Abstract
The arterial baroreceptor reflex in children and adolescents has not been well studied in the current literature with a lack of agreed upon normal values, particularly in postural orthostatic tachycardia syndrome (POTS) or neurocardiogenic syncope (NCS). We used the sequence method and head-up tilt test (HUTT) to evaluate baroreceptor function in 3 phases: baseline supine position for 10 min, head-up position at 70° for 30 min or until syncope, and post-tilt supine reposition for 10 min. We measured the number of baroreceptor events, baroreceptor effectiveness index (BEI), and the magnitude of sensitivity of the events at each phase of HUTT. We studied 198 individuals (49 normal subjects, 67 POTS, 82 NCS) with age ranges from 8 to 21 years. The data show a statistically significant decrease in slope and BEI in patients with POTS and NCS during the head-up phase, with an increase in activity in the lag 1 and 2 portions of all phases in patients with POTS. This study provides terminology to describe baroreceptor function and identifies the slope and BEI portions of the baroreceptor reflex as the most useful objective measures to differentiate pediatric patients with POTS and NCS from normal subjects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The arterial baroreceptor reflex is a vital intrinsic mechanism for controlling both acute and chronic changes in blood pressure. [1, 2] Dysfunction of this reflex and the resulting inability to maintain vascular homeostasis can result in body system malfunction, most commonly involving cerebral perfusion [3, 4]. Two of the most common clinical manifestations are postural orthostatic tachycardia syndrome (POTS) and neurocardiogenic syncope (NCS) [5, 6]. Although the pathophysiology of these disorders is likely heterogeneous, dysfunction of the baroreceptor reflex has been implicated as the underlying cause for a significant portion of those patients [7, 8]. In conditions, such as POTS or NCS, it is theorized that this reflex fails to act properly or acts in an uncoordinated fashion and manifesting clinically as symptoms of tachycardia or syncope [9].
Changes in arterial baroreceptor function and activity in different body positions and physiologic states have been described in the adult and to a lesser extent the pediatric populations [8, 10,11,12,13,14,15,16,17]. However, the published literature to date has provided mixed results regarding the impact of arterial baroreceptors on these conditions, likely due to a combination of small sample size and/or variation in study design [1, 8, 9, 18,19,20]. Additionally, a clear terminology to describe baroreceptors is needed given the variation in the ways baroreceptors have been defined in the published literature [1, 8,9,10,11,12,13,14,15, 17,18,19,20], resulting in difficulty to standardize and compare research findings. The aim of this study is to provide a concise definition of the overall function of the arterial baroreceptors, which we are designating the baroreceptor reflex response (BRR), characterized by: a. baroreceptor activity, b. baroreceptor effectiveness index (BEI), and c. baroreceptor sensitivity and to use the HUTT to assess the BRR in pediatric patients with POTS and NCS as compared to a normal cohort.
Methods
Tilt Protocol
The HUTT was performed according to a 3-phase protocol involving a pre-tilt period (phase 1) consisting of a 10-min supine period, followed by the head-up period (phase 2) where the subject underwent an upright head-up tilt to 65–70° for 30 min, followed by a post-tilt period (phase 3) consisting of another 10 min of recording in the supine position. In patients that experienced syncope, phase 2 of the tilt protocol was terminated prior to the 30-min mark and went on to complete the 10-min phase 3. We chose the median period recommended by the European Society of cardiology (minimum 20 min and maximum of 45 min) and the previous reported protocol for pediatric patients by Robinson et al. [21, 22].
Vital signs were recorded and logged using the Task Force Monitor by CNSystems® (Graz, Austria) and consisted of a continuous 12 lead electrocardiogram, continuous heart rate monitor, and non-invasive continuous finger blood pressure measurements standardized with a biceps cuff pressure measurement every minute for accuracy. All phases of the HUTT procedure were monitored by a physician to ensure proper recording of goal measurements and manually validated at time of testing. All individuals were fasted at least 3 h prior to start of the HUTT procedure.
