Abstract
Data comparing surgical systemic-to-pulmonary artery shunt and patent ductus arteriosus (PDA) stent as the initial palliation procedure for patients with pulmonary atresia with intact ventricular septum (PA-IVS) are limited. We sought to compare characteristics and outcomes in a multicenter cohort of patients with PA-IVS undergoing surgical shunts versus PDA stents. We retrospectively reviewed neonates with PA-IVS from 2009 to 2019 in 19 United States centers. Bivariate comparisons and multivariable logistic regression analysis were performed to determine the relationship between initial palliation strategy and outcomes including major adverse cardiovascular events (MACE): stroke, mechanical circulatory support, cardiac arrest, or death. 187 patients were included: 38 PDA stents and 149 surgical shunts. Baseline characteristics did not differ statistically between groups. Post-procedural MACE occurred in 4 patients (11%) with PDA stents versus 38 (26%) with surgical shunts, p = 0.079. Overall, the initial palliation strategy was not significantly associated with MACE (aOR:0.37; 95% CI,0.13–1.02). In patients with moderate-to-severe right ventricle hypoplasia, PDA stents were significantly associated with decreased odds of MACE (aOR:0.36; 95% CI,0.13–0.99). PDA stents were associated with lower vasoactive inotrope scores (median 0 versus 5, p < 0.001), greater likelihood to be extubated at the end of their procedure (37% versus 4%, p < 0.001), and shorter duration of mechanical ventilation (median 24 versus 96 h, p < 0.001). PDA stents were associated with significantly more unplanned reinterventions for hypoxemia compared to surgical shunts (42% vs. 20%, p = 0.009). In this multicenter study, neonates with PA-IVS who underwent PDA stenting received less vasoactive and ventilatory support postoperatively compared to those who had surgical shunts. Furthermore, patients with the most severe morphology had decreased odds of MACE.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary atresia intact ventricular septum (PA-IVS) is a rare cardiac defect, accounting for only 1% of congenital heart diseases [1]. It is characterized by complete obstruction of right ventricular outflow, an intact ventricular septum, and varying degrees of tricuspid valve and right ventricular hypoplasia. Neonatal intervention also varies, dependent on the degree of right ventricle (RV) hypoplasia and the presence of RV-dependent coronary circulation (RVDCC). For example, patients with adequate RV chamber size and no coronary abnormalities commonly undergo RV decompression to establish RV-PA continuity with the goal of biventricular repair, whereas those with RVDCC, severe coronary abnormalities or clinical signs of coronary ischemia may undergo a heart transplantation as the primary neonatal management [2]. In the subset of patients with inadequate RV chamber size, palliative surgical shunt placement with or without right ventricle decompression was traditionally performed. In more recent years, placement of a stent in the patent ductus arteriosus (PDA) via cardiac catheterization has been utilized as an alternative initial palliative procedure in some patients.
Survival had historically been poor for PA-IVS patients with hypoplastic RV, with reported neonatal mortality of 20–34% but has improved to less than 10% within the current era [3,4,5,6,7,8,9]. While mortality has improved, recovery without morbidity following neonatal intervention continues to be challenging. In a multicenter study of 279 patients with PA-IVS, Leung et al. demonstrated that 1 in 5 patients had major adverse cardiac events (MACE) post-procedural intervention, including stroke (6%), mechanical circulatory support (9%), cardiopulmonary resuscitation (CPR) (13%), and death (8%) [4]. The highest frequency of MACE occurred in the subset of patients with hypoplastic right ventricle who underwent palliation with surgical shunt placement or PDA stenting as the initiation intervention. A recent meta-analysis of retrospective studies comparing surgical shunt to PDA stenting in mixed cohorts of patients with congenital heart defects showed those who underwent PDA stent had reduced risk of mortality, post-procedural mechanical circulatory support, and other complications [10]. To our knowledge, there are no published studies focused on patients with PA-IVS that have compared outcomes following these procedures. We utilized contemporary multicenter data from Collaborative Research from the Pediatric Cardiac Intensive Care Society (CoRe-PCICS) to compare the characteristics and post-procedural outcomes, including major adverse cardiovascular events (MACE), of patients with PA-IVS undergoing traditional surgical systemic-to-PA shunt placement versus PDA stent placement.
