Abstract
Cardiac implantable electronic device (CIED) infections are associated with significant morbidity in the pediatric device population, with a tenfold higher risk of infection in children compared to adults. The 2010 American Heart Association (AHA) guidelines recommend a single dose of systemic antibiotic (ABX) prophylaxis prior to CIED implantation and no post-operative (OP) ABX. However, there is limited data regarding adherence to this recommendation among the pediatric community. To assess current clinical practices for CIED ABX prophylaxis in pediatrics; whether the AHA guidelines are being followed; and if not, the reasons for non-adherence. An anonymous web-based survey was sent to physician members of the Pediatric And Congenital Electrophysiology Society regarding ABX prophylaxis for new CIED implants and reoperations. 75 (25%) members responded. Only 7% of respondents follow the 2010 AHA guidelines. While all respondents give pre-OP IV ABX, 64% routinely treat patients with 24-h post-OP IV ABX with additional oral or IV therapy. 69% of respondents are cognizant of the guidelines but 88% of those cognizant do not follow the guidelines for a variety of reasons including lack of data and different substrate (pediatric patients). 79% stated that pediatric-specific data would be required for them to change their practice and follow the published guidelines. The majority of pediatric EP physicians who responded to this survey do not follow the current AHA guidelines on ABX prophylaxis and administer post-OP ABX. Most pediatric EP physicians believe that the increased risk of infection in children merits additional ABX.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of cardiac implantable electronic devices (CIED) in pediatric patients has expanded in recent years, with implantable cardioverter defibrillator (ICD) utilization in children more than doubling in the 10 years between 1997 and 2006 [1, 2]. While these devices have proven to be lifesaving therapies, complications continue to be a significant problem with rates as high as 10% [3,4,5,6,7]. CIED-related infection remains an important cause of morbidity following CIED implantation. Infection rates have continued to rise disproportionally when compared to rates of new device implant, with studies showing a tenfold higher risk of infection in children compared to adults [8,9,10,11].
The American Heart Association (AHA), with the endorsement of the Heart Rhythm Society and the Infectious Diseases Society of America, issued a scientific statement in 2010 addressing CIED infections and management [12]. The writing committee, citing a large randomized control trial, recommended systemic administration of antibiotic prophylaxis once immediately before device implant [13]. The committee did not recommend the use of antibiotic prophylaxis post-operatively, citing the lack of data for efficacy and concerns for drug adverse events, drug resistance, and cost. While the AHA statement cites multiple studies suggesting higher CIED-related infection rates in the pediatric population, it does not have specific recommendations for antibiotic prophylaxis in pediatric CIED implant procedures.
At present, there is no study examining adherence rates to the AHA guidelines for antibiotic prophylaxis in pediatric clinical practice. We performed an international survey of practicing pediatric electrophysiologists to assess current clinical practices for CIED antibiotics prophylaxis in pediatrics.
Methods
An anonymous web-based survey was sent in 2016 via Qualtrics to physician members of the Pediatric And Congenital Electrophysiology Society (PACES). The survey consisted of 25 Yes/No, multiple choice, and open-ended questions regarding antibiotic prophylaxis for different scenarios concerning new CIED implants and reoperations. Physicians were asked to explain practice preferences such as the antibiotics agents of choice and duration of antibiotic prophylaxis for each of the following scenarios: ICD implant, pacemaker implant, ICD reoperation, and pacemaker reoperation. We also asked whether they had knowledge of the current CIED antibiotic prophylaxis guidelines, and why they chose to follow or not follow these guidelines. Summary statistics of this descriptive study was presented as counts and percentages (n, %) for categorical data.
Results
Respondent Characteristics
A total of 75 PACES physician members of the 305 queried (25%) responded to the survey. 28% of those who responded reported practicing for < 5 years; 23% reported 5–10 years; and 49% reported > 10 years. Median center implant volume was 20 (5–75) CIED implants per year (Table 1).
Survey Responses
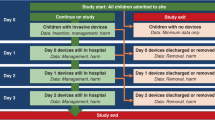
Antibiotic use surrounding CIED use is shown in Fig. 1. The vast majority (99%) of respondents administer prophylactic antibiotics during CIED procedures. Only 7–8% of respondents report to follow the 2010 AHA guidelines (single dose of pre-operative antibiotics) for new device implants and 15–16% for device reoperations. While all respondents give pre-operative IV antibiotics, 93% of respondents report administering additional antibiotics in new device implants and 84% in device reoperations. 64% routinely treat patients with 24 h of post-operative IV antibiotics followed by an additional course of oral or IV antibiotics. Different regimens for epicardial and transvenous systems were reported by 34% of participants. These differences were attributed to operator preference. 89–93% of respondents report administering Cefazolin as the preferred intravenous agent in CIED implant and reoperation procedures and 91% report using Cefalexin as the preferred oral agent in ICD implant procedures.
