Abstract
Because Fontan circulation does not have a subpulmonary ventricle, the preload is limited. In Fontan circulation with extracardiac conduit, the size of conduit could be an important factor in determining the preload. We compared exercise capacity with each conduit size and tried to search for optimal conduit size in Fontan circulation. We reviewed the medical record of 677 patients with Fontan circulation. Patients who had other type Fontan circulation (Kawashima, atriopulmonary, lateral tunnel), SpO2 < 85%, protein losing enteropathy, results of inappropriate exercise test were excluded. As a result, 150 patients were enrolled and classified according to conduit size. We compared with their exercise capacity and analyzed correlation between exercise capacity and conduit size per body surface area (BSA). 97 Males were included and mean age was 17.5 ± 5.1 years old. In cardiac catheterization, central venous pressure (CVP) was 12.4 ± 2.5 mmHg and pulmonary vascular resistance was 1.2 ± 0.5 wu m2. In cardiopulmonary exercise test, predictive peak VO2 was 59.1 ± 9.7% and VE/VCO2 was 36.2 ± 6.9. In analysis using quadratic model, impacts of gender, age at Fontan operation, ventricular morphology, isomerism, and fenestration on exercise capacity were excluded and conduit size per BSA had a significant curved correlation with predictive peak VO2 and VE/VCO2. Our results showed that patients with about 12.5 mm/m2 conduit per BSA have the best exercise capacity. Patients with larger than smaller-sized conduit were found to be more attenuated in their ability to exercise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Fontan operation is considered definitive palliation in patients with single-ventricle physiology. Since its first description in 1971 [1], several modifications have been introduced, including the lateral tunnel or fenestrated Fontan operation [2, 3]. Lacking a subpulmonic ventricle, the Fontan circulation has to maintain high systemic venous pressure and low pulmonary artery pressure and the preload is limited [4, 5]. The limitation of preload is more prominent during exercise [6]. In extracardiac conduit type Fontan circulation, conduit size can be an important factor in determining preload [6, 7].
In an extracardiac Fontan operation, a larger conduit for body size is used to allow for the patient growth. However, a large conduit causes inefficient flow due to turbulence or stagnation and might cause later problems such as thrombosis or stenosis [8, 9]. Despite improvements in surgical strategies and techniques, the optimal conduit size in the extracardiac Fontan operation has not yet been determined. We aimed to determine optimal extracardiac conduit size based on exercise capacity in patients with Fontan circulation.
Subjects and Methods
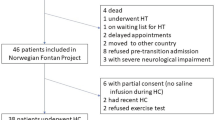
We retrospectively reviewed the medical records of 677 patients over 10 years old who underwent a Fontan operation in Seoul National University and Sejong General Hospital. Of these, 46 were mortality or heart transplantation cases, and 228 did not have extracardiac conduit type Fontan circulation (atriopulmonary, lateral tunnel type, and Kawashima type). A total of 527 patients were excluded for various causes that could limit exercise capacity (Table 1). We compared hemodynamic data from cardiac catheterization and results from cardiopulmonary exercise test. The correlation between results from cardiopulmonary exercise test and conduit diameter for body surface area was analyzed.
Patients underwent progressive exercise testing with expiratory gas analysis. Cardiopulmonary exercise testing (Quinton Q-stress®, Cardiac Science, WI, USA/Vmax®, CareFusion, CA, USA/GE Medical systems, T2100 CASE, Mexico) was performed with a modified Bruce protocol. Expiratory gas analysis was performed with a Medical Graphics metabolic cart (TrueOne 2400®, ParvoMedics, Salt Lake City, UT, US). Oxygen consumption, carbon dioxide production (VCO2), and minute ventilation (VE) were measured on a breath by breath basis and analyzed in 15-s intervals. Peak VO2 was defined as the highest VO2 achieved by the subject during the test. Ventilatory anaerobic threshold (VAT) was measured using the V-slope method when it could be accurately determined [10]. Values for VO2 were indexed to body surface and expressed as percentage of predicted values for healthy age- and sex-matched subjects as reported by Cooper and Weiler-Ravell [11]. The ventilatory equivalent of carbon dioxide (VE/VCO2) was measured at the ventilatory anaerobic threshold (VAT) determined with the V-slope method [10]. The respiratory exchange ratio (RER) (VCO2/VO2) was measured continuously. The pulse O2 (VO2/heart rate [HR]) was measured at peak VO2 and indexed to body surface area. The pulse O2 was equal to the product of stroke volume and the arterial-venous O2 content difference. Because the arterial-venous O2 content difference at peak exercise varies little among subjects, the pulse O2 was used as a surrogate for stroke volume at peak exercise [12].