Patients and Methods
The study was approved by the Institutional Review Board of each participating center and the data coordinating center at Cincinnati Children’s Hospital Medical Center (ID: 2019-0708; 24 May 2019). Parental consent was waived given the retrospective nature of the study.
We conducted a multicenter retrospective cohort study across 19 United States hospitals affiliated with CoRe-PCICS. Participating centers are listed in Supplemental Table 1. We reviewed the records of all neonates (age less than 30 days) with PA-IVS admitted in participating centers over a 10-year period, from 01-01-2009 until 12-31-2018. We included patients who underwent either a PDA stent or surgical shunt as their initial palliation in the study. Patients with antegrade blood flow across the pulmonary valve and those with any size ventricular septal defects were excluded. Additionally, in keeping with previous reports, we excluded patients with Ebstein’s anomaly or severely dysplastic tricuspid valve [11]. The diagnosis of PA-IVS and evaluation for exclusion criteria were based on the initial echocardiogram report. Data were extracted from electronic medical records, surgical, echocardiography and cardiac catheterization databases as available in each participating hospital by local investigators. Anonymized data were recorded in a centralized REDCap database and reviewed at the data coordinating center for missingness and plausibility. Tricuspid valve Z-scores were based on apical 4-chamber measurements as documented in the initial echocardiogram report (before any intervention). The definition of RVDCC was not standardized but rather based on the assessment of the local care team at the time of the initial hospitalization. Patients were categorized as having RVDCC only if it was explicitly stated in cardiac catheterization reports or elsewhere in the medical record. Patients that had unclear documentation regarding the status of coronary circulation were considered “unknown RVDCC.”
Our primary outcome was frequency and risk of MACE (defined as CPR, mechanical circulatory support, stroke or hospital mortality). Secondary outcomes of interest were post-procedure vasoactive support (defined as vasoactive inotrope score [12] on admission to the ICU and at 12 h postoperatively), nosocomial infection, necrotizing enterocolitis, renal failure, duration of mechanical ventilation, length of ICU stay, and unplanned procedures after the initial palliation. Renal failure was defined as oliguria with sustained urine output < 0.5 cc/kg/hr for 24 h and/or a rise in creatinine > 1.5 times upper limits of normal for age, with need for dialysis (including peritoneal dialysis and/or hemodialysis) or hemofiltration [13] The diagnosis of stroke was determined by review of available post-procedural brain imaging by site principal investigators.
Statistical Analysis
Median with 25th–75th percentile and frequency with percent were used to summarize patient demographics and clinical characteristics. Bivariate comparisons of characteristics and clinical outcomes according to the initial intervention group (surgical shunt versus PDA stent) were made using Wilcoxon rank-sum tests for continuous variables and chi-squared tests for categorical variables.
A multivariable logistic regression model with the initial intervention group (PDA stent vs. surgical shunt) as a primary independent variable was used to estimate the adjusted odds ratio (aOR) and 95% confidence interval (CI) for MACE. The model covariates were chosen a priori based on clinical experience with patients with PA-IVS and included preoperative inotropic support, preoperative ventilation, RVDCC status, and right ventricular decompression (RVD) as part of initial palliation. Robust standard errors computed via the Huber-White method were used to correct for the clustering of patients within hospitals. A subgroup analysis was performed on patients with moderate-to-severe RV hypoplasia using similar methods. P-values < 0.05 were considered statistically significant. All statistical analyses were performed using the R statistical program (version 4.3.1) [14]. The rms package (version 6.7.1) [15] was used to perform logistic regression models.
