Abstract
Neurodevelopmental (ND) impairment is common in children with congenital heart disease (CHD). While routine ND surveillance and evaluation of high-risk patients has become the standard-of-care, capture rate, barriers to referral, and potential patient benefits remain incompletely understood. Electronic data warehouse records from a single center were reviewed to identify all eligible and evaluated patients between July 2015 and December 2017 based on current guidelines for ND screening in CHD. Diagnoses, referring provider, and payor were considered. Potential benefit of the evaluation was defined as receipt of new diagnosis, referral for additional evaluation, or referral for a new service. Contingencies were assessed with Fisher’s exact test. In this retrospective, cohort study, of 3434 children identified as eligible for ND evaluation, 135 were evaluated (4%). Appropriate evaluation was affected by diagnostic bias against coarctation of the aorta (CoArc) and favoring hypoplastic left heart syndrome (HLHS) (1.8 vs. 11.9%, p<0.01). Referrals were disproportionally made by a select group of cardiologists, and the rate of ND appointment non-compliance was higher in self-pay compared to insured patients (78% vs 27%, p<0.01). Potential benefit rate was 70–80% amongst individuals with the three most common diagnoses requiring neonatal surgery (CoArc, transposition of the great arteries, and HLHS). Appropriate ND evaluation in CHD is impacted by diagnosis, provider, and insurance status. Potential benefit of ND evaluation is high regardless of diagnosis. Strategies to improve access to ND evaluations and provider understanding of the at-risk population will likely improve longitudinal ND surveillance and clinical benefit.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital heart disease (CHD) is the most common birth defect with an annual incidence of 1 in 100 live births in the USA [1]. Nearly one-third of these patients have critical congenital heart disease (CCHD) and require early surgical intervention during the first year of life [1]. Survival of infants with CHD into adolescence and adulthood continues to improve with constant refinement of diagnostic modalities, surgical techniques, and advances in medical management. Increased survival has highlighted the consequence of CHD and its related interventions on the long-term ND morbidity in these patients.
For children with CHD, ND impairments are not as severe as they are prevalent [2]. The etiology of ND delays in CHD is multifactorial. Despite a growing understanding of the risk factors for delay, these deficits have persisted over time [3]. Delays vary from early gross motor and language delays and visual-spatial deficits to executive functioning and social cognition [4]. There is also significant intra- and inter- patient variations that are dynamic over the lifetime of these children [5]. ND delays have immediate and longitudinal implications on a child’s academic performance and their overall quality of life.
The positive impact of early and systematic ND evaluation and intervention has been demonstrated in premature infants [6]. The similarities in brain immaturity and insults in early life between premature infants and those with CHD would suggest that a similar model of early evaluation and intervention would provide developmental benefit for children with CHD. In 2012, the American Heart Association (AHA) and the American Academy of Pediatrics (AAP) created specific guidelines targeting children with CHD at the highest risk for ND delays. These guidelines recommended surveillance, screening, periodic evaluation, reevaluation, and management of ND deficits in children with CHD [7]. Nationally, longitudinal ND follow-up programs have been created in most large cardiac surgical centers. These programs are challenged by center-level variability in timing of evaluations and clinical structure. Additionally, capture rates across centers are unknown and there are little data describing the short-term patient benefits associated with these programs after the implementation of the AHA guidelines.
Practical benefit to any heart center’s patient population is dependent on equitable distribution of care. Barriers to care are likely related to socio-demographic factors, access to developmental evaluations, parental understanding of the risks of developmental delay, and practitioner awareness of AHA screening guidelines. In an effort to optimize referrals and evaluations in our Heart Center ND Program (HCNP), this retrospective, cohort study aimed to describe the local capture rate, referral patterns, and potential patient benefits associated with ND evaluations for high-risk children with CCHD.