Resting 12-lead electrocardiograms were performed in sitting and standing position and during brief hyperventilation. Heart rate was monitored continuously. The chronotropic index, a measure of response that is independent of resting HR and stroke volume, was defined as: chronotropic index = (maximal achieved HR − resting HR)/(predicted maximal HR − resting HR) [13, 14].
Cardiac catheterization was performed with the patient conscious and the pressure and oxygen saturation were measured in a stable state. Calculation of systemic and pulmonary flow and their ratio (Qp/Qs) was made using the principles described by Fick, with assumed values for O2 consumption according to data published by LeFarge and Miettinen [15]. The superior and inferior vena cava saturations were taken as the mixed venous and systemic arterial saturation in the descending thoracic aorta. Pulmonary venous saturations were obtained by pulmonary artery wedge or left ventricle indirectly. Total pulmonary vascular resistance was expressed in indexed Woods Units (WU). An oxygen delivery was calculated as the product of the cardiac index and arterial O2 content. Because all initial hemodynamic evaluations were performed with the patient breathing room air, the contribution of dissolved O2 was excluded from these calculations. Cardiac catheterization was performed by a pediatric cardiologist with more than 5 years of experience.
Statistical analysis was performed with SPSS 22.0 (SPSS Inc., Chicago, IL, USA) for Windows and R. Descriptive data are presented as numbers with percentage, mean with standard deviation (SD) as appropriate. Generalized additive model (GAM) is a method for finding the non-linear relationship between independent variables and response variables using nonparametric function assuming that the relationship between independent variables and response variables is not linear. Generalized additive model (GAM) is applied to identify non-linear association between conduit diameter per BSA and predicted peak VO2. We also performed GAM between conduit diameter per BSA and VE/VCO2 with adjustment for gender, Fontan operation age, ventricular Morphology, isomerism, and Fenestration. Statistical test were two sided, and a p value ≤ 0.05 was considered statistically significant. All analyses were performed by using SPSS 25.0 (IBM Corp., Armonk, NY, USA) and R software (version 3.4.1; The Comprehensive R Archive Network: https://cran.r-project.org). This study was approved by the institutional review board in Seoul National University and Sejong General Hospital.
Results
The medical records of 677 patients were reviewed and 527 were excluded for various causes limiting exercise capacity (Table 1). The baseline patient characteristics are shown in Table 2. In correlation study between predictive peak VO2 and hemodynamic data from cardiac catheterization such as CVP, VEDP, PVR, and Qs, only CVP had significant linear negative correlation with peak VO2 (p value 0.026). In correlation study between VE/VCO2 and hemodynamic data from cardiac catheterization such as CVP, VEDP, PVR, and Qs, only VEDP had significant linear negative correlation with peak VO2 (p value 0.041).
For adjusting the impact of other factors on exercise capacity, we analyzed by quadratic model (Tables 3, 4). Analysis of the correlation between predicted peak VO2 and conduit diameter per body surface area (BSA) showed a significant convex curved correlation (p = 0.0387) and a maximum peak VO2 at about 12.7 mm/m2 conduit diameter per BSA. (Fig. 1a) We analyzed the correlation between VE/VCO2 and conduit diameter per BSA. These patients showed a significant concave curved correlation pattern (p = 0.0211) (Fig. 1b), with a lowest value at 12.4 mm/m2 conduit diameter per BSA. Patients had maximum exercise capacity at about 12.5 mm/m2. Even though we analyzed the significance between exercise capacity and other factors such as age at Fontan operation, ventricular morphology, isomerism, and fenestration in Fontan pathway, they did not showed the significance statistically (Tables 3, 4).