Population Selection
The study prospectively enrolled a normal subject group [16] that was then compared to patients with POTS and NCS based on prospective enrollment and retrospective review of cataloged HUTT data obtained from the Task Force machine at the Children’s Memorial Hermann Hospital in Houston, TX between 2011 and 2018. Subjects were referred for HUTT based on history of symptoms and were subsequently diagnosed with POTS or NCS based on criteria described below. Patients with incomplete data, or other diagnosed neurologic or cardiac diseases, or on any prescription medications were excluded from the study. Consent was obtained from the individuals and/or parents and the study was approved by The University of Texas Health Science Center at Houston Institutional Review Board.
Subject Classification
POTS in a pediatric patient was defined as an increase of 40 beats/min during the first 10 min of standing and without associated hypotension [23, 24]. NCS was defined as a syncope syndrome that usually (1) occurs with upright posture held for more than 30 s or with exposure to emotional stress, pain, or medical settings; (2) features diaphoresis, warmth, nausea, and pallor; (3) is associated with hypotension and relative bradycardia, when known; and (4) is followed by fatigue [25,26,27].
BRR Measurements
The sequence method was used to identify and tabulate three goal measurements. The first measurement was the arterial baroreceptor activity, measured as number of baroreceptor events per minute. A baroreceptor event was defined as a change in blood pressure greater than 1 mmHg per heart beat spanning over at least three heart beats, with an associated change in heart rate defined as a change in the R–R intervals greater than or equal to 4 ms. (Fig. 1) In addition, the lag associated with the change in systolic pressure and heart rate was also measured and defined as Lag 0 where the changes in the R–R interval and blood pressure were synchronized, Lag 1 where the change in heart rate was delayed by one R–R interval from the change in blood pressure, and Lag 2 where the change in heart rate was delayed by two R–R intervals. (Fig. 2).
The second goal measurement was the baroreceptor effectiveness index (BEI) and was calculated as the ratio of events that occurred divided by the total number of blood pressure changes that took place, including those instances with no associated heart rate change.
The third goal measurement was baroreceptor sensitivity (BRS), where the slope of the regression line between the R–R intervals and blood pressures was calculated for each event and reported as msec/mm Hg. The sensitivity was further defined as an “up-event” where the blood pressure and R–R interval were increasing, a “down-event” where the blood pressure and R–R interval were decreasing and a “net” value which offered a congregate mean of all the up and down events (Table 1).
Statistics
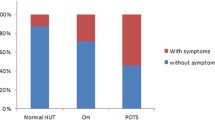
Descriptive statistics (mean, standard deviation, etc.) and bar charts were provided for each lag at each phase of events per minute, BEI, and slope in normal, POTS, and NCS groups (Tables 2, 3 and 4; Figs. 3, 4, and 5). A generalized linear mixed model with empirical estimators was used to model outcomes on group, phase and/or lag, and their interactions, while accounting for the within-subject correlation robustly [28]. P values for pairwise comparisons among normal, POTS, and NCS groups at each lag and phase were adjusted by the Tukey method for multiple comparisons and significance set at P value < 0.05. All data analyses were performed in SAS 9.4 (Cary, NC).
Baroreceptor activity—figure depicts the mean values for the activity of the baroreceptors during the three phases of the HUTT. The cross (+) indicates a statistically significant difference between the patient and normal subject groups. The asterisk (*) indicates a statistically significant difference between the patient groups. Lag 0, 1, and 2 depicted by the (0, 1, 2) designations below the bar graphs
Results
Of the individuals analyzed during the study time period, all met study criteria and were enrolled, 49 were normal subjects, 67 patients had POTS, and 82 patients had NCS. There was no statistically significant difference between the median age and weight of the three groups. The patients and normal subjects’ measured heart rate, blood pressure, and BMI were noted between the 10th and 90th percentile for their age.
POTS
In the 67 patients enrolled in the POTS group, the average maximum heart rate was 151 ± 30 BPM. As shown in Fig. 3, in comparison to the normal subject group, there was a significant increase in the baroreceptor activity in the lag 1 and 2 portions of the phase 1, a significant decrease in lag 0 and a significant increase in lag 2 portion of the head-up phase 2, and a significant increase in lag 1 portion of phase 3. In regards to BEI, there was a significant decrease in the patients with POTS during the head-up phase 2, but no statistically significant difference during the other phases, as shown in Fig. 4. In regards to baroreceptor sensitivity, as shown in Fig. 5 there was a significant decrease in the patients with POTS during the head-up phase 2, but no statistically significant difference during the other phases.
