) early postoperatively, and 61% (z-score − 0.60) late postoperatively. Median dP/dtic was 1393 (IQR 1029, 1775) mmHg/s preoperatively, 1178 (IQR 886, 1946) mmHg/s early postoperatively, and 1270 (IQR 791, 1765) mmHg/s late postoperatively. Preoperative median dP/dtic correlated with early and late postoperative EF. Preoperative EF was not significantly correlated with early postoperative EF, but was correlated with late postoperative EF. Mitral valve intervention in pediatric patients is associated with an initial decline but subsequent recovery of systolic function. Non-invasively derived mean dP/dtic may offer advantages over other preoperative echocardiographic indices to predict postoperative systolic function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patients with chronic mitral regurgitation (MR) often develop left ventricular (LV) dysfunction over time secondary to the chronic volume overload imposed upon the LV by this lesion. This development has adverse prognostic implications. LV dysfunction is recognized by the American Heart Association (AHA) as an indication for surgical intervention for MR [1]. Surgical repair or replacement of the mitral valve usually prevents further deterioration of LV function in adults without congenital heart disease (CHD), but recovery of function is not routinely observed [2,3,4,5].
Assessment of LV function in the setting of significant MR is not straightforward. An incompetent mitral valve permits the LV to eject some of its blood into the low-pressure left atrium (LA). This form of afterload reduction will cause an increase in left ventricular ejection fraction (LVEF) unrelated to a change in the LV’s contractile state. As such, the AHA recommends mitral valve (MV) surgery in adults when the LVEF is ≤ 60%, 10 percentage points higher than that recommended for aortic valve intervention. MR also causes LV volume overload (increased preload) which also may affect the LVEF and other measures of ventricular function [2].
A variety of echocardiographic parameters have been proposed to detect subclinical LV dysfunction preoperatively in asymptomatic patients and may predict outcomes and dysfunction following MV surgery. In adults, echocardiographically determined preoperative mean dP/dtic (change in pressure over change in time during isovolumetric contraction) of the LV was found to be a better predictor of postoperative dysfunction than preoperative LVEF [6]. This may be because it possesses properties that render it ideal for the assessment of LV function. Moreover, the mean dP/dtic approximates and closely correlates with the (invasively measured) peak dP/dt. Similarly the echocardiographically determined Tei index has also been shown to be a sensitive metric to identify patients at risk for systolic dysfunction after MV repair [7, 8].
Assessment of LV function in pediatric patients with CHD and MV pathology is more challenging. The anatomic variations and segmental wall motion abnormalities encountered in patients with CHD may render the geometric assumptions required for the estimation of LVEF from standard two-dimensional (2D) echocardiography unreliable. Moreover, patients with CHD who have had multiple surgical procedures often have poor acoustic windows which may make accurate visualization of endocardial borders difficult and further compromise attempts to quantitatively assess LV function. Hence, in children under consideration for MV surgery, a more robust assessment of LV function beyond a reliance solely on LVEF seems warranted. It is possible that children are more resilient than their adult counterparts and that improvement in LV function would be more consistently observed but this has not been well studied [9]. The main aims of this study were (1) to determine if pediatric patients have recovery of LV function after mitral valve surgery and (2) to assess whether a more comprehensive assessment of LV function prior to surgery using noninvasive echocardiography-derived indices of mean dP/dtic and the Tei index is better than LVEF at identifying patients at risk for early and late postoperative dysfunction.
Methods
This was a single-center, retrospective cohort study. The Institutional Review Board (IRB-P00041058) approved the study and the requirement for individual informed consent was waived. The authors are solely responsible for the design and conduct of this study, all analyses, the drafting and editing of the paper, and its final contents.
