Abstract
This study examined the progression of left ventricular dysfunction and myocardial fibrosis in patients with Duchenne muscular dystrophy (DMD) or Becker muscular dystrophy (BMD) to evaluate the effects of angiotensin-converting enzyme inhibitor (ACEI). Ninety-eight cardiovascular magnetic resonance (CMR) studies in 34 consecutive patients with DMD (n = 21) or BMD (n = 13) were retrospectively reviewed. Left ventricular ejection fraction (LVEF) and the extent of myocardial late gadolinium enhancement (LGE) were semiautomatically quantified. During the study period, five patients had already been treated with ACEI at the first CMR; five were started on ACEI at LVEF ≥ 55% and 10 at LVEF < 55%. All patients had hyperenhanced myocardium on LGE images at the first CMR (median extent, 3.3%; interquartile range 0.1–14.3%). A mixed-effects model for longitudinal data of each patient, adjusted for age, type of muscular dystrophy, steroid use, and ACEI use showed that higher age (β = − 1.1%/year; 95% confidence interval [CI], − 1.8% to − 0.4%; p = 0.005) and no use of ACEI (β = − 3.1%; 95% CI, − 5.4% to − 0.8%; p = 0.009) were significantly associated with a lower LVEF. When ACEI use was stratified by time of initiation (LVEF ≥ 55% vs. < 55%), only ACEI initiation at LVEF < 55% had a beneficial effect on LVEF at each imaging examination (β = 3.7%; 95% CI, 0.9–6.4%; p = 0.010). ACEI use or the time of initiation of ACEI did not significantly affect age-related increase in LGE. ACEI attenuated the age-related decline in LVEF only in patients with DMD or BMD and reduced LVEF, suggesting that further investigation on prophylactic use of cardioprotective therapy in these patients is warranted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Duchenne muscular dystrophy (DMD) and Becker muscular dystrophy (BMD) are X-linked disorders caused by mutations in the dystrophin gene and characterized by progressive wasting and weakness of skeletal muscles. Although survival in patients with DMD has improved with advances in respiratory care, cardiac complications remain an important determinant of prognosis in patients with DMD [1]. BMD is a milder and more variable phenotype, which maintains the open reading frame of dystrophin; nevertheless, cardiac involvement is seen in approximately 70% of patients with BMD by the age of 40 years [2]. The most common form of cardiac involvement in patients with DMD or BMD is dilated cardiomyopathy [3, 4], presenting as an age-related progressive decline in left ventricular ejection fraction (LVEF) accompanied by myocardial fibrosis, which is detected by late gadolinium enhancement (LGE) cardiovascular magnetic resonance (CMR) imaging [5, 6]. To delay the progression of dilated cardiomyopathy in DMD and BMD, the American Heart Association scientific statement recommends the use of an angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blocker in patients with reduced LVEF [7]. Furthermore, previous studies reported that the prophylactic use of ACEI in patients with DMD or BMD and normal LVEF was associated with delaying myocardial fibrosis [8] and decreasing all-cause mortality [9]. However, the prophylactic effects of ACEI on LVEF and the extent of LGE in these patients have not been fully investigated. Therefore, we examined the progression of left ventricular dysfunction and myocardial fibrosis using CMR in DMD and BMD cohorts to evaluate the longitudinal effects of ACEI on LVEF and the extent of LGE.
Materials and methods
Study population
All consecutive patients with DMD (n = 21) or BMD (n = 13) referred for clinically indicated CMR to our hospital between January 2013 and August 2017 were retrospectively included in this study. Patients with other neuromuscular disease were excluded. The study was approved by the Institutional Review Board (IRB No. 017–0207) with a waiver of written informed consent. The medical records of all patients in the study were reviewed, and DMD or BMD was ascertained by a clinical examination, dystrophin gene analysis by multiplex ligation-dependent probe amplification, the absence or reduction of dystrophin in muscle biopsy, and family history of DMD or BMD. Every clinical visit consisted of a review of medication use and blood tests, including total creatine kinase, brain natriuretic peptide (BNP), human atrial natriuretic peptide, and troponin T. According to the current recommendations [7], ACEI treatment was started in patients with reduced LVEF basically, although the time of ACEI initiation was considered on an individual basis at discretion of their physicians.