Results
Patient Characteristics
We reviewed a total of 187 patients with PA-IVS, of which 149 underwent surgical systemic-to-PA shunt placement and 38 underwent PDA stent placement. Of these 187 cases, 36 patients (19%) had simultaneous right ventricular decompression: 25 (17%) underwent surgical shunt and 11 (29%) who underwent PDA stent (p = 0.142). Baseline characteristics of patients who underwent surgical shunt are compared to patients who underwent PDA stent placement in Table 1. More patients who underwent surgical shunt placement were mechanically ventilated prior to the procedure (58% vs. 37%, p = 0.028). Other baseline characteristics including age and weight were not statistically different between groups.
The number of patients undergoing shunts and PDA stents varied across centers (Fig. 1). All centers performed surgical shunts whereas 11 out of 19 centers performed PDA stents. The median number of surgical shunts was 6 per center (range: 1–22) versus 1 per center for PDA stents (range: 0–16).
The expected end-stage circulation at the time of the procedure for all patients, as judged by the clinical teams at each center, is summarized in Fig. 2. Single ventricle physiology was the expected end-stage circulation for the majority of patients: 98 (66%) with surgical shunt versus 24 (64%) with PDA stent. Heart transplantation was ultimately anticipated in 15 patients (10%) with a surgical shunt and 3 patients (8.1%) with PDA stent. Of the patients who received surgical shunts, 130 (87.2%) received a modified Blalock-Taussig-Thomas (BTT) shunt and 19 (12.8%) underwent a central shunt. Characteristics of surgery, type, and size of shunts are provided in Supplementary Table 2.
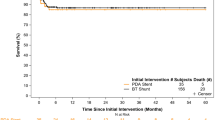
Major Adverse Cardiovascular Events
MACE occurred in 42 (22%) patients: 4 (11%) with PDA stent vs. 38 (26%) with surgical shunt (p = 0.079). Table 2 compares the rate of each MACE based on the initial surgical intervention. Hospital mortality occurred in 17 (9.1%) patients, of which 15 (10%) underwent surgical shunt compared to 2 (5.3%) who underwent PDA stent (p = 0.546). No significant difference was observed in the frequency of CPR, mechanical circulatory support, or strokes, between the groups.
The multivariable model for factors associated with post-procedural MACE is provided in Table 3. Multivariable analysis of all patients in our cohort demonstrated that, when compared to surgical shunt as the initial procedure, odds for MACE for patients who underwent PDA stent were not significantly different (aOR 0.37; 95% CI, 0.13–1.02, p = 0.056). We found no evidence of association of preoperative ventilation, RV decompression, and RVCC status with MACE, whereas the presence of preoperative inotropic support was associated with increased risk of MACE (aOR 2.31; 95% CI, 1.01–5.30; p = 0.047). However, in the subgroup analysis of patients with moderate-to-severe right ventricle hypoplasia, PDA stents were inversely associated with MACE compared to surgical shunts (aOR 0.36; 95% CI, 0.13–0.99, p = 0.047). In this more extreme morphologic cohort, the presence of preoperative inotropic support was also associated with an increased risk of MACE (aOR 3.10; 95% CI, 1.28–7.50; p = 0.012) (Table 4).
Post-procedural Hospital Outcomes
Table 5 summarizes the short-term hospital outcomes between the two groups. There was a significant difference in the vasoactive inotropic score during the post-procedural period between the two groups, with a median score of 0 in patients with PDA stents compared to a median score of 5 in the patients with surgical shunts on CICU admission (p < 0.001) and at 12 h of admission (p < 0.001). Notably, there was also a significant difference in the post-procedural mechanical ventilation utilization. More patients with PDA stents were extubated at the end of the procedure compared to patients with surgical shunts (37% vs. 4%, p < 0.001). Additionally, total post-procedural ventilation time after the first initial palliation was significantly shorter in patients with PDA stents (median 24 vs. 96 h, p < 0.001). There was no difference in the ICU or hospital length of stay (LOS) with PDA stents compared to surgical shunts: median 12 vs. 17 days (p = 0.146) and median 27 vs. 29 days (p = 0.271), respectively.