A majority (69%) of respondents were cognizant of the AHA guidelines. However, 88% of respondents do not practice guideline recommendations. Reasons given for this included personal experience and the fact that children pose a different risk for infection when compared to adult patients. 81% stated that pediatric-specific data would be required for them to change their practice and follow the published guidelines.
Of the five respondents reported to follow the AHA guidelines (single dose of pre-operative antibiotics), all have been in practice for > 10 years and four of the five respondents practice at high implant volume centers (defined as > 20 implants/year). No association was found between guideline awareness and center implant volume or physician years in practice (p = 0.6).
Discussion
This survey demonstrates that the majority of pediatric electrophysiologists do not follow current AHA guidelines regarding antibiotic prophylaxis, citing differences in pediatric versus adult infection rates as one of the main reasons for this discrepancy. The concern about higher device infection rates in children is well supported in the literature. Indeed, the AHA guidelines cite studies supporting the premise that pediatric and congenital heart disease patients have higher infection rates compared to adult patients. Klug et al. reviewed a large pacemaker database and found a much higher infection rate in young patients < 40 years of age (5.5% vs. 1.2% p < 0.001) [14]. They hypothesized that several factors may influence these findings, including higher rates of reintervention and higher likelihood of trauma in young active individuals. ICDs in children also have a high infection rate. In a four center retrospective registry, Berul et al. found an acute infection rate of 1.5% and a chronic infection rate of 2.9% [15]. In a comparison of adults and pediatric patients in the same institution, Link found an ICD infection rate of 18% in pediatric patients compared to 1.2% in adults [11]. Despite these concerning findings, no specific pediatric guidelines were proposed in the AHA guidelines, presumably due to the lack of prospective data.
This dissent from the guidelines is not limited to pediatric practice. Recently, Basil et al. surveyed clinicians on antibiotic prophylaxis practices for CIED procedures in the adult population [16]. According to the study, 50% of respondents administer post-operative intravenous antibiotics in new CIED implant procedures and 25% in device reoperations. Over 20% administer post-operative oral antibiotics in new CIED implant procedures and 35% in device reoperations. While these results are significantly lower than the 93% reported in new CIED implant procedures and 84% in reoperations presented here, they still represent a high number of centers with practice that departs from current AHA guidelines. Survey participants from this study have similar characteristics in the number of years in practice.
Surprisingly, one-third of surveyed pediatric electrophysiologists were not aware of the AHA guidelines. We did not find a significant association between guideline awareness and years in practice or center implant volume. Much has been done to increase awareness of guidelines by the AHA, American College of Cardiology, and Heart Rhythm Society. While it is beyond the scope of this work to address possible reasons for the high rate of unfamiliarity with the guidelines, it does highlight a problem with dissemination of guideline recommendations.
Limitations
As this study was based on a voluntary survey sent to members of PACES, it may not reflect practice preferences of all pediatric electrophysiologists. In addition, not all physicians responded to all of the questions presented.
Conclusions
In conclusion, the majority of pediatric electrophysiologists surveyed do not follow the published AHA guidelines on antibiotic prophylaxis usage for CIED. Further work is needed to reconcile the discrepancy between current practice patterns among pediatric electrophysiologists and current AHA guidelines. While the majority of pediatric electrophysiologists cite a lack of data for their preferences, a prospective randomized study of antibiotic prophylaxis in children would be challenging due to the size, scope, and limited patient population to provide definitive pediatric-specific data that would change individual practices.