Materials and Methods
Study Design and Patient Population
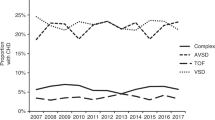
This retrospective cohort study describes children with CCHD who underwent ND evaluation at Utah’s HCNP outpatient program between July 2015 and December 2017 and all individuals were identified as eligible to undergo an evaluation during the same timeframe. The evaluated cohort was identified through electronic medical record (EMR) review of HCNP clinical encounters. The eligible cohort was identified by querying the local surgical database to identify patients operated on at Primary Children’s Hospital (PCH) who met local programmatic inclusion criteria. The EMR search criteria included a procedural code including a surgical procedure with cardiopulmonary bypass at age less than 12 months, and/or a diagnostic code for the following anatomic diagnoses: Tetralogy of Fallot with or without pulmonary atresia, d- transposition of the great arteries (TGA), tricuspid atresia, total anomalous pulmonary venous return (TAPVR), hypoplastic left heart syndrome (HLHS), double inlet left ventricle, atrioventricular septal defect, double outlet right ventricle, truncus arteriosus, coarctation of the aorta (CoArc), and interrupted aortic arch (IAA). The eligible cohort was filtered to identify ages that corresponded with the HCNP standard evaluation ages during the study period (12 to 24 months, 4–6 years, 8–14 years). Because the retrospective screening approach did not include all potential indications for referral, the evaluated and eligible cohorts were cross referenced and individuals in the evaluated cohort that were not identified in the eligible cohort were excluded from comparative analyses. The study was approved by the University of Utah (UU) Institutional Review Board (IRB_00099252) and was exempted from patient and parental consent. This study was part of a larger quality improvement effort and endpoints were selected from a key driver diagram created to identify primary and secondary drivers of appropriate referrals for ND evaluations of high-risk CHD patients.
Center-Specific Practice
Based on the AHA/AAP ND screening guidelines, the UU and the Heart Center at Primary Children's Hospital (PCH) created the HCNP in July 2015. The HCNP oversees activities in both inpatient and outpatient settings. The outpatient HCNP targets children with high-risk conditions including cyanotic heart disease, CHD requiring surgery as a newborn (< 30 days), CHD combined with other risk factors (prematurity, extracorporeal membrane oxygenation, genetic syndrome, neurologic injury, heart transplant, and history of cardiac arrest), or CHD with significant provider concern for ND delay. Patients receive a ND screening and evaluation at 12–24 months, 4–6 years, and 8–14 years of age. The outpatient clinic is embedded in the University Developmental Assessment Clinics, overseen by the Division of General Pediatrics. Providers include a developmental pediatrician, pediatric psychologist, speech, occupational and physical therapists, and a pediatric cardiologist. Referrals are accepted from primary care providers, cardiologists, and self-referrals. The HCNP clinic billing structure is aligned with institutional practice for developmental evaluation. The clinic accepts public and private insurance and self-pay patients. It does not balance bill guarantors for any financial obligation. In late 2015, primary neonatal referrals were protocolized and made at the time of discharge from all hospitalizations that included neonatal CHD surgery. A prospective clinical and ND database was created including eligible neonates and evaluated patients.
Measurements
Payor and Referring Provider
Insurance data and referring provider were collected from the electronic medical record (EPIC, Epic Systems Corporation, Verona, Wi). Insurance coverage was categorized as commercial (private), Medicaid, or self-pay. Referring providers were identified by the physician listed in the initial clinical referral shell in EPIC. In instances where the HCNP director was listed due to an automatic referral at the time of discharge from the hospital, the patient’s primary cardiologist was selected as the referring provider.
Potential Clinical Benefit
Given the lack of published, standardized definitions of clinical benefit associated with ND screening and evaluation in children with CHD, local stakeholders, including quality improvement experts and the HCNP clinical team, created a working definition of clinical benefit. Potential clinical benefit was divided into three categories: new behavioral or psychosocial diagnosis, referral for additional testing used to better define the identified delays on screening, and referral for new therapy, such as behavioral or mental health therapies. For individuals with the three most common diagnoses requiring a neonatal surgical intervention, the occurrence of a new diagnosis, testing, or service following a visit was determined by chart review (JJW, JM, TAM) and adjudicated by a single member of the research team for consistency (TAM).