CMR imaging protocol
CMR imaging was performed using a 1.5-T whole-body scanner (Achieva; Philips Medical Systems, Best, the Netherlands) with a 5-channel phased-array cardiac coil during repeated breath-holds if tolerated. After localization of the heart, left ventricular (LV) short-axis cine images were obtained using a retrospectively electrocardiogram-gated, balanced steady-state free precession pulse sequence with the following parameters: field of view, 380 mm; repetition time, 2.8 ms; echo time, 1.38 ms; flip angle, 60°; slice thickness, 10 mm; acquisition matrix, 192 × 164 pixels; sensitivity encoding parallel imaging factor, 2.5; and 20 phases per cardiac cycle. LGE images were obtained 10–15 min after administration of 0.1 mmol/kg of Gd-DTPA (Magnevist; Bayer, Osaka, Japan) using an inversion-recovery-prepared, 3-dimensional fast field echo pulse sequence with the following parameters: spectral presaturation with inversion recovery for fat suppression; field of view, 400 mm; repetition time, 3.4 ms; echo time, 1.04 ms; flip angle, 15°; slice thickness, 5 mm with no gap; inversion time, 250–290 ms; acquisition matrix, 224 × 96 pixels; and sensitivity encoding parallel imaging factor, 2. The optimal inversion time was selected to null the signal from normal myocardium using a Look-Locker sequence. Sedation during CMR was performed at the physician’s discretion. Body weight and height were ascertained at the time of CMR examination by interviewing patients and their parents or by using medical records. Body surface area was calculated using the Dubois formula: body weight (kg)0.425 × height (cm)0.725 × 0.007184.
CMR image analysis
CMR image analysis was performed using commercially available software (Ziostation2; Ziosoft Inc., Tokyo, Japan). LV volumes, mass, and LVEF were measured by semiautomatically outlining endocardial and epicardial borders of the myocardium on the short-axis cine images, as previously described [10]. The LV myocardium was automatically divided into 16 segments of the American Heart Association 17-segment model, excluding the apex segment. Two observers (with 4 and 20 years of experience in cardiac imaging, respectively) independently assessed the presence of hyperenhanced myocardium in each segment on LGE images. After the initial assessment, any interobserver disagreements were resolved by consensus. The extent of hyperenhanced myocardium on LGE images was quantified as the percentage area of hyperenhanced myocardium using a 5-standard deviation threshold above the mean of remote myocardium [8, 11] (Fig. 1). We defined substantial LGE as the extent of hyperenhancement ≥ 5% of total LV mass on the basis of previous study [12].
Representative late gadolinium enhancement images of a 15-year-old boy with Becker muscular dystrophy. a Hyperenhanced myocardium was seen in the inferior to lateral and septal wall. b Yellow areas denote myocardium ≥ 5 standard deviations above the mean for signal intensity in the remote myocardium
Statistical analysis
Continuous variables are presented as medians with interquartile range (IQR). Categorical variables are presented as absolute numbers with percentages. Differences between groups were evaluated using the Wilcoxon rank sum test for continuous data and the Fisher exact test for categorical data. Correlations between continuous variables were examined using Spearman rank correlation coefficients (ρ). We assessed the relationship between age-related decline in LVEF or increase in the extent of LGE, the type of muscular dystrophy, and medication use (steroid and ACEI) using a mixed-effects model with a random intercept and slope for longitudinal data of each patient [6] to maximize statistical power. To test the effectiveness of prophylactic use of ACEI, a stratified analysis by time of initiation of the ACEI (initiated at LVEF ≥ 55% vs. < 55%) was performed. β-blocker use was not adjusted in the mixed-effects model analysis [13] because a previous study reported that concomitant use of β-blocker with ACEI did not affect LVEF in patients with DMD [14]. A 2-tailed p value of < 0.05 was considered statistically significant. All statistical analyses were performed using JMP Pro 13.1.0 (SAS Institute Inc., Cary, NC).