Unplanned Interventions
Details of all unplanned procedures prior to discharge are summarized in Supplementary Table 3. Unplanned procedures performed for hypoxemia, which were deemed to be related to the choice of procedure (i.e., PDA stent versus surgical shunt), are compared in Table 6. Unplanned procedures for hypoxemia were significantly more frequent in patients who underwent PDA stenting (p = 0.009). The most common unplanned procedure for hypoxemia in patients with PDA stents was re-intervention with PDA stent angioplasty (n = 8, 21%). The most common unplanned intervention in patients with surgical shunts was shunt revision including banding or de-banding (n = 16, 11%), shunt balloon angioplasty or shunt stenting (n = 8, 5%). Notably, 4 patients (10%) subsequently underwent a BTT shunt placement after the initial PDA stent procedure.
Discussion
In this contemporary multicenter cohort of patients with PA-IVS undergoing either a surgical systemic-to-pulmonary artery shunt or PDA stent as the initial palliation, the incidence of MACE was substantial, occurring in 1 out of 5 patients. The overall risk of MACE was similar between the two groups; however, within the subset of patients with moderate-to-severe right ventricle hypoplasia, PDA stents were associated with a lower risk of MACE compared to surgical shunts. Additionally, patients undergoing PDA stenting received significantly less post-procedure inotropic support and had a shorter duration of post-procedural invasive mechanical ventilation.
Several retrospective single-center and multicenter studies have evaluated the outcomes of PDA stents vs. systemic-to-pulmonary shunts in neonates with heterogenous types of congenital heart defects with positive findings supporting the use of PDA stenting as an alternative to surgical shunts. Fakhry [10] et al. performed a systematic review and meta-analysis of 6 published multicenter and single-center studies, showing a significant reduction in risk of mortality, complications, and use of ECMO in patients with PDA stenting compared to systemic-arterial shunt. Utilizing data from the Congenital Catheterization Research Collaborative (CCRC), Glatz and colleagues compared the outcomes of 106 patients with PDA stents and 251 patients with modified Blalock-Taussig-Thomas shunts in a heterogeneous group of patients with congenital heart disease [16]. No difference was demonstrated in the primary outcome of death or unplanned reinterventions to treat cyanosis. Similarly, in a large national audit from the United Kingdom, Bentham and colleagues reviewed 170 patients with modified BTT shunts and 83 patients with PDA stents and reported an increased survival to discharge for the PDA stent group [17]. In keeping with our findings, both these large multicenter studies demonstrated fewer ventilator days with the PDA stent group compared to surgical shunts.
Our study results aligned with the findings of published literature, but specifically for patients with PA-IVS. While the mortality rate is lower in our cohort of patients compared to published literature [3, 5,6,7, 9], the rate of MACE was significantly striking at 22%. The overall risk of MACE was similar in PA-IVS undergoing either the PDA stents or surgical shunts; however, it is noteworthy that in subsets of patients with moderate-to-severe RV hypoplasia, PDA stents were associated with significantly lower odds of MACE compared to surgical shunts. A possible reason for the high risk of MACE in our study could be due to the morphological severity of our PA-IVS patient cohort. Patients in our study demonstrated significant RV hypoplasia with the median tricuspid valve z-score of − 3.5 and 93% of patients had at least moderate-to-severe RV hypoplasia. Diminutive tricuspid valve and RV size are associated with the presence of coronary abnormalities, which may account for the increased susceptibility to MACE [9, 18]. Interestingly, we found that RVDCC, as designated by the primary centers, was not a predictor of MACE within our patient cohort. The wide heterogeneity of the definition and interpretation of RVDCC across centers likely contributed to this finding.
While vasoactive scores do not entirely reflect the hemodynamic status of patients as they can be variable based on the discretion of the treating team, the consistently higher vasoactive inotropic score across centers in the surgical shunt group implied a perceived greater need for cardiovascular support after surgical shunts compared to PDA stents. Given the heightened circulatory vulnerabilities in patients PA-IVS, the impact of post-procedural vasoactive drugs on the susceptibility to MACE is unclear.
