Abstract
Atrioventricular reentrant tachycardia (AVRT) is the most common form of supraventricular tachycardia in newborns. AVRT is sometimes refractory to conventional antiarrhythmic therapy. We describe our experience about the use of the triple combination of flecainide + propranolol + amiodarone as third-line regimen for refractory and recurrent AVRT in newborns. We considered a series of 14 patients who had failed both first-line and second-line therapy and were treated using the combination of flecainide + propranolol + amiodarone. Transoesophageal electrophysiologic study (TES) was performed to test the effectiveness of medical therapy during hospitalization and to try to reduce the amount of therapy, after amiodarone wash-out, before 1 year of age. TES was repeated at 1 year of age to test the spontaneous resolution of the arrhythmia after treatment discontinuation. Rhythm control was achieved in all 14 patients. At a mean age of 9.3 ± 2 months, AVRT was not inducible by TES in 11/12 amiodarone-free patients. At a mean age of 14.1 ± 3 months, AVRT was still inducible in 7/12 patients after interrupting the entire antiarrhythmic therapy (58.3%). Triple combination was effective as third-line option to suppress AVRT refractory to single and double antiarrhythmic therapy, with no significant adverse events. Our experience suggests that triple therapy could be maintained for a short-term treatment, discontinuing amiodarone before 1 year of age to avoid long-term side effects. Newborns who needed triple therapy appear to have a lower chance of accessory pathway disappearance at 1 year of age. TES could be useful for risk stratification of recurrences at the time of drug discontinuation in infants considered to be at higher risk of recurrent AVRT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrioventricular reentrant tachycardia (AVRT) is the most common form of supraventricular tachycardia (SVT) in newborns. Antiarrhythmic therapy has been showed to be safe and effective to suppress the arrhythmia until spontaneous resolution, which is usually observed by 1 year of age [1,2,3,4]. Sodium channel blockers (class IC antiarrhythmics), beta blockers (class II antiarrhythmics), digoxin and class III antiarrhythmic drugs are traditionally used as single agents, or in combination therapy when monotherapies fail to control the arrhythmia [5,6,7,8]. Nevertheless, AVRT is recurrent and refractory to conventional antiarrhythmic therapy for some newborns [9,10,11]. Furthermore, transcatheter ablation, which represents to date the most effective treatment for this arrhythmia, is burdened by a high risk of morbidity and mortality in this age group [3]. This clinical scenario poses a clinical challenge. A third-line regimen using a combination therapy of three drugs is possible: however, limited data are available in literature concerning its use in this selected population.
The aim of this study was to describe our experience about the use of the combination of flecainide, propranolol and amiodarone as triple antiarrhythmic therapy for control of refractory and recurrent AVRT in newborns.
Methods
We performed a systematic review of the medical records of all newborns who were referred to the Paediatric Cardiology Unit of our Hospital (Monaldi Hospital, Naples, Italy) between January 2012 and December 2022 because of occurrence of SVT after birth. This observational, retrospective, case series study complied with the Declaration of Helsinki and its later amendments and was approved by local ethics committee. Written informed consent was obtained from the patient’s parents/legal guardians in each case.
Inclusion Criteria and Data Collection
Inclusion criteria consisted of (a) diagnosis of AVRT, (b) age ≤ 28 days at the time of diagnosis, (c) failure of single and double antiarrhythmic therapy to obtain complete rhythm control, (d) use of the combination of three antiarrhythmic drugs (flecainide + propranolol + amiodarone) in the attempt to control the SVT.
We collected data about the following clinical features for all patients: gestational age at birth, presence of fetal tachycardia and fetal heart failure, weight at birth, age at diagnosis of AVRT, mean heart rate during tachycardia, associated cardiac malformations or congenital heart diseases (CHD), presence of cardiac dysfunction or respiratory distress, drug therapy, side effects, surface electrocardiogram (ECG) abnormalities during treatment and at discharge, blood chemistry tests (including kidney, liver and thyroid function tests) at discharge, age and weight at discharge. Furthermore, we collected clinical, laboratory and instrumental data during follow-up.
Diagnostic Criteria of AVRT
Diagnosis of AVRT was obtained on admission on surface ECG (Fig. 1) and confirmed by transoesophageal electrophysiologic study (TES) according to the following criteria: narrow QRS tachycardia, fixed 1:1 atrioventricular relationship, regular RR interval, VA interval < AV interval with fixed VA interval ≥ 70 ms, abrupt onset and offset, induction by programmed atrial stimulation or incremental atrial pacing, interruption by overdrive atrial pacing. TES was performed using a 6 Fr or 7 Fr transoesophageal catheter. We performed incremental atrial pacing down to a cycle length of 200 ms and programmed atrial stimulation with single, double and triple extrastimuli (down to 200 ms) at different drive cycle lengths (between 450 and 300 ms) to induce AVRT when not present at baseline. We also delivered short bursts of rapid atrial pacing at 200 ms and 180 ms. Overdrive atrial pacing at least 30 ms shorter than the spontaneous tachycardia cycle length was used for interruption of the tachycardia (Fig. 2).