Statistical Analysis
Descriptive statistics were calculated as counts and percentages. Diagnostic groups, payor, and benefit variables were compared using Fisher’s exact test. Significance was determined at p < 0.05. Statistical analyses were performed with Prism 8 software (Graph Pad Software, Inc, San Diego, CA).
Results
Patient Population and CHD Diagnoses
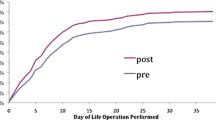
Between July 2015 and December 2017, 148 patients underwent formal ND evaluation at the UU HCNP clinic. There were 3434 patients identified as eligible for ND evaluation during that same period. Thirteen individuals were evaluated but not identified in the eligible cohort. Reasons for not being identified by the methods described to determine eligibility included the following: minor heart disease not requiring surgery in the first year of life (n = 6), arrhythmia (n = 3), cardiomyopathy (n = 2), and surgery performed at an outside center or prior to capture in the surgical database (n = 2). Demographics and diagnoses for the evaluated and eligible cohorts are shown in Table 1. The capture rate of evaluated/eligible was 4%. CoArc, TGA, and HLHS represented 45% of the evaluated and 50% of the eligible patient cohort. Of the three most common diagnoses requiring neonatal surgery, capture rate for evaluated patients demonstrated a significant diagnostic bias against CoArc and HLHS (p < 0.01), while the proportion of individuals with TGA was similar in the evaluated and eligible cohorts (Figure 1).
Referring Provider and Payor
Twenty-seven pediatric cardiologists from the University of Utah were the sole source of patient referrals for ND evaluation. There were no referrals from primary care physicians or family/self- referrals. Five cardiologists referred 48% of the evaluated cohort (Figure 2). A minority of patients were evaluated without health insurance (1%), and the majority were covered with private insurance (69%). Appointment non-compliance (no-show or < 24 h notice of cancelation) occurred in 30% of the patients who were referred for evaluation. No-show and late cancelation rate based on payor is shown in Figure 3. There was a higher appointment non-compliance rate in self-pay patients versus insured patients (p < 0.01).
Potential Clinical Benefit
Across the three most common diagnoses (CoArc, TGA, and HLHS), potential benefit of the evaluation was high. Greater than 70% of the evaluated patients received at least one benefit as a result of their ND screening visit, and 13% received all three defined benefits (Figure 4b). Patients with HLHS were less likely to receive a new cognitive or behavioral diagnosis (9%) compared to patients with CoArc (36%) and TGA (70%) (Figure 4a), but the potential clinical benefit was similar regardless of the diagnostic group (Figure 4b). The benefit of further testing was most commonly a referral to the UU Developmental Assessment Clinics for a comprehensive neuropsychological evaluation to better characterize ND impairment identified in the ND screening visit. New ND diagnoses varied from cognitive and language disorders to attention deficit disorder (ADHD) and autism spectrum disorder. The most common new service referrals included speech therapy and local early intervention program enrollment.
Discussion
In this single center experience, we found a low capture rate for appropriate ND evaluations for children with CHD. The capture rate was significantly affected by provider and diagnostic referral bias and appointment non-compliance related to a lack of insurance coverage. Clinical benefit of a comprehensive ND evaluation was not affected by the anatomic complexity of the patient’s CHD. To our knowledge, this is the first study to document the distribution of acute, clinical benefit for children with CHD undergoing formal, routine ND evaluation in a heart center follow-up program.
Capture Rate
The 2012 scientific statement of the AHA recommends that all high-risk children with CHD receive lifelong ND surveillance [7]. Worldwide, congenital cardiac surgical centers have created formalized programs to comply with these recommendations. Seven years after the guidelines were released, little is known about the referral patterns of these programs or the impact of these evaluations on patient outcomes. Similar to many centers, in response to the guidelines, our institution developed a follow-up program to better serve the developmental needs of our patients. We identified a large cohort of patients that met criteria for referral and evaluation. Despite our cohort assembly methods likely underestimating the number of eligible patients, our capture rate for ND follow-up was only 4%. In this study, the capture rate metric serves a surrogate for the prevalence of comprehensive developmental follow-up in this complex patient population. Despite guidelines targeted at pediatricians and pediatric cardiologists, our capture rate appears to be adversely affected by provider bias. Our results suggest that only a select few providers are aware of the AHA guidelines and the risk factors for ND delay in their patients and make referrals. This provider bias may be due to a deficit in local provider education, limited exposure to the guidelines, low awareness of available services, or clinical workflow habits. No formal studies have evaluated the compliance with the 2012 AHA guidelines in the pediatric cardiology community, but our results mirror the trend amongst general pediatric providers, where few providers are referring high-risk patients for formal screening and evaluation unless deficits are suspected. Additionally, when surveyed, only 21% of pediatricians are aware of the AHA guidelines [8], which may explain why none of the referrals came from primary care pediatricians.