Study Population
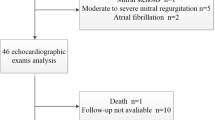
All patients (ages 1 month to ≤ 19 years) who underwent MV surgical repair or replacement for MR at Boston Children’s Hospital between September 2015 and April 2021 were screened for eligibility. Inclusion criteria required the availability of a preoperative echocardiogram (0–9 months prior to surgery) and at least one available early postoperative echocardiogram (0–6 weeks after surgery). If an additional postoperative echocardiogram was available (5 months to 2.5 years after surgery), it was also analyzed and considered to be the late postoperative study. When multiple echocardiographic studies were available for a given time interval, the earliest echocardiogram within that time interval was used. Patients with concomitant surgical procedures that may affect ventricular function (e.g., ventricular septal defect closure, coronary artery surgery, endocardial fibroelastosis resection, other valvular surgery, pacemaker implantation, Fontan palliation, left ventricular outflow tract surgery, or right ventricular outflow tract surgery) were excluded. Children with a repaired primary atrioventricular canal defect with recurrent MR were eligible but those with unrepaired atrioventricular canal with left-sided atrioventricular valve regurgitation were excluded. Patients with genetic diseases were included if they did not have a concomitant known underlying cardiomyopathy. Other secondary surgeries such as tricuspid valve or atrial septal defect repairs were allowed. All patients had at least moderate MR prior to their operation. Additionally, patients with inadequate image quality for analysis, insufficient electrocardiogram tracings on their echocardiogram study, non-sinus rhythm, frequent ectopy, a PR interval of > 0.24 s, or > 20 bpm discrepancy between the heart rate on the preoperative and postoperative studies were excluded.
Demographic, clinical, and baseline echocardiographic data were extracted from electronic medical records. In terms of surgical history, it was recorded if this was the first MV intervention (labeled primary surgery) and if any additional cardiac lesions were repaired at the time of MV intervention (labeled secondary surgery). Quantitative measurements of LVEF were obtained using the 5/6 area-length method [10]. Qualitative estimates of LV function were also collected from the corresponding echocardiography reports and graded on a 1–4 scale for normal function to severe dysfunction, respectively. In addition, if a catheterization was performed within 3 months prior to the operation, the LV end-diastolic pressure (LVEDP) was recorded. Patient last known follow-up, need for mitral valve reoperation, hospital length of stay, and days to extubation were also extracted from medical records.
Echocardiographic Protocol
Previously acquired 2D and Doppler echocardiograms obtained according to a standardized protocol were analyzed. In addition to the LVEF, we also measured the mean dP/dt during isovolumetric contraction (mean dP/dtic) as previously described [11]. Mean dP/dtic henceforth is referred to as dP/dtic. dP/dtic was calculated as the difference between the aortic diastolic blood pressure and LVEDP divided by isovolumetric contraction time (ICT). Briefly, the ICT was calculated by subtracting the time interval between a salient point on the QRS complex and the closure of the MV on the LV inflow Doppler tracing, from the time interval between the same point on the QRS complex and the opening of the aortic valve on the LV outflow Doppler tracing. An average of 3 measurements was used for the calculation. Standard pulse wave Doppler tracings rather than tissue Doppler indices or strain imaging (which may include these times) were used as they are more routinely performed at most centers and across the broader patient population (i.e., even in uncooperative toddlers and older children with poor acoustic windows). Aortic diastolic pressure was obtained from an automated blood pressure monitoring system using an appropriately sized cuff during the echocardiographic study. None of the patients had more than mild aortic regurgitation, which could adversely affect diastolic pressure measurements. In patients with a preoperative cardiac catheterization, the value of the LVEDP obtained during the catheterization was used for the calculation of dP/dtic. For those without preoperative catheterizations, LVEDP was assumed to equal 10.0 mm Hg, the median of the LVEDPs available from the subset of 18 patients with a catheterization (Table 1). For the postoperative studies, the LVEDP was assumed to have fallen by 2 mm Hg from preoperative values, due to the elimination/reduction of the MR. Note that because LVEDP is usually much less than aortic diastolic pressure, errors in the estimation of LVEDP introduce relatively small errors into the calculation of dP/dtic [12,13,14]. A normal dP/dtic is typically ~ 1100 mm Hg/s and LVEF that is two standard deviations below normal corresponds to a dP/dtic of ~ 850 mm Hg/s [13].