Clinical Management of AVRT
Acute management of sustained AVRT on admission included (a) diving reflex, (b) adenosine administration (rapid intravenous bolus of 0.1 mg/kg to a maximum of 0.3 mg/kg), (c) overdrive atrial pacing. In case of early recurrences after sinus rhythm restoration, intravenous (IV) antiarrhythmic therapy was required with flecainide (1–1.5 mg/kg in 10 min), magnesium sulphate infusion (100 mg/kg in 24 h) or amiodarone infusion (10 mg/kg in 24 h).
After acute management and stable sinus rhythm restoration, a multiple step oral antiarrhythmic therapy was started to prevent AVRT recurrences. Waiting time to assess the efficacy of each treatment step was defined according to specific medications’ half-lives and time to steady state concentrations: we respected a 72-h minimum duration of treatment for flecainide, sotalol or propranolol and 7 days minimum duration for amiodarone after each step and after each dose increase. Complete rhythm control was defined as suppression of AVRT to no more than sporadic premature atrial complexes along with lack of inducibility of sustained AVRT during TES. Triple drug therapy was introduced after the evidence of failure of at least one single drug regimen and one dual therapy regimen to obtain complete rhythm control.
Our typical workflow included to start a single drug regimen with flecainide as first-line therapy, with a starting dose of 3–4 mg/kg daily and titrated up to a maximum dose of 6 mg/kg daily. Alternative options were propranolol, sotalol or amiodarone alone. The starting dose of propranolol was 1–2 mg/kg daily and titrated up to 4–5 mg/kg daily; the starting dose of sotalol was 3–4 mg/kg daily and titrated up to a maximum dose of 6 mg/kg daily. We used amiodarone as first-line single drug therapy only for newborns with severely impaired ventricular function, with an initial dose of 10 mg/kg daily and titrated up to 15 mg/kg daily. Drug doses were increased up to their target dose as mentioned above, according to clinical response and weight gain of the babies due to growth. In case of AVRT recurrences or inducibility despite first-line treatment, even at the maximum dosage, a second-line therapy was started with two possible options: (a) add a second drug (combination of flecainide + propranolol, flecainide + sotalol, flecainide + amiodarone or propranolol + amiodarone) and titrate both as mentioned above; (b) switch to a different class of drug (e.g., from flecainide to propranolol or sotalol or amiodarone) and then to combined therapy after failure of the new single drug regimen. In case of failure of the combined treatment as well, the newborns were switched to a different dual therapy regimen or to a third-line therapy with the combination of flecainide + propranolol + amiodarone.
Surface ECG, Holter monitoring, on-ward telemetry and TES were used to assess effectiveness of drug regimens and to exclude AVRT recurrences or inducibility. Surface ECGs were obtained and reviewed daily during therapy, evaluating PR interval, QRS complexes and corrected QT (QTc) interval. QTc was calculated using Bazett’s formula (QTcB = QT/RR1/2) and was considered normal when ≤ 460 ms. All patients were monitored via telemetry for the entire duration of hospitalization. ECG Holter monitoring was analysed to exclude arrhythmias and to assess maximal, minimal and average heart rate during treatment (Fig. 3). Transthoracic echocardiography (TTE) was performed at the time of admission to assess cardiac chamber dimensions, ventricular function and to exclude associated cardiac malformations or CHDs; we repeated TTE in case of worsening of clinical status during hospitalization and before discharge. Kidney, liver and thyroid function were monitored during treatment by laboratory tests to exclude drug side effects.
Follow-up
After discharge, all patients were scheduled to a regular follow-up at our Pediatric Arrhythmology outpatient clinic at 2 weeks, at 4 weeks and every 4–12 weeks intervals thereafter, evaluating clinical status, physical examination, surface ECG, TTE, results of laboratory tests and 24-h ECG Holter recording. Attention was given to presence of growth impairment (height and weight), regular or poor feeding, signs of heart failure, signs of drug toxicity, abnormal ECG changes or episodes of arrhythmia on ECG Holter monitoring. Laboratory tests (including kidney and liver function tests, TSH, FT3 and FT4) were repeated at 2 weeks follow-up and every 4–12 weeks intervals thereafter, according to clinical status, to eventually exclude medication side effects.