Results
Patient characteristics
In total, 34 patients underwent at least 1 CMR study during the study period (total 98 studies), and 24 of these patients had ≥ 2 CMR studies (median follow-up duration, 3.0 years; range 0.6–4.1 years). During the follow-up period, none of the patients died or was admitted for decompensated heart failure. Baseline patient characteristics at the first and last CMR are summarized in Tables 1 and 2, respectively. At the initial examination, the median patient age was 11.9 years (IQR 6.4–15.9 years) and 33 patients (97%) were men. Among the 21 patients with DMD, 8 (38%) were already wheelchair-bound and 8 (38%) were being treated with prednisolone (median dose 7.0 mg/day; IQR 5.0–8.3 mg/day). Five patients with DMD (median LVEF 37.5%; IQR 22.6–58.0%) were being treated with ACEI, and three of these five patients who had an LVEF < 55% were also being treated with β-blocker. During the study period, five patients were started on ACEI at LVEF ≥ 55%; 10 at LVEF < 55%; and none of the patients died. Among patients treated with ACEI (n = 20), 1 patient was prescribed cilazapril (1.5 mg/day), and the other patients were prescribed enalapril, of which median dose achieved at the end of the study period was 10 mg/day (IQR 7.2–10.0 mg/day). All patients treated with β-blocker (n = 5) were prescribed bisoprolol, of which median dose achieved at the end of the study period was 2.5 mg/day (IQR 0.625–2.5 mg/day). At baseline, nine patients had elevated BNP levels (> 18.4 pg/mL) and 25 had elevated serum troponin T levels (> 0.014 ng/mL). The levels of serum total creatine kinase, troponin T, and plasma BNP in patients with DMD were significantly higher than those in patients with BMD (Table 1).
Baseline CMR imaging results and relationship with clinical variables
Baseline CMR results were similar in patients with DMD and BMD (Table 1); there was no significant difference in baseline LVEF and end-diastolic and end-systolic volume indices. One patient with DMD underwent only cine CMR and did not undergo LGE imaging at the time of the first CMR study because he could not lie still in bed during the examination. All other patients were considered as LGE positive on visual assessment, which was typically the subepicardial location in the lateral wall. The extent of LGE at the first CMR was varied (median extent, 3.3% of LV mass; IQR 0.1–14.3%). Patients with substantial LGE (≥ 5% of total LV mass) (n = 14) had a lower LVEF than those without (n = 19) (42.7% [IQR 32.3–58.2%] vs. 55.1% [IQR 52.6–58.5%], p = 0.040). None of the patients aged < 10 years (n = 14) had substantial LGE, and eight patients (6 DMD and 2 BMD) aged < 10 years had LVEF < 55%.
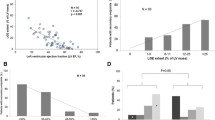
Regarding the first CMR, the extent of LGE showed a negative correlation with LVEF (Spearman ρ = − 0.59, p < 0.001) (Fig. 2), end-diastolic volume index (Spearman ρ = 0.56, p < 0.001), and end-systolic volume index (Spearman ρ = 0.62, p < 0.001). Among CMR variables and blood test data, the levels of plasma BNP were significantly correlated with LVEF (Spearman ρ = − 0.56, p < 0.001) and the extent of LGE (Spearman ρ = 0.64, p < 0.001). The levels of serum troponin T and plasma human atrial natriuretic peptide were not significantly correlated with any CMR variables. The elevated levels of plasma BNP for detecting substantial LGE, with a cutoff value of ≥ 18.4 pg/mL, yielded a sensitivity of 57%, a specificity of 95%, a positive predictive value of 89%, and a negative predictive value of 75%. The area under the curve of plasma BNP for detecting substantial LGE was 0.79.
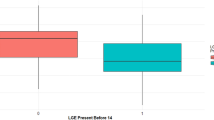
Longitudinal relationship between age and LVEF in muscular dystrophy
A mixed-effects model including only age showed that LVEF significantly decreased by 0.7% per year (95% confidence interval [CI], 0.004–1.3%; p = 0.049) (Fig. 3). On including the type of muscular dystrophy and a linear interaction term (age × BMD) in this model, LVEF significantly decreased by 1.1% per year (95% CI, 0.2–1.9%; p = 0.016), whereas additional variables were not significantly associated with LVEF (p = 0.78 and p = 0.20, respectively), indicating that the type of muscular dystrophy did not attenuate age-related decline in LVEF.