Correlation analysis between predicted peak VO2 and conduit diameter per body surface area (a) showed a significant convex curved pattern and a maximum peak VO2 at about 12.7 mm/m2 conduit diameter per BSA. Correlation analysis between VE/VCO2 and conduit diameter per BSA (b) showed a significant concave curved correlation
Discussion
Our results showed that patients with extracardiac Fontan circulation showed maximum exercise capacity at about 12.5 mm/m2 conduit diameter per BSA. More importantly, the group with smaller conduits showed better exercise capacity than those with larger conduits. Most surgeons have determined conduit size based on the size of the inferior vena cava [9]. As an extracardiac conduit using a Gore-Tex conduit does not have growth potential, there may be concern that a smaller conduit can cause hemodynamic problems as the patient grows. Particularly because of the small size of the inferior vena cava with use of a small conduit (especially a 16-mm Gore-Tex conduit), this limitation has been a concern and larger conduits have been used [16]. However, our results showed that patients with larger conduits showed a greater decrease in exercise capacity. These results suggest that flow stagnation with use of a larger conduit rather than flow disturbance with use of a smaller conduit negatively affects exercise capacity. Similar results have been reported in prior studies using computational models [8]. In this study, 16- and 18-mm conduits were found to be optimal and larger conduits had redundant space. In our study, the size of the optimal conduit was about 20 mm when considering the body surface area of the patient (BSA 1.57 m2 × 12.5 mm), and results of the previous study are almost the same considering the luminal stenosis by intimal endothelization.
The other theoretical background of this phenomenon is based on the conduit area change rate. (Fig. 2a) Based on a 20-mm conduit, although 16-mm and 24-mm conduits have the same diameter difference, the area change rate is not same. The area change rate of the 16-mm conduit is − 35.9% and area change rate of the 24-mm conduit is + 43.9%. As the size of the conduit increases, the rate of change in the conduit area is greater than the rate when it increases. In addition, luminal narrowing caused by endothelization of the Gore-Tex conduit further exacerbates the difference in the area change rate between large and small conduit (Fig. 2b). Therefore, it is thought that when the conduit size is increased based on an optimal size, the change rate of the area is larger, causing a further decrease in exercise capacity.
The most difficult aspect of this study was the selection of appropriate patients. In fact, this study was not easy because there were too many factors that could affect exercise capacity [7]. Therefore, the authors analyzed patients in detail and excluded all patients with factors that could affect their exercise capacity. Only 150 of the 677 patients in both institutions were included in the study. Patients with suspected bronchial, pulmonary arterial or pulmonary parenchymal abnormalities on chest CT were excluded. Because patients with a fenestration or veno-veno collateral vessels have increased VE/VCO2 [17], those with a fenestration on imaging or a lung/whole body ratio < 0.9 on a radioisotope scan were excluded from analysis of VE/VCO2.
Statistical analysis was also a problem. As shown in previous results, the relationship between the predicted peak VO2 and conduit size and the relationship between the VE/VCO2 and conduit size showed curved correlation patterns (Fig. 1a, b). A curved correlation pattern cannot exclude the influence of other factors. Therefore, to rule out such interference, we used the quadratic model and could exclude influence by gender, age at Fontan age, ventricular morphology, isomerism, and fenestration.
As a retrospective and double-center study, this research had several limitations. Moreover, there can be a selection bias because this study included a small number of patients with heterogeneous diseases. Pulmonary function testing was not performed in many patients and airway or pulmonary parenchymal diseases were excluded by chest CT angiography. We did not directly measure preload, but estimated the value based on cardiopulmonary exercise test. However, it was difficult to measure the preload in a static state with current technology, and was even more difficult to measure during exercise. The curved correlation pattern did not completely eliminate the influence of other factors; however, we overcame this problem by quadratic model.
Despite the above limitations, our study was significant for several reasons. The optimal conduit size in Fontan circulation was found to be about 12.5 mm/m2 conduit diameter per BSA (18 or 20 mm Gore-Tex conduit); these patients showed the best exercise capacity. Patients with larger conduits were less able to exercise. These results suggest that larger-sized conduit from optimal size may be more attenuating factor rather than smaller for supplying preload during exercise. Therefore, we need not try to put in too large sized conduit in operation room. We discussed the theoretical background using the area change rate concept.