We also measured the Tei index, a marker of LV systolic and diastolic function that can be measured from the same Doppler tracings as the dP/dtic, as previously described [15]. Tei index is calculated as the sum of isovolumetric contraction and isovolumetric relaxation times divided by the ejection time. The sum of the isovolumetric times and ejection time (component ‘a’) was calculated by measuring the time interval between the closure and subsequent reopening of the MV inflow pulse Doppler tracing. Ejection time (component ‘b’) was calculated by measuring the time interval between the opening and subsequent closure of the aortic valve on the ventricular outflow pulsed Doppler tracing. Tei index was calculated as (a − b)/b. Again, an average of 3 measurements was used for the calculation. It is important to note that higher dP/dtic values represent better ventricular function and lower Tei index values represent better ventricular function. A normal Tei index is ~ 0.36 and a Tei index of ~ 0.50 is two standard deviations above (worse than) normal [15].
In addition to the above indices standard echocardiographic measurements for LA monoplane volume estimation, LV end-diastolic, and LV end-systolic volumes using the \({\raise0.7ex\hbox{$5$} \!\mathord{\left/ {\vphantom {5 6}}\right.\kern-\nulldelimiterspace} \!\lower0.7ex\hbox{$6$}}*\) area-length method were recorded. All echocardiographic measurements were undertaken by an experienced cardiologist as well as cardiology fellows (J. R., A.G., and R.N.) blinded to the status of the patient.
Data Analysis
Demographic, clinical, laboratory, and echocardiographic data were summarized using medians and either range or interquartile range (IQR) for continuous variables and frequencies and percentages for categorical variables. The Wilcoxon signed-rank test was used to compare echocardiographic measurements and assessments of ventricular function from the preoperative to early and late postoperative periods. Spearman rank correlation coefficients were used to identify relationships between preoperative, early postoperative, and late postoperative LVEF and ventricular function variables (Tei index, EF, and dP/dtic). Preoperative variables and outcomes were compared for patients with postoperative LVEF < 50% versus ≥ 50% using the exact Wilcoxon rank sum test. Analyses were performed using STATA version 16 (StataCorp, College Station, TX). P values ≤ 0.05 were deemed statistically significant.
Results
Baseline Characteristics
A total of 61 patients were enrolled (median age 4.5 [IQR 0.14, 18.7] years), 89% mitral valve repair, 11% mitral valve replacement, and 49% primary repair). The demographic and clinical characteristics are presented in Table 1. Determination of dP/dtic and the Tei index was possible at all 3 time points in 55 patients. The chief anatomic diagnoses for repair were reoperation of atrioventricular (AV) canal defects, MV prolapse, dysplastic MV, MV cleft, endocarditis, rheumatic heart disease, and transitional AV canal. Twenty-three percent of patients had a genetic syndrome. A total of 18 patients underwent a catheterization procedure preoperatively for which the LVEDP was a median of 10.0 mmHg. The median total hospital length of stay was 7 [IQR 3, 739] days and median follow-up was 4.3 [IQR 0.1, 8.1] years.
Echocardiographic Parameters
Conventional echocardiographic parameters and measurements of the Tei index and median dP/dtic for the cohort across the three time points are presented in Table 2. The median time interval between the preoperative study and surgery was 6 days, between the surgery and the early postoperative study was 6 days, and between the surgery and late postoperative study was 350 days. The majority of patients had qualitatively normal systolic function preoperatively (82%), early postoperatively (67%), and late postoperatively (88%). The median end-diastolic volume was lower postoperatively with a z-score of 1.00 early postoperatively and 1.30 late postoperatively compared to a preoperative z-score of 2.95 (P value < 0.001 and 0.001 comparing early and late postoperative to preoperative volume, respectively). The left atrial volume z-score was also lower postoperatively (2.75 early postoperatively and 2.85 late postoperatively) compared to a preoperative z-score of 3.70 (P value 0.001 and 0.024, respectively).
The median EF was 62% (IQR 58, 68%) preoperatively (Table 2). The early postoperative EF declined to 56% (IQR 50, 62%) and late postoperatively the EF improved to 61% (57, 64%) (Fig. 1; P value < 0.001 and 0.017 comparing preoperative to early and late postoperatively, respectively). The average Tei index showed a similar pattern, increasing from the preoperative to the early postoperative study and decreasing from the early to late postoperative study without recovering to the preoperative value (Fig. 1; Table 2). The median dP/dtic decreased from the preoperative to the early postoperative study and increased from the early to late postoperative study but also did not recover to the preoperative value (Fig. 1; Table 2). For the entire cohort, the median dP/dtic was 1393 (IQR 1029, 1775) mmHg/sec preoperatively, 1178 (IQR 886, 1946) mmHg/sec early postoperatively, and 1270 (IQR 791, 1765) mmHg/sec late postoperatively.