The less invasive nature of PDA stents was evident in that PA-IVS patients who underwent PDA stenting were more likely to be extubated at the end of the procedure and had shorter mechanical ventilation duration. The avoidance of surgical stress, specifically cardiopulmonary bypass associated acute lung injury, and the earlier return to extubation status can theoretically account for less sympathetic activation and possibly more favorable myocardial oxygen balance, possibly positively influencing the susceptibility to MACE.
Despite the shorter length of ventilation time in patients undergoing PDA stents as the initial evaluation, the ICU and hospital LOS were not statistically different in patients undergoing PDA stents compared to surgical shunts in our cohort of patients. In contrast, the CCRC study and the UK national registry study demonstrated a significantly shortened ICU and hospital LOS for patients undergoing PDA stents vs. surgical shunts [16, 17]. Our ICU and hospital LOS were also considerably higher compared to patients in those two studies. For instance, the median LOS in the CCRC study for PDA stents vs. surgical shunts was 4 days vs. 7 days (p < 0.001) while our median ICU LOS was 12 vs. 17 days (p = 0.146). The likely reason for this notable difference is due to differences in our patient population compared to the patient population in the CCRC study. This is the first report to compare PDA stents vs. surgical shunts in only PA-IVS neonates, with significant morphology. 38% of all patients in our cohort were designated to have RVDCC by the local primary team. > 60% of our patients in both the PDA stent and surgical shunt cohorts were expected to have a single ventricle physiology, whereas > 60% of the cohort of patients in the PDA stent group in the CCRC study were expected to have 2-ventricle physiology [16]. Moreover, feeding difficulties is common and an important factor in determining the length of stay both in the ICU and in the total hospital LOS for these high-risk patients with shunted physiology. As shown on Table 5, less than 50% of our patients were exclusively PO fed at discharge. Therefore, it would have been unlikely for our cohort of patients to achieve ICU discharge status at 4 or 7 days, as reported by the CCRC study for their PDA stent and surgical patients, respectively. Although there was a trend toward a shorter LOS in the PDA stent patients, our smaller sample size might have masked small differences that exist between the two groups. Additionally, the higher rate of unplanned re-intervention in patients undergoing PDA stents as the initial palliation may have also contributed to the overall length of stay in that group.
The result of our study further reinforces the value of PDA stents as a contemporary alternative to surgical shunts, with an appreciable advantage in decreased post-procedural morbidity and decreased risk of MACE in a subset of PA-IVS patients with moderate-to-severe RV hypoplasia. However, patients who underwent PDA stenting underwent a significantly higher number of unplanned interventions for hypoxemia compared to surgical shunts. The CCRC study did not observe a difference in the unplanned intervention for hypoxemia but found overall an increased frequency of unplanned procedures after PDA stents compared to BTT shunts [16]. The higher rate of unplanned procedures for PDA stents was also reported in the United Kingdom multicenter study [17]. Notably, in our study, 10% of PDA stent patients were converted to BTT shunt after the initial procedure among the unplanned interventions. This higher rate of unplanned interventions could be reflective of differences in the development of intraluminal stenosis of PDA stents versus surgical shunts, center practice variations, or the learning-curve associated with a relatively novel procedure compared to traditional surgical shunts. Nonetheless, acknowledging this consistent observation is important and should be factored into the decision-making process for patients with PA-IVS.
The strength of our study is our multicenter design involving diverse institutions, allowing for the collection of a large cohort of patients with this rare congenital cardiac lesion. However, this design also resulted in several limitations to our study. Given its multicenter and retrospective nature, there may be practice and procedural variability among centers that we could not account for. The decision to proceed with PDA stent vs. surgical shunt by each center was not clearly delineated in the medical records and may reflect institutional bias. There was a preference for surgical shunts at most participating centers, with only 11 out of 19 centers performing PDA stents whereas all centers performed surgical shunts. There was one center that performed 16 PDA stents over the study period, but the median number of PDA stents for each center was only 1, reflecting relative inexperience with this interventional approach for this cohort of patients, which may have affected the post-procedural outcomes, including the higher rate of unplanned intervention for PDA stents compared to unplanned intervention rate for surgical shunts. Another limitation of our study was that we could not assess whether there was a trend for increased utilization of PDA stents as the first palliative procedure over surgical shunts throughout our study period, as we did not collect the exact procedural dates. As PDA stenting becomes more common and experience with PDA stenting increases, future studies should be performed to determine if the trends and post-procedural outcomes observed in our study demonstrate improvement over time.