Baroreceptor sensitivity—figure depicts the mean values for the sensitivity of the baroreceptors during the three phases of the head-up tilt table test, as measured by the slope of the baroreceptor reflex. The cross (+) indicates a statistically significant difference in comparison between the patient and normal subject groups. Net slope, slope up, and slope down, depicted by (N, U, D), respectively, below the bar graph
NCS
In the 82 patients enrolled in the NCS group, the average time to syncope was 12.1 ± 5.3 min. As shown in Fig. 3, in comparison to the normal subject group, there was no statistically significant difference in the arterial baroreceptor activity between normal subjects and patients with NCS, aside from the lag 0 portion of the post-tilt phase 3, where the patients with NCS had significantly lower activity. The time of phase 2 varied due to a varied response of time to syncope for these patients. When the time to syncope was analyzed in respect to the number of events of lag 0 in phase 3, it was found that a longer time to syncope correlated to more lag 0 events in phase 3 with a correlation of 0.56515 and a p value of < 0.0001, which was statistically significant. In regards to BEI, as shown in Fig. 4 there was a significant decrease in the patients with NCS during the head-up phase 2, but no statistically significant difference during the other phases. In regards to arterial baroreceptor sensitivity, as shown in Fig. 5 there was a significant decrease in sensitivity during the head-up phase 2, but no statistically significant difference during the other phases. When analyzing the slope up versus down, there was no change in statistical significance between the patients with NCS and normal subjects.
POTS Versus NCS
In comparing the POTS and NCS groups, there was a statistically significant difference when comparing the arterial baroreceptor activity in the post-tilt phase 3, with increased activity noted in patients with NCS except in lag 2 where there was a decrease in activity. All lag measurements show a significantly lower activity in the patients with NCS in comparison to POTS. The remaining measurements did not have a statistically significant difference between POTS and NCS. (Tables 2, 3, and 4).
Discussion
The arterial baroreceptor is an intricate reflex loop that involves efficiency of activation, sensitivity, and an effectiveness index; moreover, a description of each component is necessary to fully define this reflex. Therefore, we propose designating the new term, the baroreceptor reflex response (BRR), consisting of a measure of the baroreceptor activity, sensitivity, and effectiveness index. This new descriptor provides a more complete depiction of the different qualities of the arterial baroreceptor and allows for a more directed investigation into the overall performance of the arterial baroreceptor. This study aims to describe the arterial baroreceptor physiology in a pediatric population with autonomic dysfunction as compared to a normal subject cohort and to establish a new terminology to more thoroughly characterize the components of the baroreceptor to better standardize the findings between studies.
Postural orthostatic tachycardia syndrome is suspected to affect 0.2% of the general population [23], while NCS affects up to 25% of the general pediatric population [26] causing injury on presentation in up to 18% of pediatric patients [29]. With the development of the head-up tilt test (HUTT) as a verified method to assess arterial baroreceptor function and activity [2, 30, 31], it has become feasible to investigate these autonomic conditions without the need for an invasive procedure. In addition, the sequence method avoids pharmacological manipulation of the subjects’ receptors that can potentially alter baseline arterial baroreceptor physiology [12, 32, 33]. The sequence method also makes it possible to monitor beat-to-beat changes in heart rate and blood pressure to directly pinpoint any deviations or delays from the expected reflex pathway [33, 34]. The coordination of measurements of heart rate and blood pressure allows for assessment of the lag of arterial baroreceptor activation, in addition to the assessment of sensitivity and baroreceptor effectiveness index (BEI) [34,35,36,37]. In our recently published study, we described the arterial baroreceptor characteristics in normal pediatric subjects using the HUTT and sequence method, showing that under normal conditions, the arterial baroreceptor activity increased during the head-up phase, while the sensitivity decreased [16].