Correlation Between Markers of Ventricular Function
The correlations between markers of ventricular function are shown in Table 3. The preoperative EF was not correlated with the preoperative dP/dtic (rs = 0.02; P value = 0.88). The preoperative dP/dtic, however, was positively correlated with early postoperative EF (rs = 0.28; P value = 0.028) and late postoperative EF (rs = 0.37; P value = 0.01). Early postoperative dP/dtic was correlated with early postoperative EF (rs = 0.39; P value = 0.002). The preoperative EF was not significantly correlated with early postoperative EF (rs = 0.21, P value = 0.11) but was correlated with late postoperative EF (rs = 0.49, P value < 0.001). The preoperative Tei index was correlated with early postoperative EF (rs = − 0.28; P value = 0.032), but not late postoperative EF (rs = − 0.17; P value = 0.23).
Subset Analyses
Subset analyses comparing preoperative echocardiographic variables between patients with LV dysfunction (EF < 50%) in the early and late postoperative period versus those with normal EF (EF ≥ 50%) during the same time points are shown in Table 4. A total of 13 patients had early postoperative dysfunction and 47 had normal ventricular function. A total of 3 patients had late postoperative dysfunction compared to 46 patients with normal ventricular function. Those with ventricular dysfunction in the early postoperative period had higher preoperative end-diastolic and end-systolic volume z-scores and lower preoperative dP/dtic, whereas preoperative EF were similar. Those with late postoperative dysfunction had lower preoperative EF and dP/dtic. Patients with early and late dysfunction had a higher preoperative Tei index. Out of 35 patients with a preoperative EF > 60%, 7 had early postoperative EF ≤ 50% and 28 had early postoperative EF > 50%. Preoperative median dP/dTic was significantly lower in the group with early postoperative decrease in EF (1017 [IQR 795, 1406] mmHg/s compared to those with normal EF (1437 [IQR 1181, 1971] mmHg/s); P value 0.011. In the patient with the largest decrease in EF (71% to 36%) the preoperative mean dP/dtic was 722 mmHg/s.
Comparing those with normal early postoperative function to those with early postoperative dysfunction, the hospital length of stay (7 [IQR 5, 10] vs 6 [IQR 5, 12] days; P value 0.89) and time to extubation (1 [IQR 1,2] vs 1 [IQR 1,2] days; P value 0.57) were similar. There was no difference in the reoperation rates on the MV between those with and without early postoperative dysfunction (31% vs 28%; P value 1.0). Comparing the 8 patients with a low mean preoperative dP/dTic of ≤ 850 to the 53 patients with a normal mean preoperative dP/dTic of > 850, the rates of mitral valve reoperation were higher 5 (63%) versus 12 (23%), P value 0.032; however, the days to extubation (2 [IQR 1, 3] versus 1 [IQR 1, 2] days; P value 0.065), and hospital length of stay (7 [IQR 4, 15] vs 7 [IQR 5, 11] days; P value 0.99) were similar.
Discussion
We observed that in pediatric patients with chronic MR undergoing MV repair or replacement most patients preoperatively have preserved left ventricular systolic function, which declines in the early postoperative period and recovers in the late postoperative timeframe. This pattern was observed in all three echocardiographic indices that were studied (EF, dP/dtic, and Tei index), although the changes between time points did not always achieve statistical significance. In patients with a normal preoperative EF, a lower preoperative dP/dtic was able to distinguish patients who developed early postoperative dysfunction. This has important clinical implications to identify pediatric patients who may be at higher risk and need closer surveillance or therapies that are more intensive in the early postoperative period.