The prevalence and severity of ND delay increases with the complexity of the CHD lesion and is more common in patients with CHD and an associated genetic syndrome [9]. The eligible to evaluated ratio for patients with HLHS in our study would suggest that this is the mindset of most referring providers. However, the AHA guidelines suggest that all infants who undergo early palliative or corrective surgery which includes children with milder forms of CHD (CoArc) should be referred for formal, routine ND evaluations [7]. In our cohort, patients with CoArc were one-third of the eligible patients, but only represented 13% of those evaluated. This diagnostic referral bias may have a significant effect on the long-term outcomes of these patients despite their perceived lower ND delay risk in the setting of mild CHD. Studies that have explored elementary and secondary school performance, behavioral disturbances, and later executive function difficulties in children with CHD do not suggest that these challenges are impacted by the severity of the child’s CHD lesion [10,11,12]. If this diagnostic referral bias persists or if clinicians continue to refer patients only once developmental problems arise, a number of eligible patients will miss out on timely and comprehensive ND evaluations and this may impact their long-term school and behavioral performance [13].
Clinical Benefit for Evaluated Patients
The description and distribution of clinical benefit in this study supports the concept that diagnostic and referral bias is inappropriate and has the potential to impact the long-term ND of a large proportion of children with CHD. In our patient population, patients with CoArc and TGA were more likely to receive a new behavioral or cognitive deficit diagnosis during their developmental evaluation despite the diagnostic referral bias favoring HLHS. Patients with HLHS were less likely to receive a new diagnosis, but were equally referred for more testing or referred for services based on their evaluation when compared to the patients with CoArc and TGA. We suspect that the diagnostic bias is due to the heightened awareness of the referring provider concerning structurally complex heart disease for increased risk of developmental delays or when developmental deficits are identified during their multiple hospitalizations. The same heightened awareness in outside providers may have led to a referral to services bias in HLHS prior to their evaluation in the HCNP clinic, thus decreasing the rate of new ND diagnoses in this population. Some centers see patients with CHD for developmental follow-up in the first year of life and make the primary diagnosis at that time. When these patients are evaluated sooner, CHD diagnosis does not affect the incidence of developmental abnormalities [14, 15]. At our institution, patients are seen for their first developmental evaluation at 12 to 24 months. Seeing these children at an older age may be a barrier to early diagnosis and may explain the differences in the incidence of a new ND diagnosis among CHD groups. Despite the ND diagnostic discrepancy, the potential for short- and long-term benefit is maintained across diagnoses as patients were referred for services and further evaluations at the same rate, which supports the importance of ND screening at CHD surgical centers for all high-risk children.
Children who undergo surgery for CHD are more likely to require special school services, have impaired academic performance, and have behavioral challenges throughout childhood when compared to children without CHD [10,11,12]. Without routine developmental follow-up, these deficits may go unnoticed until too late, ultimately impacting school success and patient and family quality of life. This is the first study to date that documents some clinical benefits of a routine ND evaluation in children with CHD which may improve long-term outcomes. Nearly 70% of our evaluated population received a new ND diagnosis, were referred for more testing to better characterize their impairment, or were referred for comprehensive services that they were not otherwise receiving to support their intellectual or behavioral challenges. Little data exist in the CHD literature related to this topic. However, studies of neonatal intensive care unit (NICU) graduates who are evaluated followed longitudinally and received home- and hospital-based interventions that have improved school performance and long-term ND outcomes [16]. Due to the similarities in our patient populations ( critical illness early in life, brain immaturity), one could extrapolate these benefits to the CHD population further supporting the need and benefit of routine developmental evaluations.