Infants were admitted at least 6-months after discharge for a new TES, after amiodarone wash-out, to try to reduce the amount of therapy. Amiodarone was discontinued at least 30 days before the procedure, according to its long half-life. If AVRT was not inducible during TES and no spontaneous episodes of tachycardia were recorded during hospitalization and previous follow-up, dual therapy was considered effective and continued using the same doses of flecainide and propranolol; otherwise, triple combination therapy was resumed with unchanged or increased doses, according to the patient’s weight.
TES was repeated after a two-step wash-out from therapy at 1 year of age, to test the spontaneous resolution of the tachycardia. Propranolol was discontinued at least 72 h before the admission. In patients without inducible AVRT, flecainide was interrupted and TES was repeated after 72 h. If AVRT was still not inducible, even during isoproterenol infusion, accessory pathway was considered disappeared and drug therapy was ceased. Treatment was resumed in patients with inducible AVRT.
Statistical Analysis
Data are presented as mean ± standard deviation or median and interquartile range (IQR) for continuous variables as appropriate and as frequencies and percentages for dichotomous variables, checking continuous variables for normality with the Kolmogorov–Smirnov test. This study is descriptive, with no inferential statistics performed.
Results
Patient Characteristics
Fourteen patients met the inclusion criteria and represented the cohort of this study. Clinical characteristics of the patients on admission are summarized in Table 1. Mean gestational age at the time of delivery was 36.7 ± 2.4 weeks. Mean weight at birth was 2.9 ± 0.6 kg. Mean age at the time of diagnosis of AVRT was 5.2 ± 7.4 day (median: 1 day). Four patients had episodes of SVT during intrauterine life and one of them developed ventricular dysfunction with signs of hydrops fetalis. Mean heart rate during AVRT was 261 ± 16 bpm. Three newborns presented signs of ventricular preexcitation on surface ECG.
TTE on admission showed an ostium secundum atrial septal defect (OS ASD) in 9/14 cases, patent foramen ovale (PFO) in 4/14 cases and patent ductus arteriosus (PDA) in 6/14 cases: watchful waiting during follow-up was sufficient in all cases except for one patient who underwent surgical closure of hemodynamically significant PDA. One patient had diagnosis of multiple cardiac rhabdomyomas in tuberous sclerosis complex. Bicuspid aortic valve was diagnosed in one case. No complex CHDs were found.
Two infants presented with depressed cardiac contractility (ejection fraction 25–30%) and clinical signs of heart failure along with respiratory failure due to nearly incessant tachycardia: IV therapy (included antiarrhythmic drugs and diuretics) and invasive ventilation were required because clinical status was critical. Two patients developed a transient respiratory distress and one patient an isolated mild reduction of ejection fraction (45%) due to the presence of persistent AVRT.
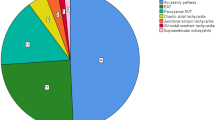
Drug Therapy
Acute suppression of sustained AVRT was obtained by diving reflex, adenosine injection or overdrive atrial pacing in almost all cases at admission. Three patients needed IV antiarrhythmic therapy in the early phase of hospitalization to control refractory AVRT. After acute management, oral prophylactic therapy was started. The most used first-line medication for AVRT in neonates was flecainide (12/14 patients), except for children with severely impaired ventricular function which were initially treated using amiodarone. Nine patients were treated using one regimen of dual therapy (9/14), four patients using two regimens (4/14) and one patient using three regimens (1/14). The most used second-line regimen was combination of flecainide + propranolol (10/14 patients). Triple therapy was started when each patient had failed at least one single drug regimen and one dual therapy regimen. Complete rhythm control was achieved in all patients after introduction of combination therapy with flecainide + propranolol + amiodarone within the first or second week of treatment. Efficacy was documented by serial surface ECGs, 24-h Holter monitoring and telemetry (complete suppression of spontaneous episodes of AVRT) and confirmed by TES (lack of induction of sustained AVRT) performed at least 7 days after the beginning of the triple therapy.
Side Effects
Four newborns reported an isolated mild increase of TSH levels by age (not exceeding 11 mUI/L) that did not require any specific treatment but a dose reduction of amiodarone. FT3 and FT4 values resulted within the normal age-specific reference interval in all infants. Mean TSH value at discharge was 6.3 ± 2.8 mUI/L, mean FT3 value was 4.2 ± 0.5 ng/mL, mean FT4 value was 1.6 ± 0.3 ng/dL. Kidney and liver function tests were found to be in the normal range by age in all cases. No other clinical effects that could be related to amiodarone administration (gastrointestinal, neurologic, dermatologic or pulmonary toxicity) were noted.