Longitudinal relationship between age and left ventricular ejection fraction (LVEF). Each patient [red circles, Duchenne muscular dystrophy (DMD); blue circles, Becker muscular dystrophy (BMD)] is connected by a colored line during follow-up. The filled and open circles denote patients treated with and without angiotensin-converting enzyme inhibitor (ACEI), respectively. LVEF decreased by 0.65% ± 0.31% (β ± standard error) per year in a mixed-effects model adjusted for age only
Longitudinal effect of ACEIs on LVEF in muscular dystrophy
Table 3 summarizes the results of mixed-effects models including medication use to identify predictors of LVEF in patients with DMD or BMD. In a multivariate analysis including age, the type of muscular dystrophy, and medication use (Model 1), lower age and ACEI use were significantly associated with a higher LVEF (p = 0.005 and p = 0.009, respectively). When the time of initiation of ACEI was stratified (Model 2), lower age and ACEI initiation at LVEF < 55% were significantly associated with a higher LVEF (p = 0.005 and p = 0.010, respectively), whereas ACEI introduction at LVEF ≥ 55% was not significantly associated with a higher LVEF (p = 0.24).
Longitudinal relationship between age, treatment, and myocardial fibrosis in muscular dystrophy
Table 4 summarizes the results of mixed-effects models to identify predictors of the extent of LGE in patients with DMD or BMD. In a multivariate analysis including age and the type of muscular dystrophy (Model 1), a higher age was significantly associated with a larger extent of LGE (p = 0.005). ACEI use (Model 2) or the time of initiation of ACEI (Model 3) did not significantly affect age-related increase in LGE.
Discussion
This study showed that ACEI initiation at LVEF < 55%, but not LVEF ≥ 55%, significantly attenuated the age-related decline in LVEF in patients with DMD or BMD. However, ACEI use did not affect the age-related increase in myocardial fibrosis detected by LGE. Importantly, ACEI treatment for DMD and BMD may be effective only in patients with reduced LVEF.
ACEI are a standard therapy for DMD and BMD with systolic heart failure [7]. It was found that ACEI initiation at LVEF < 55% was significantly associated with a higher LVEF in patients with DMD or BMD, which is in line with previous reports [3, 13]. We also found that there was no significant association between ACEI initiation at LVEF ≥ 55% and progressive decline in LVEF. In 2005, Duboc et al. reported on the prophylactic effects of ACEI on LVEF in patients with DMD with LVEF > 55% (mean LVEF, 65.0% ± 5.4%) [15]. However, this earlier randomized trial did not show a significant difference in mean LVEF between patients treated with and without ACEI at 3-year follow-up (60.7% ± 7.6% vs. 64.4% ± 9.8%; p = not significant). Although they also reported that the prophylactic use of ACEI was significantly associated with a lower mortality in patients with DMD after 10-year follow-up [9], the effects of steroid therapy, which yielded a survival benefit for patients with DMD [16], were not considered in these results. Recently, Silva et al. reported that in their randomized clinical trial, early initiation of ACEI was associated with an attenuation of myocardial fibrosis progression in patients with DMD or BMD with LVEF ≥ 50% [8]; however, they also reported that there was no significant difference in 2-year decline in LVEF between patients treated with and without ACEI (− 6.2% ± 6.0% vs. − 4.9% ± 6.4%, p = 0.94). Although ACEI treatment is usually well tolerated, it is well known that use of ACEI can cause chronic cough, symptomatic hypotension, and angioedema. Given the lack of conclusive evidence on the benefit of prophylactic ACEI for DMD or BMD patients with normal LVEF, we should be careful to ensure that ACEI treatment is effective in all stages of the disease. These results also suggest that annual CMR is preferable for patients with normal LVEF to detect changes in LVEF and myocardial fibrosis.