This study demonstrated a modest correlation between postoperative EF and preoperative Doppler-derived left ventricular dP/dtic as well as Tei index for pediatric patients undergoing surgical repair or replacement of the MV in the setting of MR. In contrast, the preoperative EF did not correlate with early postoperative EF. This suggests that in the setting of significant MR, EF may not accurately reflect the LV function and these alternative indices may be better suited in this scenario. This observation may relate to the fact that dP/dtic and Tei index do not rely on geometric assumptions or good acoustic windows and are less affected by the loading changes caused by MR compared to EF. Mean dP/dtic approximates and closely correlates with the invasively measured peak dP/dt. Peak dP/dt is sensitive to changes in contractility and is only modestly affected by changes in preload [14]. Because of the close agreement between peak dP/dt and dP/dtic, it is reasonable to ascribe these properties to dP/dtic as well. Furthermore, it can easily be calculated from measurements of the diastolic blood pressure and acquired Doppler tracings of the aortic and mitral valves [6, 11].
In adults with chronic MR, the regurgitation tends to get worse over time and decreased contractility often develops despite an often normal EF [16]. In those who develop an EF 50–60% and particularly EF < 50% the prognosis is guarded [4]. Similar to the adult literature, we observed in our pediatric cohort that contractility may be reduced despite a normal EF and that those with a preserved EF preoperatively also had a preserved EF at late follow-up [16]. It is not a common practice to perform a catheterization in pediatric patients with this disease. Therefore, echocardiography remains standard of care for routine disease surveillance. As such, Doppler-based measures such as dP/dtic and the Tei index may have additional advantages in young children in whom obtaining accurate volumetric data can be challenging without the use of sedation. In adults undergoing MV surgery for MR, echocardiographically determined dP/dtic as an index of ventricular function was found to be one of the best predictors of postoperative EF [6]. While outcomes of hospital length of stay, days to extubation, and MV reoperation rates were not different between those patients with normal versus abnormal preoperative EF, a low mean preoperative dP/dtic was associated with need for mitral valve reoperation and trended toward significance for longer time to extubation suggesting it may have clinical utility.
Similar to published studies in adults without CHD, we found that preoperative dP/dtic correlated modestly with early and late postoperative EF, whereas preoperative EF correlated only with late postoperative EF. This may be because chronic MR causes LV dilatation from adaptive remodeling to the volume overload [6]. Consequently, the EF preoperatively often remains in normal ranges despite significant impairment of LV contractility [2, 16]. Prior studies on adults found a stronger correlation (r 0.75) between preoperative dP/dtic and postoperative EF, which likely reflects the overall relatively small sample of patients in our cohort and, in particular, those with depressed ventricular function postoperatively.
Limitations
This was a single-center retrospective analysis of a relatively small cohort. The majority of patients had normal LVEF preoperatively and postoperatively which may have affected our results. Mitral valve anatomy, indications for surgery, and follow-up of patients who underwent interventions were not standardized. As a referral center, many patients were excluded who were lost to follow-up or who did not have ongoing care at our institution. Additionally, time intervals between the echocardiographic measurements varied significantly from individual to individual. The estimation of dP/dtic has potential sources of error including the assumption of LVEDP in some patients as well as use of cuff diastolic pressure as a surrogate for aortic diastolic pressure. Nonetheless, large errors in the estimation of LVEDP introduce only small errors in the calculation of dP/dtic. Moreover, if, as is likely, an improvement in ventricular function is associated with a fall in LVEDP > 2 mmHg, our methodology would have, if anything, underestimated the pressure change during ICT.
Conclusion
In pediatric patients with chronic MR, MV intervention is associated with an initial decline, but long-term recovery of left ventricular function. In these patients, Doppler-derived indices of left ventricular performance in the form of dP/dtic and Tei index may better identify patients at risk of postoperative LV dysfunction compared to EF. Further investigation is warranted to ascertain whether these indicators surpass EF in predicting clinical outcomes, such as functional status, and the clinical relevance of these findings.