On evaluation of arterial baroreceptor activity, the higher dependence on the lag 1 and lag 2 portions of the baroreceptor reflex seen in the patients with POTS indicates an overall slower response of the arterial baroreceptors as compared to normal subjects. In contrast, patients with NCS had a difference in activity only during the lag 0 portion of the phase 3, but otherwise there were no other statistically significant differences when compared to the normal subjects. This small difference found in lag 0 of phase 3 could indicate a possible reset of the arterial baroreceptor reflex post-syncope, hence the lower activity; otherwise, the phase 1, phase 2, and phase 3 lag 1 and lag 2 activity in patients with NCS are similar to that of the normal subject cohort. However, patients who had a longer time to syncope in phase 2 had more lag 0 events in phase 3 which could suggest a more coordinated and functioning baroreceptor reflex response in those patients who were able to sustain a head-up tilt longer during phase 2. When comparing POTS versus NCS groups, there is a significantly lower activity during all lag measurements in the post-tilt phase 3, but otherwise no statistically significant difference was found. This difference in phase 3 between the patient groups could be due to the patients with NCS entering phase 3 directly following a syncopal episode and their arterial baroreceptors functioning at a lower level than expected and therefore unable to recover fully. The only statistically significant difference noted in patients with NCS as compared to normal subjects was during the lag 0 portion of phase 3, which again could be due to the syncopal episode. Nevertheless, it appears that arterial baroreceptor activity plays a larger role in the pathophysiology of POTS with a higher dependence on the delayed lag 1 and lags 2 responses, which is not seen in the patients with NCS. Investigation into the lag portions of the arterial baroreceptor reflex has not been performed in these patient groups previously and this novel data provide a better understanding of the underlying physiology of the arterial baroreceptor function.
On evaluation of BEI, patients with POTS and NCS had significantly lower values compared to the normal subjects during the head-up portion of the study. This finding is in contrast to a previous study in adults with NCS [8]. The lower BEI suggests that there was a larger amount of blood pressure changes that were not transmitted via the arterial baroreceptors and did not result in heart rate changes. We hypothesize that the decrease in BEI seen in both POTS and NCS can be due to a saturation phenomenon where the arterial baroreceptors can only transmit stimuli in a limited frequency. In patients who require more adjustments for their blood pressure, the arterial baroreceptors will continue to be stimulated, but are perhaps refractory for a period of time and cannot respond directly to the consecutive stimuli. Therefore, the arterial baroreceptors end up responding to a lower proportion of the total stimuli and thus resulting in a lower BEI.
A possible reason for the increased stimuli in patients with NCS or POTS can be explained by investigation into baroreceptor sensitivity. Our data show that patients with POTS or NCS had a significantly lower value compared to the normal subjects during the head-up portion of the study. When subdividing the net slope into slope up or down, the data remain statistically significant indicating that for both an increase and decrease in blood pressure, the arterial baroreceptor reflex in patients with POTS and NCS is less robust in the attempt to adjust for blood pressure difference. There was no statistically significant difference found when comparing POTS versus NCS groups. The decreased sensitivity is also consistent with the clinical presentation of patients with POTS or NCS and their inability to properly compensate for postural stresses that induce a blood pressure change and result in symptoms of tachycardia or syncope. The less robust heart rate adjustment can potentially be insufficient to reach the goal cardiac output and a subsequent stimulus is required in the body’s continued attempts to re-stimulate the arterial baroreceptor until the goal cardiac output is reached [9, 38]. This would in turn result in a higher measured baroreceptor activity or lower measured BEI, as seen in our data.
The BRS findings in our study are in contrast to the previously reported higher BRS values in pediatric and adult patients with POTS [39] and NCS [8]. In our study, we found no significant difference in BRS during phase 1 between the normal subjects, POTS, and NCS, but did show a significant difference during phase 2. In both of the above-mentioned studies, BRS was measured at rest in contrast to our study which evaluated BRS in phase 2 as well. Additionally, in the second study above, there was a broader age range of both adolescents and adults [8]. Differences between children, adolescents, and adults in the BRS and HR have been noted [40]; moreover, different cardiac responses have been noted in POTS patients [41]. Additional studies with tighter delineated age groups and using the sequence method and evaluating patients in specific phases, measuring lags, may be warranted in the future to further clarify these differences; however, the lower BRS found in our study in phase 2 appears to be more consistent with the clinical presentation and other baroreceptor characteristics of patients with these conditions.