ACEI use or the time of initiation of ACEI did not significantly affect age-related progressive myocardial fibrosis detected by LGE. On the basis of this finding, only a small fraction of the benefits of ACEI could be attributed to a reduction in myocardial fibrosis, suggesting that the benefits of ACEI among patients with reduced LVEF are mediated by reduction in left ventricular preload and afterload or reduction in sympathetic stimulation [17].
The extent of LGE was moderately correlated with LVEF and LV volume. However, we found that eight patients aged < 10 years had an LVEF < 55% even without substantial LGE (≥ 5% of total LV mass). Although LGE is well established for detecting myocardial fibrosis, these findings suggest that LGE may not always detect fibrotic changes, particularly when these occur diffusely in patients with DMD or BMD. This concern has been raised about a variety of other nonischemic cardiomyopathies [18]. In this regard, previous studies suggested that circumferential strain analysis [19] or T1 and extracellular volume fraction mapping [20] using CMR may be more suited to detecting diffuse myocardial damage in patients with DMD and normal LVEF.
Cardiac biomarkers for early detection of cardiac dysfunction or myocardial damage have been used in various settings of heart failure [21]. We found that most patients with DMD or BMB had an elevated level of serum troponin T at baseline, probably reflecting latent and progressive myocardial damage, and that those with elevated levels of plasma BNP were more likely to have a substantial LGE. BNP or N-terminal pro-BNP is the most widely used biomarker for the detection and management of heart failure, which may be useful for risk stratification in pediatric outpatients [22] and in patients with DMD [23]. Our results suggest that significant elevation in plasma BNP levels may be a sign of substantial myocardial fibrosis.
Study limitations
This study has several limitations. First, it is a single-center retrospective study and is subject to selection bias. Although the patients were treated at the discretion of their physicians, the latter were all experienced pediatric cardiologists. Second, the small sample size did not allow for separate analysis by the type of muscular dystrophy. Although the natural course of progressive cardiac involvement might differ between DMD and BMD, cardioprotective effects of ACEI were found to be independent of the type of muscular dystrophy in multivariate analysis. Third, we did not assess the effects of combination therapy with aldosterone antagonists, which may attenuate progressive LV systolic dysfunction in patients with DMD [24] or BMD. Therefore, further studies are needed to expand upon the present findings in an effort to improve the management of muscular dystrophy patients with cardiac involvement and normal LVEF.
Conclusions
ACEI attenuated the age-related decline in LVEF only in patients with DMD or BMD and reduced LVEF. However, ACEI use did not affect the age-related increase in myocardial fibrosis in patients with DMD or BMD.
References
Eagle M, Baudouin SV, Chandler C, Giddings DR, Bullock R, Bushby K (2002) Survival in Duchenne muscular dystrophy: improvements in life expectancy since 1967 and the impact of home nocturnal ventilation. Neuromuscul Disord 12:926–929. https://doi.org/10.1016/S0960-8966(02)00140-2
Melacini P, Fanin M, Danieli GA, Villanova C, Martinello F, Miorin M, Freda MP, Miorelli M, Mostacciuolo ML, Fasoli G, Angelini C, Volta SD (1996) Myocardial involvement is very frequent among patients affected with subclinical Becker’s muscular dystrophy. Circulation 94:3168–3175. https://doi.org/10.1161/01.CIR.94.12.3168