A slight QTc increase was observed in two patients during triple therapy (maximum value recorded 482 ms). QTc prolongation was managed by a dose adjustment of amiodarone in both cases. At discharge, mean QTc value was 436 ± 18 ms. One patient developed a transient mild widening of QRS (130 ms) during triple therapy which resolved after a dose reduction of flecainide. No proarrhythmic effects (bradycardia, torsades de pointe or other ventricular arrhythmias) or atrioventricular node disturbance were noted during combination therapy.
TTE showed normal cardiac function at the time of discharge in all cases. At discharge, the mean dose of flecainide was 3.3 ± 1.1 mg/kg daily, the mean dose of propranolol was 2.4 ± 1.3 mg/kg daily and the mean dose of amiodarone was 8.1 ± 1.8 mg/kg daily. Mean weight at discharge was 3.9 ± 0.6 kg. Mean age at discharge was 37 ± 17 days.
Follow-up
After discharge, all infants had a good weight gain and height growth without complications during strict follow-up at our Paediatric Arrhythmology outpatient clinic. Mean follow-up from diagnosis to last clinical evaluation was 32.5 ± 30 months (range 8–121 months). The doses of individual medications were adjusted according to the rapid weight gain of the infants, maintaining doses similar to those reached at discharge in the first months and subsequently applying a mild and progressive reduction during follow-up. Spontaneous episodes of tachycardia that were clinically relevant did not occur. Furthermore, no episodes of AVRT or other significant arrhythmias were documented on surface ECGs or Holter recordings. The ECG Holter monitoring was repeated during follow-up at 2 weeks, at 4 weeks and every 4–12 weeks intervals thereafter. None of the patients developed signs of amiodarone or flecainide toxicity. No patient had iatrogenic dysthyroidism, liver or kidney toxicity: serum creatinine, AST, ALT, FT3, FT and TSH values remained within the age-specific normal range during the follow-up period. No neurologic, pulmonary or dermatologic side effects were noted. Growth in height and weight was in the normal range for age in all infants. One patient (patient #4) developed a slight increase of QTc interval that was easily managed by a mild dose reduction of flecainide and amiodarone.
Twelve out of 14 infants reached at least 6-months after discharge and were admitted to our ward after discontinuation of amiodarone. The dosages of individual medications that maintained rhythm control until that time were as follows: flecainide 2.6 ± 0.7 mg/kg daily + propranolol 1.4 ± 0.5 mg/kg daily + amiodarone 4.6 ± 1 mg/kg daily. Mean duration of triple therapy was 226 ± 73 days (median 210 days). Mean age at the time of second hospitalization to perform TES was 9.3 ± 2 months. AVRT was not inducible by TES in 11/12 amiodarone-free patients, therefore they were discharged on dual therapy with flecainide + propranolol. Sustained AVRT was inducible in one patient (#5), so triple combination therapy was resumed. Two patients completed 6 months of treatment and are currently on waiting list for TES without amiodarone.
At the mean age of 14.1 ± 3 months, all these 12 patients were admitted to test the disappearance of the accessory pathway. Among them, sustained AVRT was still inducible by TES in 7 patients. Three patients were tested positive without propranolol on single therapy with flecainide. Consequently, double therapy with flecainide + propranolol was restarted. Three patients were tested negative without propranolol but positive without flecainide. Thus, single therapy with flecainide was resumed using the same effective dose. Patient #5 repeated a new TES without amiodarone and was tested positive again, therefore triple combination therapy was restarted. In the other 5 cases, AVRT was not inducible: the accessory pathway was considered to be disappeared and antiarrhythmic treatment was discontinued. Among the more complex patients, the child with history of hydrops fetalis was tested positive without propranolol. Two patients with Wolff-Parkinson-White (WPW) syndrome were tested negative without propranolol but positive without flecainide. The younger child with WPW was on waiting list for TES without amiodarone. On the contrary, the patient with tuberous sclerosis and rhabdomyomas was tested negative without propranolol and then without flecainide. During follow-up, the child began to suffer from epilepsy and started therapy with levetiracetam and vigabatrin.
All patients tested negative by TES after withdrawal of the prophylactic treatment had no recurrences during follow-up. Among the 7 infants tested positive by TES at 1 year of age, maintenance therapy was continued in all cases. At 2–3 years, four out of 7 children underwent a new TES after medication wash-out to exclude a late disappearance of the accessory pathway, but it still confirmed inducibility of AVRT. Patient #5 was tested negative without amiodarone but positive after discontinuation of propranolol and flecainide. One of them (patient #10) was again tested positive at the age of 6 and finally underwent radiofrequency catheter ablation of two concealed accessory pathways (left and right posteroseptal accessory pathway) at the age of 10, when parents gave us consent.