Barriers to ND Evaluation
As surgical morbidity and mortality improve, ND outcomes in CHD is rapidly becoming a paramount outcome measure. The 2012 AHA scientific statement is relatively new and due to varied resources and infrastructure, CHD surgical centers are undertaking diverse approaches to the development of ND follow-up programs. Diagnostic inclusion criteria, timing of evaluation, and referral methods and patterns vary, thus impacting our ability to compare capture rate, barriers to care, and benefit associated with ND evaluation. Few centers have reported specific barriers to ND follow-up in CHD, and these barriers are not consistent among studies [18,19,20]. Attention should be paid to referral methods and timing of follow-up. NICU ND follow-up clinics have existed for decades and most CHD centers have modeled their ND follow-up according to these clinical models. Barriers to ND follow-up in the NICU population is related to referral methods and timing of follow-up after hospital discharge. Removal of appointment scheduling burden on the family and increasing appointment availability improved access to ND care in NICU graduates [17]. Similar strategies may improve ND follow-up in the CHD population. Families of children with CCHD are often overwhelmed with multispecialty outpatient follow-up and are more likely to miss appointments or suffer from appointment fatigue [18]. During the course of our study, we implemented practitioner-driven appointment scheduling at neonatal hospital discharge to decrease the burden on families and expanded our clinical availability from one to two clinics per month to increase patient access to ND evaluation. The effect of these changes has not been analyzed, but likely contributed to our 70% appointment attendance rate during the study period.
Scheduled visit non-attendance represents a missed opportunity for the patient and a waste of clinic resources. Unfortunately, 30% of our referred patients did not undergo their scheduled ND evaluation. Reported rates of ND follow-up after referral in children with CHD ranges from 17–52% [18, 19] but, lack of insurance coverage or insurance type is an independent risk factor for clinic non-attendance [18, 19]. Our study did not extensively explore reasons for appointment non-attendance. In our scheduled cohort, patients without health insurance were at the highest risk of appointment non-attendance after referral. Developmental care, because of its multispecialty team approach, can be perceived as expensive, making access to care by self-pay patients more difficult. Currently, our clinic does not balance bill guarantors or self-pay patients in an effort to eliminate this barrier to care. Insurance coverage and the perceived cost of this comprehensive care should be incorporated into care models and clinical program implementation to support long-term ND benefit in high-risk children with CHD.
Limitations
This study is limited by its single center, retrospective design. Nationally, ND programs at CHD centers differ in staffing, referral patterns, and timing of evaluations which challenge the generalizability of these results. With many different models being implemented, however, it is important that sites report successes and limitations to local approaches. Our construct of perceived clinical benefit may also be considered relatively subjective and overestimated by a bias to refer patients with subjective concerns. With a paucity of the literature on this topic, we chose to define benefit as identification of a developmental deficit, referral for more testing, and referral for therapeutic services. The impact of longitudinal developmental follow-up for these patients and future studies should address uniform definitions of clinical benefit to improve generalizability of these outcomes in future research studies and clinical care.
Conclusions
Longitudinal, formal developmental screening and evaluation is recommended by the AHA and is becoming a part of the national standard-of-care in congenital cardiac surgical centers. Diagnostic and provider referral bias impact overall capture rate, highlighting a need for improved provider and family understanding of the risk of ND delays in children with CHD. Developmental evaluation requires multispecialty care, time-intensive clinic visits, and may be costly to families, surgical centers, and insurance providers. As more centers add ND services to their care plan for children with CHD, future research should focus on programmatic structure, sustainability, and generalizable outcomes related to perceived clinical benefit for patients.