Abbreviations
- BSA:
-
Body surface area
- CVP:
-
Central venous pressure
- HR:
-
Heart rate
- PVRi:
-
Pulmonary vascular resistance index
- Qs:
-
Systemic blood flow
- RER:
-
Respiratory exchange ratio
- SD:
-
Standard deviation
- VAT:
-
Ventilatory anaerobic threshold
- VCO2 :
-
Minute carbon dioxide production
- VE:
-
Minute ventilation
- VEDP:
-
Ventricular end-diastolic pressure
- VO2 :
-
Oxygen consumption
References
Fontan F, Baudet E (1971) Surgical repair of tricuspid atresia. Thorax 26(3):240–248
Burkhart HM, Dearani JA, Mair DD, Warnes CA, Rowland CC, Schaff HV, Puga FJ, Danielson GK (2003) The modified Fontan procedure: early and late results in 132 adult patients. J Thorac Cardiovasc Surg 125(6):1252–1259
Petrossian E, Reddy VM, McElhinney DB, Akkersdijk GP, Moore P, Parry AJ, Thompson LD, Hanley FL (1999) Early results of the extracardiac conduit Fontan operation. J Thorac Cardiovasc Surg 117(4):688–696. https://doi.org/10.1016/S0022-5223(99)70288-6
Gewillig M, Brown SC, Eyskens B, Heying R, Ganame J, Budts W, La Gerche A, Gorenflo M (2010) The Fontan circulation: who controls cardiac output? Interact Cardiovasc Thoracic Surg 10(3):428–433. https://doi.org/10.1510/icvts.2009.218594
Hammel JM (2017) The lonely ventricle in chronic Fontan circulation. J Thoracic Cardiovasc Surg 154(1):e9. https://doi.org/10.1016/j.jtcvs.2017.03.058
Shachar GB, Fuhrman BP, Wang Y, Lucas RV Jr, Lock JE (1982) Rest and exercise hemodynamics after the Fontan procedure. Circulation 65(6):1043–1048
Gewillig MH, Lundstrom UR, Bull C, Wyse RK, Deanfield JE (1990) Exercise responses in patients with congenital heart disease after Fontan repair: patterns and determinants of performance. J Am Coll Cardiol 15(6):1424–1432
Itatani K, Miyaji K, Tomoyasu T, Nakahata Y, Ohara K, Takamoto S, Ishii M (2009) Optimal conduit size of the extracardiac Fontan operation based on energy loss and flow stagnation (discussion 572–563). Ann Thorac Surg 88(2):565–572. https://doi.org/10.1016/j.athoracsur.2009.04.109(discussion 572–563)
Alexi-Meskishvili V, Ovroutski S, Ewert P, Dahnert I, Berger F, Lange PE, Hetzer R (2000) Optimal conduit size for extracardiac Fontan operation. Eur J Cardio-Thorac Surg 18(6):690–695
Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60(6):2020–2027
Cooper DM, Weiler-Ravell D (1984) Gas exchange response to exercise in children. Am Rev Respir Dis 129(2 Pt 2):S47–S48. https://doi.org/10.1164/arrd.1984.129.2P2.S47
Wasserman K HJ, Sue DY, Casaburi R, Whipp BJ (1999) Principles of exercise testing and interpretation. In: Clinical exercise testing, 3rd edn. Lippincott, Philadelphia,
Dresing TJ, Blackstone EH, Pashkow FJ, Snader CE, Marwick TH, Lauer MS (2000) Usefulness of impaired chronotropic response to exercise as a predictor of mortality, independent of the severity of coronary artery disease. Am J Cardiol 86(6):602–609
Elhendy A, van Domburg RT, Bax JJ, Nierop PR, Geleijnse ML, Ibrahim MM, Roelandt JR (1999) The functional significance of chronotropic incompetence during dobutamine stress test. Heart 81(4):398–403
LaFarge CG, Miettinen OS (1970) The estimation of oxygen consumption. Cardiovasc Res 4(1):23–30
Cho S, Kim WH, Choi ES, Kwak JG, Chang HW, Hyun K, Lee CH (2017) Outcomes after extracardiac Fontan procedure with a 16-mm polytetrafluoroethylene conduit. Eur J Cardio-Thorac Surg 1:1. https://doi.org/10.1093/ejcts/ezx238
Meadows J, Lang P, Marx G, Rhodes J (2008) Fontan fenestration closure has no acute effect on exercise capacity but improves ventilatory response to exercise. J Am Coll Cardiol 52(2):108–113. https://doi.org/10.1016/j.jacc.2007.12.063
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was waived by this retrospective study from my hospital institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Date and number of IRB approval: Jan 05, 2018/number 1754 (Sejong General Hospital). Date and number of IRB approval: Mar 20, 2019/number H-1812-147-997 (Seoul National University Hospital).
Rights and permissions
About this article
Cite this article
Lee, SY., Song, Mk., Kim, GB. et al. Relation Between Exercise Capacity and Extracardiac Conduit Size in Patients with Fontan Circulation. Pediatr Cardiol 40, 1584–1590 (2019). https://doi.org/10.1007/s00246-019-02190-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-019-02190-4