Additionally, in our study, the diagnosis of stroke was determined by the review of available post-procedural brain imaging by site principal investigators, which may contribute to variability in the interpretation of clinically relevant imaging findings. Furthermore, the growing ubiquity of postoperative MRI imaging may have resulted in an increased number of stroke diagnoses. One reason for the higher rate of MACE in our cohort of patients was due to the relatively higher rate of stroke, as determined by site investigators (5.3% in PDA stents and 5.4% in surgical shunts, p > 0.999). A recent review of perioperative brain MRI in children undergoing cardiac surgery showed that 50% had new postoperative radiological abnormalities: 29% of which were infarcts and 9% were hemorrhages [19]. The clinical implications of radiologic evidence of “strokes” rather than clinically relevant diagnoses are uncertain.
Lastly, even though our study was comprised of the largest reported cohort of patients with PA-IVS undergoing PDA stent vs. surgical shunt, our study may be underpowered to detect statistically significant differences in other outcomes between the groups. Moreover, our current study was only focused on short-term post-procedural outcomes. Future studies are needed to evaluate relevant and important long-term outcomes between the two groups including longitudinal survival, pulmonary artery growth, as well as neurodevelopmental outcomes.
Conclusion
Surgical systemic-to-pulmonary artery shunts remained overwhelmingly more common over PDA stents across multicenter sites for our contemporary cohort of patients with PA-IVS. The rate of post-procedural MACE for both groups was high, occurring in 1 out of 5 patients. PDA stenting was associated with decreased early post-procedural morbidity, and while there was no difference in the overall risk of MACE associated with each procedure, PDA stents may confer a reduced risk of MACE in the subset of PA-IVS patients with moderate-to-severe RV hypoplasia. On the other hand, unplanned interventions to address hypoxemia were significantly more frequent following PDA stenting compared to surgical shunt placement. Altogether, PDA stents should be considered a valuable contemporary alternative to surgical shunts in patients with PA-IVS.
Data availability
No datasets were generated or analysed during the current study.
Change history
17 June 2024
The duplicate word “Included were” was removed from the abstract.
References
Daubeney PEF, Delany DJ, Anderson RH et al (2002) Pulmonary atresia with intact ventricular septum: range of morphology in a population-based study. J Am Coll Cardiol 39:1670–1679. https://doi.org/10.1016/S0735-1097(02)01832-6
Chikkabyrappa SM, Loomba RS, Tretter JT (2018) Pulmonary atresia with an intact ventricular septum: preoperative physiology, imaging, and management. Semin Cardiothorac Vasc Anesth 22:245–255. https://doi.org/10.1177/1089253218756757
Sukhavasi A, McHugh-Grant S, Glatz AC et al (2022) Pulmonary atresia with intact ventricular septum: intended strategies. J Thorac Cardiovasc Surg 164:1277–1288. https://doi.org/10.1016/J.JTCVS.2021.11.104
Cheung EW, Mastropietro CW, Flores S et al (2022) Procedural outcomes of pulmonary atresia with intact ventricular septum in neonates: a multicenter study. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2022.07.055
Hannan RL, Zabinsky JA, Stanfill RM et al (2009) Midterm results for collaborative treatment of pulmonary atresia with intact ventricular septum. Ann Thorac Surg 87:1227–1233. https://doi.org/10.1016/J.ATHORACSUR.2009.01.040
Lydia WK, Knight J, Thomas AS et al (2019) Long-term outcomes after intervention for pulmonary atresia with intact ventricular septum congenital heart disease. Heart 105:1007–1013. https://doi.org/10.1136/heartjnl-2018-314124