Data Availability
No datasets were generated or analysed during the current study
References
Otto CM, Nishimura RA, Bonow RO et al (2020) ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. https://doi.org/10.1161/CIR.0000000000000923
Nishimura RA, Otto CM, Bonow RO et al (2014) AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. https://doi.org/10.1161/CIR.0000000000000029
Crawford MH, Souchek J, Oprian CA et al (1990) Determinants of survival and left ventricular performance after mitral valve replacement. Circulation. https://doi.org/10.1161/01.CIR.81.4.1173
Enriquez-Sarano M, Tajik AJ, Schaff HV, Orszulak TA, Bailey KR, Frye RL (1994) Echocardiographic prediction of survival after surgical correction of organic mitral regurgitation. Circulation 90(2):830–837. https://doi.org/10.1161/01.CIR.90.2.830
Starling MR (1995) Effects of valve surgery on left ventricular contractile function in patients with long-term mitral regurgitation. Circulation. https://doi.org/10.1161/01.CIR.92.4.811
Pai RG, Bansal RC, Shah PM (1990) Doppler-derived rate of left ventricular pressure rise. Its correlation with the postoperative left ventricular function in mitral regurgitation. Circulation. https://doi.org/10.1161/01.CIR.82.2.514
Mabrouk-Zerguini N, Léger P, Aubert S et al (2008) Tei index to assess perioperative left ventricular systolic function in patients undergoing mitral valve repair. Br J Anaesth. https://doi.org/10.1093/bja/aen212
Bruch C, Schmermund A, Dagres N, Katz M, Bartel T, Erbel R (2002) Tei-index in symptomatic patients with primary and secondary mitral regurgitation. Int J Cardiovasc Imaging. https://doi.org/10.1023/A:1014664418322
Krishnan US, Gersony WM, Berman-Rosenzweig E, Apfel HD (1997) Late left ventricular function after surgery for children with chronic symptomatic mitral regurgitation. Circulation. https://doi.org/10.1161/01.CIR.96.12.4280
Margossian R, Chen S, Sleeper LA et al (2015) The reproducibility and absolute values of echocardiographic measurements of left ventricular size and function in children are algorithm dependent. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2015.01.014
Joyce J, O’Leary ET, Mah DY, Harrild DM, Rhodes J (2020) Cardiac resynchronization therapy improves the ventricular function of patients with fontan physiology. Am Heart J. https://doi.org/10.1016/j.ahj.2020.09.018
Rhodes J, Margossian R, Sleeper LA et al (2011) Non-geometric echocardiographic indices of ventricular function in patients with a fontan circulation. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2011.07.006
Rhodes J, Fulton DR, Levine JC, Marx GR (1997) Comparison between the mean dP/dt during isovolumetric contraction and other echocardiographic indexes of ventricular systolic function. Echocardiography. https://doi.org/10.1111/j.1540-8175.1997.tb00713.x
Rhodes J, Udelson JE, Marx GR et al (1993) A new noninvasive method for the estimation of peak dP/dt. Circulation. https://doi.org/10.1161/01.CIR.88.6.2693
Cui W, Roberson DA (2006) Left ventricular tei index in children: comparison of tissue Doppler imaging, pulsed wave Doppler, and M-mode echocardiography normal values. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2006.06.006
Starling MR, Kirsh MM, Montgomery DG, Gross MD (1993) Impaired left ventricular contractile function in patients with long-term mitral regurgitation and normal ejection fraction. J Am Coll Cardiol. https://doi.org/10.1016/0735-1097(93)90840-W
Funding
S.B. is supported by the Fred Lovejoy Housestaff Research and Education Fund. A.G. is supported by NIH 5 T32 HL007572-35 Research Methods in Pediatric Heart Disease.
Author information
Authors and Affiliations
Contributions
S.E., J.R., and S.B. conceptualized the design. J.R., A.G., and R.N. performed ventricular measurements. F.S. and K.G. performed the statistical analysis and created the figure. A.G., S.J.G, J.R., and N.T. wrote the main manuscript text and prepared the tables. All authors reviewed the manuscript
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical Approval
This article has achieved Institutional Review Board approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gearhart, A., Thatte, N., Bassi, S. et al. Preoperative Echocardiographically Derived Mean dP/dTic Predicts Early Post-operative Dysfunction in Children Undergoing Mitral Valve Surgery. Pediatr Cardiol (2024). https://doi.org/10.1007/s00246-024-03584-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-024-03584-9