The findings measured in our study may explain the manifestations of the symptoms in the two conditions studied. For the POTS group, the higher dependence on the lag 1 and lag 2 portions of the baroreceptor reflex could indicate an uncoordinated or delayed response to the stimuli. Multiple pathophysiological mechanisms have been proposed as the cause for the symptoms associated with POTS, including impaired sympathetic vasoconstriction, excessive cardiac sympathoexcitatory responses, volume dysregulation, and physical deconditioning [5]. The less robust baroreceptor sensitivity in addition to the delayed and perhaps lingering response resulting in tachycardia symptoms is consistent with the theory of impaired sympathetic response and volume dysregulation in patients with POTS [38]. For patients with NCS, the underlying cause of their disease involves a lack of coordinated cardiac reflex response to a decrease in blood pressure resulting in a decrease in cerebral perfusion and subsequent brief loss of consciousness until re-establishment of homeostasis and rapid recovery [34, 42]. A less robust arterial baroreceptor response that results in an inadequate heart rate response can be the reason for the patients exhibiting fainting due to inadequate brain perfusion. The higher number of lag 0 events in phase 3 in NCS patients with a longer time to syncope would suggest variability in ability to mount a coordinated cardiovascular response to orthostatic stress in such patients. In addition, the higher dependence of the patients with POTS on the delayed lag 1 and lag 2 portions of the baroreceptor reflex could also potentially indicate a similar delayed response in the NCS patients, but to a larger degree that would require measuring lag 3 or lag 4 to uncover the effects. Further study into the lag subdivision of the arterial baroreceptor reflex can clarify this theory.
Conclusion
This study identifies key differences and provides more understanding of arterial baroreceptor reflex components, the baroreceptor activity, BEI, and sensitivity in pediatric patients with POTS and NCS. Our data show that slope and BEI appear to be the main factors that change in pediatric patients with POTS and NCS. We also provide new data regarding delayed heart rate responses to pressure changes in the Lag 1 and Lag 2 values found to be statistically significant in the patients with POTS. These findings indicate that these patients deviate from normal subjects in regards to their arterial baroreceptor physiology as made evident by the stressor of the head-up position. This new data regarding the difference in arterial baroreceptor function of patients with autonomic disorders further highlight the impact of this reflex on the symptoms and manifestation of these disorders and may provide a potential new avenue for therapies. A longitudinal study of the arterial baroreceptor response to therapies and the resulting changes in symptoms would delineate the effect of the baroreceptor reflex on these patients and is an opportunity for further study. Finally, our study also defines a new term, the baroreceptor reflex response (BRR), to more clearly describe the different characteristics of the baroreceptor reflex and to provide a framework for more consistent and complete investigation of this physiologic response to stress.
Limitations
A limitation of this study was the inability to enroll infants and toddlers due to difficulty with compliance with the HUTT and thus a portion of the pediatric population was unstudied. Additionally, this study did not specifically address sex differences in relation to POTS or NCS. Orthostatic intolerance is more common in females compared to males. This may be due to differences in stroke volume, cardiac size, and the effects of estrogen on the central autonomic nuclei; however, the sample size was not large enough to adequately compare sex differences in this study. Also, this study represents the findings at one academic institution. Although our institution encompasses a large and diverse patient population, our experience may differ from other institutions and further investigation and correlation will be beneficial.