References
Hoffman JI, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol 39:1890–1900
Goldberg CS et al (2014) Factors associated with neurodevelopment for children with single ventricle lesions. J Pediatr 165:490–496. https://doi.org/10.1016/j.jpeds.2014.05.019
Gaynor JW et al (2015) Neurodevelopmental outcomes after cardiac surgery in infancy. Pediatrics 135:816–825. https://doi.org/10.1542/peds.2014-3825
Ringle ML, Wernovsky G (2016) Functional, quality of life, and neurodevelopmental outcomes after congenital cardiac surgery. Semin Perinatol 40:556–570. https://doi.org/10.1053/j.semperi.2016.09.008
Mussatto KA et al (2014) Risk and prevalence of developmental delay in young children with congenital heart disease. Pediatrics 133:e570–e577. https://doi.org/10.1542/peds.2013-2309
Spittle A, Orton J, Anderson PJ, Boyd R, Doyle LW (2015) Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005495.pub4
Marino BS et al (2012) Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation 126:1143–1172. https://doi.org/10.1161/CIR.0b013e318265ee8a
Knutson S, Kelleman MS, Kochilas L (2016) Implementation of developmental screening guidelines for children with congenital heart disease. J Pediatr 176:135–141.e132. https://doi.org/10.1016/j.jpeds.2016.05.029
Mahle WT, Wernovsky G (2001) Long-term developmental outcome of children with complex congenital heart disease. Clin Perinatol 28:235–247
Oster ME, Watkins S, Hill KD, Knight JH, Meyer RE (2017) Academic outcomes in children with congenital heart defects: a population-based cohort study. Circulation 10(2):e003074. https://doi.org/10.1161/circoutcomes.116.003074
Sanz JH et al (2017) Prevalence and pattern of executive dysfunction in school age children with congenital heart disease. Congenit Heart Dis 12:202–209. https://doi.org/10.1111/chd.12427
Mulkey SB et al (2016) School-age test proficiency and special education after congenital heart disease surgery in infancy. J Pediatr 178:47–54
Simon BV et al (2019) Neurodevelopmental delay following the neonatal repair of coarctation and arch obstruction. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2019.04.088
Soto CB et al (2011) Implementation of a routine developmental follow-up program for children with congenital heart disease: early results. Congenit Heart Dis 6:451–460. https://doi.org/10.1111/j.1747-0803.2011.00546.x
Mussatto KA et al (2015) Risk factors for abnormal developmental trajectories in young children with congenital heart disease. Circulation 132:755–761. https://doi.org/10.1161/circulationaha.114.014521
Spittle AJ et al (2010) Preventive care at home for very preterm infants improves infant and caregiver outcomes at 2 years. Pediatrics 126:e171–e178. https://doi.org/10.1542/peds.2009-3137
Patra K, Greene MM, Perez B, Silvestri JM (2014) Neonatal high-risk follow-up clinics: how to improve attendance in very low birthweight infants. E-J Neonatol Res 4(1):3–13
Michael M, Scharf R, Letzkus L, Vergales J (2016) Improving neurodevelopmental surveillance and follow-up in infants with congenital heart disease. Congenit Heart Dis 11:183–188. https://doi.org/10.1111/chd.12333
Loccoh EC et al (2018) Prevalence and risk factors associated with non-attendance in neurodevelomental follow-up clinic among infants with CHD. Cardiol Young 28:554–560. https://doi.org/10.1017/s1047951117002748
Chorna O et al (2016) Feasibility of a team approach to complex congenital heart defect neurodevelopmental follow-up: early experience of a combined cardiology/neonatal intensive care unit follow-up program. Circulation 9:432–440. https://doi.org/10.1161/circoutcomes.116.002614
Funding
This study was not funded by internal or external funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Due to the retrospective nature of the study, there was no direct contact with participants. The data was collected through medical chart review. Informed consent was waived and this waiver was approved by the University of Utah and Primary Children’s Hospital Institutional Review Board.
Research Involving Human and Animal Participants
This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Glotzbach, K.L., Ward, J.J., Marietta, J. et al. The Benefits and Bias in Neurodevelopmental Evaluation for Children with Congenital Heart Disease. Pediatr Cardiol 41, 327–333 (2020). https://doi.org/10.1007/s00246-019-02260-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-019-02260-7