Discussion
The aim of the antiarrhythmic treatment is to control and prevent episodes of AVRT until spontaneous resolution of the arrhythmia substrate [11,12,13,14]. Prolonged or incessant episodes of tachycardia can promote development of tachycardia-induced cardiomyopathy with reduced ejection fraction and hemodynamic impairment, leading to high morbidity and poor outcome, especially in neonates and infants [6]. Furthermore, the presence of an accessory pathway has been associated with an increased risk of sudden cardiac death as a result of rapid antegrade conduction of high atrial frequencies to the ventricles [15, 16].
A high percentage of resolution (60–90%) has been defined for infants with diagnosis of AVRT after drug discontinuation at 1 year of age [17,18,19,20,21]. It was advocated that tachycardia is more likely to recur in patients with ventricular preexcitation [6,7,8], history of episodes of AVRT during intrauterine life, late diagnosis (> 60 days of age), need for second-line therapies and/or multi-antiarrhythmic drugs [4, 20]. Infants with early diagnosis (< 60 days of age), without ventricular preexcitation, and discharged on first-line monotherapy (propranolol) showed to be at lower recurrence risk [5, 20, 21].
Optimal medical management for control of AVRT in newborns and infants has not been well defined yet. To date, the overwhelming majority of patients are maintained on prophylactic drug therapy after tachycardia suppression: the standard practice is to continue treatment for 6–12 months, following which medications are often discontinued [1, 4, 17, 20, 21]. Several pharmacological regimens have been described in literature [9,10,11,12,13,14]. Medication choices were influenced by personal preference and experience and by the presence of ventricular preexcitation, with digoxin being not used in case of manifest preexcitation on surface ECG [3,4,5, 20]. In our institution, the most used first-line medication for AVRT in neonates and infants is usually a sodium-channel blocker. Flecainide is highly effecting in blocking both anterograde and retrograde conduction through the accessory pathway [1], with low significant proarrhythmic effects (mainly QRS widening) or adverse events [9,10,11,12,13,14], sometimes due to inappropriate use [22]. We prefer flecainide over propafenone because of our wide experience with this medication and the need of a lower number of daily administrations. [11]. Propranolol is the main beta-blocker we use for treatment of AVRT in infants, with low incidence of side effects (bradycardia, hypotension or hypoglycemia) [4, 5]. Sotalol is also a good choice as single drug or combination therapy for AVRT, delaying both conduction over the accessory pathway and ventricular repolarization [1, 11, 23]. However, careful monitoring of ECG is mandatory, given the risk of QTc prolongation and ventricular arrhythmias at high doses [11]. Considering the multiple amiodarone-induced adverse effects in children, we rarely use it as first-line therapy for AVRT, except for children with severely impaired ventricular function, switching to other drugs when haemodynamic stability is reached. We prefer amiodarone as second- or third-line combination therapy with flecainide and/or propranolol. Despite its wide use in other centres, digoxin use was abandoned at our Unit because of its narrow therapeutic window, the need for monitoring of serum levels, its potential drug interactions and lower efficacy compared with other drugs, as flecainide [4, 5, 14].
If these drugs fail to control the arrhythmia as monotherapies, dual antiarrhythmic therapy is usually initiated. Different regimens have been described in literature (combination of flecainide + sotalol, flecainide + amiodarone, flecainide + propranolol) [1, 9, 13]. In our experience, all these combinations are good options as second-line treatment for recurrent AVRT in infants. However, dual combination therapy sometimes fails as well. In these cases, catheter ablation could be attempted. Nevertheless, interventional therapy carries a high risk of morbidity and mortality in infants in the first months of age, even in tertiary referral centres with high experience [3]. The high risks related to the procedure and the natural history of AVRT reinforce and justify the importance of searching for alternative medical regimens for this population.
Drago et al. [24] reported 4 patients in a cohort of 55 infants who needed triple therapy with flecainide + propranolol + amiodarone to suppress SVT, after evidence of failure of different regimens with one or two drugs. They found that the use of amiodarone was the only predictor of persistence of the re-entry circuit at 1 year of age assessed by TES [24]. Moore et al. [20] reported 9 patients among 460 infants who required triple antiarrhythmic therapy: 7 patients were treated using flecainide + propranolol + amiodarone, one patient using flecainide + digoxin + amiodarone and one patient using propranolol + digoxin + amiodarone. Considering this evidence, to the best of authors’ knowledge, this study describes to date the largest cohort of newborns with diagnosis of refractory AVRT treated by triple combination therapy.