Abbreviations
- HUTT:
-
Head-up tilt test
- POTS:
-
Postural orthostatic tachycardia syndrome
- NCS:
-
Neurocardiogenic syncope
- BRR:
-
Baroreceptor reflex response
- BEI:
-
Baroreceptor effectiveness index
References
Dietrich A, Riese H, Van Roon AM et al (2006) Spontaneous baroreflex sensitivity in (pre)adolescents. J Hypertens 24:345–352. https://doi.org/10.1097/01.hjh.0000200517.27356.47
Parati G, Di Rienzo M, Mancia G (2001) Dynamic modulation of baroreflex sensitivity in health and disease. Ann N Y Acad Sci 940:469–487. https://doi.org/10.1111/j.1749-6632.2001.tb03699.x
Lankford J, Numan M, Hashmi SS et al (2015) Cerebral blood flow during HUTT in young patients with orthostatic intolerance. Clin Auton Res 25:277–284. https://doi.org/10.1007/s10286-015-0295-9
Mitro P, Simurda M, Evin L et al (2015) Reduced baroreflex sensitivity in patients with vasovagal syncope. Bratisl Med J 116:582–586. https://doi.org/10.4149/BLL
Benarroch EE (2012) Postural tachycardia syndrome: a heterogeneous and multifactorial disorder. Mayo Clin Proc 87:1214–1225. https://doi.org/10.1016/j.mayocp.2012.08.013
McLeod KA (2003) Syncope in childhood. Arch Dis Child 88:350–353. https://doi.org/10.1136/adc.88.4.350
Garland E, Celedonio J, Raj S (2015) Postural tachycardia syndrome: beyond orthostatic intolerance. Curr Neurol Neurosci Rep. https://doi.org/10.1007/s11910-015-0583-8
Pitzalis M, Parati G, Massari F et al (2003) Enhanced reflex response to baroreceptor deactivation in subjects with tilt-induced syncope. J Am Coll Cardiol 41:1167–1173. https://doi.org/10.1016/S0735-1097(03)00050-0
Samniah N, Sakaguchi S, Ermis C et al (2004) Transient modification of baroreceptor response during tilt-induced vasovagal syncope. Europace 6:48–54. https://doi.org/10.1016/j.eupc.2003.09.004
Zavodna E, Honzikova N, Hrstkova H et al (2006) Can we detect the development of baroreflex sensitivity in humans between 11 and 20 years of age? Can J Physiol Pharmacol 84:1275–1283. https://doi.org/10.1139/Y06-060
Tanaka H, Thulesius O, Borres M et al (1994) Blood pressure responses in Japanese and Swedish children in the supine and standing position. Eur Heart J 15:1011–1019
Rüdiger H, Bald M (2001) Spontaneous baroreflex sensitivity in children and young adults calculated in the time and frequency domain. Auton Neurosci Basic Clin 93:71–78. https://doi.org/10.1016/S1566-0702(01)00326-5
Papaioannou VE (2007) Heart rate variability, baroreflex function and heart rate turbulence: possible origin and implications. Hell J Cardiol 48:278–289
Nováková Z, Honzíková N, Závodná E et al (2001) Baroreflex sensitivity and body growth parameters in children and adolescents. Exp Clin Cardiol 6:35–37
Difrancesco MW, Shamsuzzaman A, McConnell KB et al (2018) Age-related changes in baroreflex sensitivity and cardiac autonomic tone in children mirrored by regional brain gray matter volume trajectories. Pediatr Res 83:498–505. https://doi.org/10.1038/pr.2017.273
Alnoor MS, Varner HK, Butler IJ et al (2019) Baroreceptor activity and sensitivity: normal values in children and young adults using the head up tilt test. Pediatr Res 85:841–847. https://doi.org/10.1038/s41390-019-0327-6
Li H, Liao Y, Han Z et al (2018) Head-up tilt test provokes dynamic alterations in total peripheral resistance and cardiac output in children with vasovagal syncope. Acta Paediatr Int J Paediatr 107:1786–1791. https://doi.org/10.1111/apa.14342
Honzíková N, Závodná E (2016) Baroreflex sensitivity in children and adolescents: physiology, hypertension, obesity, diabetes mellitus. Physiol Res 65:879–889
Iacoviello M, Forleo C, Guida P et al (2010) Independent role of reduced arterial baroreflex sensitivity during head-up tilt testing in predicting vasovagal syncope recurrence. Europace 12:1149–1155. https://doi.org/10.1093/europace/euq149
Klemenc M, Štrumbelj E (2015) Predicting the outcome of head-up tilt test using heart rate variability and baroreflex sensitivity parameters in patients with vasovagal syncope. Clin Auton Res 25:391–398. https://doi.org/10.1007/s10286-015-0318-6