Jefferies JL, Eidem BW, Belmont JW, Craigen WJ, Ware SM, Fernbach SD, Neish SR, Smith EO, Towbin JA (2005) Genetic predictors and remodeling of dilated cardiomyopathy in muscular dystrophy. Circulation 112:2799–2804. https://doi.org/10.1161/CIRCULATIONAHA.104.528281
Melacini P, Fanin M, Danieli GA, Fasoli G, Villanova C, Angelini C, Vitiello L, Miorelli M, Buja GF, Mostacciuolo ML, Pegoraro E, Volta SD (1993) Cardiac involvement in Becker muscular dystrophy. J Am Coll Cardiol 22:1927–1934. https://doi.org/10.1016/0735-1097(93)90781-U
Silva MC, Meira ZM, Gurgel Giannetti J, da Silva MM, Campos AF, Barbosa Mde M, Starling Filho GM, Ferreira Rde A, Zatz M, Rochitte CE (2007) Myocardial delayed enhancement by magnetic resonance imaging in patients with muscular dystrophy. J Am Coll Cardiol 49:1874–1879. https://doi.org/10.1016/j.jacc.2006.10.078
Tandon A, Villa CR, Hor KN, Jefferies JL, Gao Z, Towbin JA, Wong BL, Mazur W, Fleck RJ, Sticka JJ, Benson DW, Taylor MD (2015) Myocardial fibrosis burden predicts left ventricular ejection fraction and is associated with age and steroid treatment duration in duchenne muscular dystrophy. J Am Heart Assoc. https://doi.org/10.1161/JAHA.114.001338
Feingold B, Mahle WT, Auerbach S, Clemens P, Domenighetti AA, Jefferies JL, Judge DP, Lal AK, Markham LW, Parks WJ, Tsuda T, Wang PJ, Yoo SJ, American Heart Association Pediatric Heart Failure Committee of the Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; Council on Cardiovascular Radiology and Intervention; Council on Functional Genomics and Translational Biology; and Stroke Council (2017) Management of cardiac involvement associated with neuromuscular diseases: a scientific statement From the American Heart Association. Circulation 136:e200–e231. https://doi.org/10.1161/CIR.0000000000000526
Silva MC, Magalhaes TA, Meira ZM, Rassi CH, Andrade AC, Gutierrez PS, Azevedo CF, Gurgel-Giannetti J, Vainzof M, Zatz M, Kalil-Filho R, Rochitte CE (2017) Myocardial fibrosis progression in Duchenne and Becker muscular dystrophy: a randomized clinical trial. JAMA Cardiol 2:190–199. https://doi.org/10.1001/jamacardio.2016.4801
Duboc D, Meune C, Pierre B, Wahbi K, Eymard B, Toutain A, Berard C, Vaksmann G, Weber S, Becane HM (2007) Perindopril preventive treatment on mortality in Duchenne muscular dystrophy: 10 years’ follow-up. Am Heart J 154:596–602. https://doi.org/10.1016/j.ahj.2007.05.014
Aikawa T, Naya M, Obara M, Oyama-Manabe N, Manabe O, Magota K, Ito YM, Katoh C, Tamaki N (2017) Regional interaction between myocardial sympathetic denervation, contractile dysfunction, and fibrosis in heart failure with preserved ejection fraction: 11C-hydroxyephedrine PET study. Eur J Nucl Med Mol Imaging 44:1897–1905. https://doi.org/10.1007/s00259-017-3760-y
Aikawa T, Oyama-Manabe N, Naya M, Ohira H, Sugimoto A, Tsujino I, Obara M, Manabe O, Kudo K, Tsutsui H, Tamaki N (2017) Delayed contrast-enhanced computed tomography in patients with known or suspected cardiac sarcoidosis: a feasibility study. Eur Radiol 27:4054–4063. https://doi.org/10.1007/s00330-017-4824-x
Nassenstein K, Breuckmann F, Bucher C, Kaiser G, Konorza T, Schafer L, Konietzka I, de Greiff A, Heusch G, Erbel R, Barkhausen J (2008) How much myocardial damage is necessary to enable detection of focal late gadolinium enhancement at cardiac MR imaging? Radiology 249:829–835. https://doi.org/10.1148/radiol.2493080457
Allen HD, Flanigan KM, Thrush PT, Dvorchik I, Yin H, Canter C, Connolly AM, Parrish M, McDonald CM, Braunlin E, Colan SD, Day J, Darras B, Mendell JR (2013) A randomized, double-blind trial of lisinopril and losartan for the treatment of cardiomyopathy in duchenne muscular dystrophy. PLoS Curr. https://doi.org/10.1371/currents.md.2cc69a1dae4be7dfe2bcb420024ea865