Triple therapy probably enhanced arrhythmia control for the combination of different mechanisms of action on refractory periods of both the accessory pathway and the atrioventricular node. Moreover, the sum of the effects of this antiarrhythmics agents made it possible to reduce the average dose of each individual drug, with a consequent probable reduction of the amount of side effects. A warning on this approach could be the need for multiple drug administrations by parents or guardians, leading to possible errors. Therefore, parents/guardians must be instructed very well on proper administration at discharge and during follow-up [22].
We have presented our experience in treating refractory AVRT with a multiple step oral antiarrhythmic therapy. TES was a valuable tool to guide medical therapy and to test effectiveness of each treatment step during hospitalisation, in view of its high negative predictive value [25]. Moreover, TES was useful to try to reduce the amount of therapy, after amiodarone wash-out, before 1 year of age. Our study shows that an earlier amiodarone discontinuation could be considered after short treatment course, to avoid its long-term side effects. It suggests that triple therapy might just be needed in the early phase of treatment to achieve rhythm control.
TES was used for risk stratification of recurrences after weaning from antiarrhythmic therapy at 1 year of age, as previously reported in literature [24, 25]. Currently, the use of TES for SVT inducibility is not standard of care, but is performed at many institutions to guide clinical management of these patients. Conversely, the other standard is weaning medications as an outpatient and performing intermittent ambulatory cardiac monitoring. In consideration of the presence of an accessory pathway such as to determine recurrent episodes of tachycardia refractory to conventional first and second line therapies, we tested by TES the safety of interrupting the antiarrhythmic therapy at 1 year of age. Our workflow included a two-step wash out from propranolol and then from flecainide. This workflow allowed us to better distinguish between children that still needed dual therapy to suppress AVRT inducibility and children who just needed one single therapy, obtaining a further reduction of medical therapy, reaching the minimal effective therapy for rhythm control. This important data would not have been obtained by carrying out the test after discontinuing all drugs at the same time followed by a single TES, and even more, after discontinuing one or two drugs and directing the patients to Holter monitoring only. It has been shown that AVRT inducibility may be useful in determining which infants are at increased risk for recurrences [25, 26]. However, inducibility by TES may not necessarily mean clinical risk of SVT. Not all infants with SVT require chronic prophylaxis, and untreated infants could have no documented recurrences, especially infants with features consistent with a low risk profile. Nevertheless, we considered our approach a safer option than stopping one or two medications and doing Holter monitoring for these selected children considered to be at higher risk of recurrences, in view of the presence of one or more of the following features: need for multi-antiarrhythmic drugs (including amiodarone), presence of ventricular preexcitation, history of fetal AVRT or hydrops fetalis, history of tachycardia-induced cardiomyopathy (development of reduced ejection fraction and hemodynamic impairment). We observed a relatively high percentage of inducibility of AVRT (58.3%). Hence, we identified a group of patients who would have been at increased risk of relapse of tachycardia after drug therapy discontinuation due to the lack of resolution of the accessory connection. Furthermore, the impact on the families cannot be underestimated. The greater sense of reassurance reported by parents after a negative test result (lack of inducibility) should not be overlooked and could justify the need for hospitalization to carry out the procedure. At the same time, parents reported a greater sense of safety in knowing that their children with persistent AVRT inducibility were maintained on antiarrhythmic therapy and strict follow-up than without treatment, bearing in mind the previous history of recurrent arrhythmia and long hospitalization after birth.
Limitations
The main limitations of this study mostly relate to the retrospective single-centre design with a small cohort of patients. We recognize some confounding factors, as referral bias to different treatment regimens before triple therapy initiation or changes in responsible referring physicians during hospitalizations and follow-up, with implications in medical management, according to personal preference and experience. Triple therapy was used in treatment‐resistant AVRT in newborns aged between 0 and 28 in this study; therefore, our results could be limited to this selected subgroup. We could not collect serum flecainide levels for all patients during hospitalization since specific laboratory test was not previously available at our hospital, which would have given further interesting information about correlation between efficacy, side effects and plasma drug concentrations. Further studies with larger size of sample are warranted to confirm our results and to establish the optimal management in infants at higher risk of recurrent tachycardia.
Conclusion
Triple combination therapy with flecainide + propranolol + amiodarone was effective as a third-line option in our cohort of newborns to suppress AVRT refractory to conventional single and double antiarrhythmic therapy, with no significant adverse effects. Our experience suggests that triple therapy could be maintained for a short-term duration of treatment after rhythm control is reached. Amiodarone could be safely discontinued in the majority of patients before 1 year of age to avoid its long-term side effects. Newborns who needed triple therapy to suppress AVRT appear to have a lower chance of accessory pathway disappearance at 1 year of age, with an increased risk of relapse after discontinuation of antiarrhythmic therapy. TES could be useful for risk stratification of recurrence at the time of drug discontinuation in infants considered to be at higher risk of recurrent tachycardia.