Robinson JA, Shivapour JK, Snyder CS (2017) Tilt table testing to diagnose pseudosyncope in the pediatric population. Congenit Heart Dis 12:411–416. https://doi.org/10.1111/chd.12458
Moya A, Sutton R, Ammirati F et al (2009) Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 30:2631–2671. https://doi.org/10.1093/eurheartj/ehp298
Bryarly M, Phillips LT, Fu Q et al (2019) Postural orthostatic tachycardia syndrome: JACC focus seminar. J Am Coll Cardiol 73:1207–1228. https://doi.org/10.1016/j.jacc.2018.11.059
Freeman R, Wieling W, Axelrod FB et al (2011) Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res 21:69–72. https://doi.org/10.1007/s10286-011-0119-5
Swenne CA (2013) Baroreflex sensitivity: mechanisms and measurement. Neth Hear J 21:58–60. https://doi.org/10.1007/s12471-012-0346-y
Singhi P, Saini AG (2018) Syncope in pediatric practice. Indian J Pediatr 85:636–640. https://doi.org/10.1007/s12098-017-2488-9
Alboni P (2015) The different clinical presentations of vasovagal syncope. Heart 101:674–678. https://doi.org/10.1136/heartjnl-2014-307096
Hedeker (2008) Longitudinal data analysis. Longit Data Anal. https://doi.org/10.4324/9780203929483-16
Driscoll DJ, Jacobsen SJ, Porter CBJ, Wollan PC (1997) Syncope in children and adolescents. J Am Coll Cardiol 29:1039–1045. https://doi.org/10.1016/S0735-1097(97)00020-X
Allen MT, Matthews KA, Kenyon KL (2000) The relationships of resting baroreflex sensitivity, heart rate variability and measures of impulse control in children and adolescents. Int J Psychophysiol 37:185–194. https://doi.org/10.1016/S0167-8760(00)00089-1
Teodorovich N, Swissa M (2016) Tilt table test today—state of the art. World J Cardiol 8:277. https://doi.org/10.4330/wjc.v8.i3.277
Laude D, Elghozi JL, Girard A et al (2004) Comparison of various techniques used to estimate spontaneous baroreflex sensitivity (the EuroBaVar study). Am J Physiol 286:226–231. https://doi.org/10.1152/ajpregu.00709.2002
Parati G, DiRienzo M, Mancia G (2000) How to measure baroreflex sensitivity: from the cardiovascular laboratory to daily life. J Hypertens 18:7–19. https://doi.org/10.1097/00004872-200018010-00003
La Rovere MT, Pinna GD, Raczak G (2008) Baroreflex sensitivity: measurement and clinical implications. Ann Noninvasive Electrocardiol 13:191–207. https://doi.org/10.1111/j.1542-474X.2008.00219.x
Malik M (1996) Guidelines heart rate variability. Eur Heart J 17:354–381. https://doi.org/10.1161/01.CIR.93.5.1043
Pellizzer AM, Kamen PW, Jackman G et al (1996) Non-invasive assessment of baroreflex sensitivity and relation to measures of heart rate variability in man. Clin Exp Pharmacol Physiol 23:621–624. https://doi.org/10.1111/j.1440-1681.1996.tb02800.x
Takahashi N, Nakagawa M, Saikawa T et al (1999) Noninvasive assessment of the cardiac baroreflex: response to downward tilting and comparison with the phenylephrine method. J Am Coll Cardiol 34:211–215. https://doi.org/10.1016/S0735-1097(99)00158-8
Furlan R, Jacob G, Snell M et al (1998) Chronic orthostatic intolerance: a disorder with discordant cardiac and vascular sympathetic control. Circulation 98:2154–2159. https://doi.org/10.1161/01.CIR.98.20.2154
Li H, Liao Y, Wang Y et al (2016) Baroreflex sensitivity predicts short-term outcome of postural tachycardia syndrome in children. PLoS ONE 11:1–12. https://doi.org/10.1371/journal.pone.0167525
Fu Q, VanGundy T, Galbreath M et al (2010) Cardiac origins of the postural orthostatic tachycardia. J Am Coll Cardiol 55:2858–2868. https://doi.org/10.1016/j.jacc.2010.02.043.Cardiac
Pianosi PT, Schroeder DR, Fischer PR (2016) Cardiac responses to exercise distinguish postural orthostatic tachycardia syndrome variants. Physiol Rep 4:1–8
Kanjwal K, Calkins H (2015) Syncope in children and adolescents. Cardiol Clin 33:397–409. https://doi.org/10.1016/j.ccl.2015.04.008
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alnoor, M.S., Varner, H.K., Butler, I.J. et al. Arterial Baroreceptor Physiology: Differences Between Normal Subjects and Pediatric Patients with Postural Tachycardia and Neurocardiogenic Syncope. Pediatr Cardiol 43, 1011–1019 (2022). https://doi.org/10.1007/s00246-022-02815-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02815-1