Viollet L, Thrush PT, Flanigan KM, Mendell JR, Allen HD (2012) Effects of angiotensin-converting enzyme inhibitors and/or beta blockers on the cardiomyopathy in Duchenne muscular dystrophy. Am J Cardiol 110:98–102. https://doi.org/10.1016/j.amjcard.2012.02.064
Duboc D, Meune C, Lerebours G, Devaux JY, Vaksmann G, Becane HM (2005) Effect of perindopril on the onset and progression of left ventricular dysfunction in Duchenne muscular dystrophy. J Am Coll Cardiol 45:855–857. https://doi.org/10.1016/j.jacc.2004.09.078
Schram G, Fournier A, Leduc H, Dahdah N, Therien J, Vanasse M, Khairy P (2013) All-cause mortality and cardiovascular outcomes with prophylactic steroid therapy in Duchenne muscular dystrophy. J Am Coll Cardiol 61:948–954. https://doi.org/10.1016/j.jacc.2012.12.008
Lonn EM, Yusuf S, Jha P, Montague TJ, Teo KK, Benedict CR, Pitt B (1994) Emerging role of angiotensin-converting enzyme inhibitors in cardiac and vascular protection. Circulation 90:2056–2069. https://doi.org/10.1161/01.CIR.90.4.2056
Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA (2011) Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol 57:891–903. https://doi.org/10.1016/j.jacc.2010.11.013
Hor KN, Wansapura J, Markham LW, Mazur W, Cripe LH, Fleck R, Benson DW, Gottliebson WM (2009) Circumferential strain analysis identifies strata of cardiomyopathy in Duchenne muscular dystrophy: a cardiac magnetic resonance tagging study. J Am Coll Cardiol 53:1204–1210. https://doi.org/10.1016/j.jacc.2008.12.032
Soslow JH, Damon SM, Crum K, Lawson MA, Slaughter JC, Xu M, Arai AE, Sawyer DB, Parra DA, Damon BM, Markham LW (2016) Increased myocardial native T1 and extracellular volume in patients with Duchenne muscular dystrophy. J Cardiovasc Magn Reson 18:5. https://doi.org/10.1186/s12968-016-0224-7
Maisel AS, Bhalla V, Braunwald E (2006) Cardiac biomarkers: a contemporary status report. Nat Clin Pract Cardiovasc Med 3:24–34. https://doi.org/10.1038/ncpcardio0405
Price JF, Thomas AK, Grenier M, Eidem BW, O’Brian Smith E, Denfield SW, Towbin JA, Dreyer WJ (2006) B-type natriuretic peptide predicts adverse cardiovascular events in pediatric outpatients with chronic left ventricular systolic dysfunction. Circulation 114:1063–1069. https://doi.org/10.1161/circulationaha.105.608869
Cheeran D, Khan S, Khera R, Bhatt A, Garg S, Grodin JL, Morlend R, Araj FG, Amin AA, Thibodeau JT, Das S, Drazner MH, Mammen PPA (2017) Predictors of death in adults with Duchenne muscular dystrophy-associated cardiomyopathy. J Am Heart Assoc. https://doi.org/10.1161/jaha.117.006340
Raman SV, Hor KN, Mazur W, Halnon NJ, Kissel JT, He X, Tran T, Smart S, McCarthy B, Taylor MD, Jefferies JL, Rafael-Fortney JA, Lowe J, Roble SL, Cripe LH (2015) Eplerenone for early cardiomyopathy in Duchenne muscular dystrophy: a randomised, double-blind, placebo-controlled trial. Lancet Neurol 14:153–161. https://doi.org/10.1016/s1474-4422(14)70318-7
Acknowledgements
We thank Drs. Yukitoshi Isikawa and Yuka Ishikawa for providing DMD/BMD-specific knowledge and insight and Kinya Ishizaka for technical assistance.
Funding
This study was funded by the Miyata Cardiac Research Promotion Foundation (to Tadao Aikawa). The funder had no role in the study design, data collection, analysis, interpretation of data, or in the writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Aikawa, T., Takeda, A., Oyama-Manabe, N. et al. Progressive left ventricular dysfunction and myocardial fibrosis in Duchenne and Becker muscular dystrophy: a longitudinal cardiovascular magnetic resonance study. Pediatr Cardiol 40, 384–392 (2019). https://doi.org/10.1007/s00246-018-2046-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-2046-x