References
Price JF, Kertesz NJ, Snyder CS, Friedman RA, Fenrich AL (2002) Flecainide and sotalol: a new combination therapy for refractory supraventricular tachycardia in children <1 year of age. J Am Coll Cardiol 39(3):517–520. https://doi.org/10.1016/s0735-1097(01)01773-9
Perry JC, Garson A Jr (1990) Supraventricular tachycardia due to Wolff-Parkinson-White syndrome in children: early disappearance and late recurrence. J Am Coll Cardiol 16(5):1215–1220. https://doi.org/10.1016/0735-1097(90)90555-4
Srinivasan C, Balaji S (2019) Neonatal supraventricular tachycardia. Indian Pacing Electrophysiol J 19(6):222–231. https://doi.org/10.1016/j.ipej.2019.09.004
Bruder D, Weber R, Gass M, Balmer C, Cavigelli-Brunner A (2022) Antiarrhythmic medication in neonates and infants with supraventricular tachycardia. Pediatr Cardiol 43(6):1311–1318. https://doi.org/10.1007/s00246-022-02853-9
Sanatani S, Potts JE, Reed JH, Saul JP, Stephenson EA, Gibbs KA, Anderson CC, Mackie AS, Ro PS, Tisma-Dupanovic S, Kanter RJ, Batra AS, Fournier A, Blaufox AD, Singh HR, Ross BA, Wong KK, Bar-Cohen Y, McCrindle BW, Etheridge SP (2012) The study of antiarrhythmic medications in infancy (SAMIS): a multicenter, randomized controlled trial comparing the efficacy and safety of digoxin versus propranolol for prophylaxis of supraventricular tachycardia in infants. Circ Arrhythm Electrophysiol 5(5):984–991. https://doi.org/10.1161/CIRCEP.112.972620
Schoenfeld MH (1990) Pediatric pre-excitation: say “no” to drugs? J Am Coll Cardiol 16(5):1221–1223. https://doi.org/10.1016/0735-1097(90)90556-5
Deal BJ, Keane JF, Gillette PC, Garson A Jr (1985) Wolff-Parkinson-White syndrome and supraventricular tachycardia during infancy: management and follow-up. J Am Coll Cardiol 5(1):130–135. https://doi.org/10.1016/s0735-1097(85)80095-4
Lundberg A (1973) Paroxysmal tachycardia in infancy: follow-up study of 47 subjects ranging in age from 10 to 26 years. Pediatrics 51(1):26–35
Ferlini M, Colli AM, Bonanomi C, Salvini L, Galli MA, Salice P, Ravaglia R, Centola M, Danzi GB (2009) Flecainide as first-line treatment for supraventricular tachycardia in newborns. J Cardiovasc Med (Hagerstown) 10(5):372–375. https://doi.org/10.2459/JCM.0b013e328329154d
Cunningham T, Uzun O, Morris R, Franciosi S, Wong A, Jeremiasen I, Sherwin E, Sanatani S (2017) The safety and effectiveness of flecainide in children in the current era. Pediatr Cardiol 38(8):1633–1638. https://doi.org/10.1007/s00246-017-1707-5
Kahr PC, Moffett BS, Miyake CY, Kim JJ, Valdes SO (2021) “Second line medications” for supraventricular arrhythmias in children: In-hospital efficacy and adverse events during treatment initiation of sotalol and flecainide. J Cardiovasc Electrophysiol 32(8):2207–2215. https://doi.org/10.1111/jce.15077
Kohli V (2013) Oral flecainide is effective in management of refractory tachycardia in infants. Indian Heart J 65(2):168–171. https://doi.org/10.1016/j.ihj.2013.02.009
Fenrich AL Jr, Perry JC, Friedman RA (1995) Flecainide and amiodarone: combined therapy for refractory tachyarrhythmias in infancy. J Am Coll Cardiol 25(5):1195–1198. https://doi.org/10.1016/0735-1097(94)00513-p
O’Sullivan JJ, Gardiner HM, Wren C (1995) Digoxin or flecainide for prophylaxis of supraventricular tachycardia in infants? J Am Coll Cardiol 26(4):991–994. https://doi.org/10.1016/0735-1097(95)00291-9
Sarubbi B, D’Alto M, Vergara P, Calvanese R, Mercurio B, Russo MG, Calabrò R (2005) Electrophysiological evaluation of asymptomatic ventricular pre-excitation in children and adolescents. Int J Cardiol 98(2):207–214. https://doi.org/10.1016/j.ijcard.2003.10.017
Sarubbi B, Scognamiglio G, Limongelli G, Mercurio B, Pacileo G, Pisacane C, Russo MG, Calabrò R (2003) Asymptomatic ventricular pre-excitation in children and adolescents: a 15 year follow up study. Heart 89(2):215–217. https://doi.org/10.1136/heart.89.2.215