Ashburn DA, Blackstone EH, Wells WJ et al (2004) Determinants of mortality and type of repair in neonates with pulmonary atresia and intact ventricular septum. J Thorac Cardiovasc Surg 127:1000–1008. https://doi.org/10.1016/J.JTCVS.2003.11.057
Iliopoulos I, Mastropietro CW, Flores S et al (2022) Pulmonary atresia with Intact ventricular septum: midterm outcomes from a multicenter cohort. Pediatr Cardiol. https://doi.org/10.1007/S00246-022-02954-5
Hanley FL, Sade RM, Blackstone EH et al (1993) Outcomes in neonatal pulmonary atresia with intact ventricular septum: a multiinstitutional study. J Thorac Cardiovasc Surg 105:406–427. https://doi.org/10.1016/s0022-5223(19)34223-0
Fakhry AbdelMassih A, Menshawey R, Menshawey E et al (2022) Blalock-taussig shunt versus ductal stent in the palliation of duct dependent pulmonary circulation; a systematic review and metanalysis. Curr Probl Cardiol 47:100885. https://doi.org/10.1016/J.CPCARDIOL.2021.100885
Liava’a M, Brooks P, Konstantinov I et al (2011) Changing trends in the management of pulmonary atresia with intact ventricular septum: the melbourne experience. Eur J CardioThorac Surg 40:1406–1411. https://doi.org/10.1016/J.EJCTS.2011.02.036
Gaies MG, Gurney JG, Yen AH et al (2010) Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 11:234–238. https://doi.org/10.1097/PCC.0b013e3181b806fc
Alten JA, Cooper DS, Blinder JJ et al (2021) Epidemiology of acute kidney injury after neonatal cardiac surgery: a report from the multicenter Neonatal and pediatric heart and renal outcomes network. Crit Care Med 49:E941–E951. https://doi.org/10.1097/CCM.0000000000005165
R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, https://www.R-project.org/
Harrell FJr rms: Regression modeling strategies. R package version 6.7.1
Glatz AC, Petit CJ, Goldstein BH et al (2018) Comparison between patent ductus arteriosus stent and modified Blalock-Taussig Shunt as palliation for infants with ductal-dependent pulmonary blood flow: insights from the congenital catheterization research collaborative. Circulation 137:589–601. https://doi.org/10.1161/CIRCULATIONAHA.117.029987/-/DC1
Bentham JR, Zava NK, Harrison WJ et al (2018) Duct stenting versus modified Blalock-Taussig Shunt in neonates with duct-dependent pulmonary blood flow: associations with clinical outcomes in a multicenter national study. Circulation 137:581–588. https://doi.org/10.1161/CIRCULATIONAHA.117.028972/-/DC1
Daubeney PE, Wang D, Delany DJ et al (2005) Pulmonary atresia with intact ventricular septum: predictors of early and medium-term outcome in a population-based study Daubeney et al. surgery for congenital heart disease. J Thorac Cardiovasc Surg 130:1071. https://doi.org/10.1016/j.jtcvs.2005.05.044
Alablani FJ, Chan HSA, Beishon L et al (2022) Paediatric brain MRI findings following congenital heart surgery: a systematic review. Arch Dis Child 107:818–825. https://doi.org/10.1136/archdischild-2021-323132
Funding
This study received intramural funding from Heart Institute Research Core at Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Data collection, and analysis were performed by BNP, II and HZ. The first draft of the manuscript was written by BNP and subsequently revised based on all authors' comments. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Puente, B.N., Mastropietro, C.W., Flores, S. et al. Comparison of Ductal Stent Versus Surgical Shunt as Initial Intervention for Neonates with Pulmonary Atresia with Intact Ventricular Septum. Pediatr Cardiol (2024). https://doi.org/10.1007/s00246-024-03529-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-024-03529-2