Weindling SN, Saul JP, Walsh EP (1996) Efficacy and risks of medical therapy for supraventricular tachycardia in neonates and infants. Am Heart J 131(1):66–72. https://doi.org/10.1016/s0002-8703(96)90052-6
Tortoriello TA, Snyder CS, Smith EO, Fenrich AL Jr, Friedman RA, Kertesz NJ (2003) Frequency of recurrence among infants with supraventricular tachycardia and comparison of recurrence rates among those with and without preexcitation and among those with and without response to digoxin and/or propranolol therapy. Am J Cardiol 92(9):1045–1049. https://doi.org/10.1016/j.amjcard.2003.06.002
Riggs TW, Byrd JA, Weinhouse E (1999) Recurrence risk of supraventricular tachycardia in pediatric patients. Cardiology 91(1):25–30. https://doi.org/10.1159/000006873
Moore JA, Stephens SB, Kertesz NJ, Evans DL, Kim JJ, Howard TS, Pham TD, Valdés SO, de la Uz CM, Raymond TT, Morris SA, Miyake CY (2022) Clinical predictors of recurrent supraventricular tachycardia in infancy. J Am Coll Cardiol 80(12):1159–1172. https://doi.org/10.1016/j.jacc.2022.06.038
Aljohani OA, Herrick NL, Borquez AA et al (2021) Antiarrhythmic treatment duration and tachycardia recurrence in infants with supraventricular tachycardia. Pediatr Cardiol 42:716–720. https://doi.org/10.1007/s00246-020-02534-5
Correra A, Merola A, Palma M, Romeo E, Colonna D, Passariello A, Russo MG, Sarubbi B (2021) A frightening giant QRS complex in a 3-months-old infant. J Electrocardiol 66:16–17. https://doi.org/10.1016/j.jelectrocard.2020.07.012
Sarubbi B, Ducceschi V, Briglia N, Mayer MS, Santangelo L, Iacono A (1998) Compared effects of sotalol, flecainide and propafenone on ventricular repolarization in patients free of underlying structural heart disease. Int J Cardiol 66(2):157–164. https://doi.org/10.1016/s0167-5273(98)00201-0
Drago F, Silvetti MS, De Santis A, Marcora S, Fazio G, Anaclerio S, Versacci P, Iodice F, Di Ciommo V (2008) Paroxysmal reciprocating supraventricular tachycardia in infants: electrophysiologically guided medical treatment and long-term evolution of the re-entry circuit. Europace 10(5):629–635. https://doi.org/10.1093/europace/eun069
Kulakowski P, Dluzniewski M, O’Nunain S, Camm AJ, Wardzynska M, Ceremuzynski L (1992) The value of transesophageal atrial pacing in predicting the efficacy of antiarrhythmic drugs in patients with paroxysmal narrow QRS complex tachycardia. Pacing Clin Electrophysiol 15(6):895–904
Benson DW Jr, Dunnigan A, Benditt DG, Thompson TR, Narayan A, Boros S (1985) Prediction of digoxin treatment failure in infants with supraventricular tachycardia: role of transesophageal pacing. Pediatrics 75(2):288–293
Acknowledgements
Special thanks to the Paediatric and Adult Congenital Heart Disease Unit nursing staff and specially to the head nurses Mrs. Assunta Carandente, Mrs Monica Iacona and Mrs Annunziata Orefice for their essential contribution and support in maintaining high-quality standard of care for our patients. We thank our data manager Dr. Gabriella Piccolo, Dr. Nadia Puzone, Dr. Cecilia Spinelli Barrile and Dr. Tiziana Varriale for their support in data collecting and analysis.
Funding
No funding sources have been given for this study.
Author information
Authors and Affiliations
Contributions
GDC and BS contributed to write, review, and production of tables/figures. DC, AC, GP and ER contributed to data collection and review. MTP, NDC and MGR contributed to review. All authors approved the manuscript text.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no relationships that could be construed as a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ciriello, G.D., Colonna, D., Papaccioli, G. et al. Triple Antiarrhythmic Therapy in Newborns with Refractory Atrioventricular Reentrant Tachycardia. Pediatr Cardiol 44, 1040–1049 (2023). https://doi.org/10.1007/s00246-023-03162-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-023-03162-5