References
Zhan C, Baine WB, Sedrakyan A, Steiner C (2008) Cardiac device implantation in the United States from 1997 through 2004: a population-based analysis. J Gen Intern Med 23:13–19
Burns KM, Evans F, Kaltman JR (2011) Pediatric ICD utilization in the United States from 1997 to 2006. Heart Rhythm 8:23–28
Mirowski M, Reid PR, Mower MM et al (1980) Termination of malignant ventricular arrhythmias with an implanted automatic defibrillator in human beings. N Engl J Med 303:322–324
Moss AJ, Liu JE, Gottlieb S, Locati EH, Schwartz PJ, Robinson JL (1991) Efficacy of permanent pacing in the management of high-risk patients with long QT syndrome. Circulation 84:1524–1529
Bardy GH, Lee KL, Mark DB et al (2005) Amiodarone or an implantable cardioverter–defibrillator for congestive heart failure. N Engl J Med 352:225–237
Brignole M, Menozzi C, Moya A et al (2012) Pacemaker therapy in patients with neurally mediated syncope and documented asystole: Third International Study on Syncope of Uncertain Etiology (ISSUE-3): a randomized trial. Circulation 125:2566–2571
Silka MJ, Kron J, Dunnigan A, Dick M (1993) Sudden cardiac death and the use of implantable cardioverter-defibrillators in pediatric patients. Pediatr Electrophysiol Soc Circ 87:800–807
Voigt A, Shalaby A, Saba S (2006) Rising rates of cardiac rhythm management device infections in the United States: 1996 through 2003. J Am Coll Cardiol 48:590–591
Voigt A, Shalaby A, Saba S (2010) Continued rise in rates of cardiovascular implantable electronic device infections in the United States: temporal trends and causative insights. Pacing Clin Electrophysiol 33:414–419
Greenspon AJ, Patel JD, Lau E et al (2011) 16-Year trends in the infection burden for pacemakers and implantable cardioverter-defibrillators in the United States: 1993 to 2008. J Am Coll Cardiol 58:1001–1006
Link MS, Hill SL, Cliff DL et al (1999) Comparison of frequency of complications of implantable cardioverter-defibrillators in children versus adults. Am J Cardiol 83:263–266
Baddour LM, Epstein AE, Erickson CC et al (2010) Update on cardiovascular implantable electronic device infections and their management. Circulation 121:458–477
de Oliveira JC, Martinelli M, Nishioka SADO et al (2009) Efficacy of antibiotic prophylaxis before the implantation of pacemakers and cardioverter-defibrillators. Results of a large, prospective, randomized, double-blinded, placebo-controlled trial. Circulation 2:29–34
Klug D, Vaksmann GUY, JarwÉ M et al (2003) Pacemaker lead infection in young patients. Pacing Clin Electrophysiol 26:1489–1493
Berul CI, Van Hare GF, Kertesz NJ et al (2008) Results of a multicenter retrospective implantable cardioverter-defibrillator registry of pediatric and congenital heart disease patients. J Am Coll Cardiol 51:1685–1691
Basil A, Lubitz SA, Noseworthy PA et al (2017) Periprocedural antibiotic prophylaxis for cardiac implantable electrical device procedures: results from a Heart Rhythm Society Survey. JACC Clin Electrophysiol 3:632–634
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kara S. Motonaga has received educational fellowship support from Medtronic (20K) & Abbott (20K). Anne M. Dubin has received educational fellowship support from Medtronic (20K) & Abbott (20K). The other authors declare that they have no conflict of interest.
Research Involving Human and Animal Participants
This article does not contain any studies with human participants or animals performed by any of the authors.
Appendix
Appendix
Survey Questions
-
1.
Do you routinely use antibiotic prophylaxis when placing new ICDs?
-
2.
Do you give antibiotics:
-
(a)
preoperative IV dose prior to implantation only
-
(b)
preop + 24 h of IV therapy
-
(c)
preop + 24 h of IV therapy followed by 3 days of oral
-
(d)
preop + 24 h of IV followed by 5 days of oral
-
(e)
prep + 24 h of IV followed by 7 days of oral
-
(f)
Other
-
(a)
-
3.
What other antibiotic regimen do you use?
-
4.
Which IV antibiotics do you use?
-
5.
Which oral antibiotics do you use?
-
6.
Do you routinely use antibiotic prophylaxis when placing new pacemakers?
-
7.
Do you give antibiotics:
-
(a)
preoperative IV dose prior to implantation only
-
(b)
preop + 24 h of IV therapy
-
(c)
preop + 24 h of IV therapy followed by 3 days of oral
-
(d)
preop + 24 h of IV followed by 5 days of oral
-
(e)
prep + 24 h of IV followed by 7 days of oral
-
(f)
Other
-
(a)
-
8.
What other antibiotic regiment do you follow?
-
9.
Which IV antibiotics do you use?
-
10.
Do you use antibiotic prophylaxis for ICD generator replacement?
-
11.
Do you give antibiotics:
-
(a)
preoperative IV dose prior to implantation only
-
(b)
preop + 24 h of IV therapy
-
(c)
preop + 24 h of IV therapy followed by 3 days of oral
-
(d)
preop + 24 h of IV followed by 5 days of oral
-
(e)
prep + 24 h of IV followed by 7 days of oral
-
(f)
Other
-
(a)
-
12.
What other antibiotic regimen do you use?
-
13.
Which IV antibiotics do you use?
-
14.
Do you use antibiotic prophylaxis for pacemaker generator replacement?
-
15.
Do you give antibiotics:
-
(a)
preoperative IV dose prior to implantation only
-
(b)
preop + 24 h of IV therapy
-
(c)
preop + 24 h of IV therapy followed by 3 days of oral
-
(d)
preop + 24 h of IV followed by 5 days of oral
-
(e)
prep + 24 h of IV followed by 7 days of oral
-
(f)
Other
-
(a)
-
16.
What other antibiotic regimen do you use?
-
17.
What IV antibiotics do you use?
-
18.
Are you aware of the present AHA guidelines regarding antibiotic prophylaxis?
-
19.
If you are not following these guidelines, why not?
-
(a)
Lack of data
-
(b)
Personal experience
-
(c)
Children are different than adults
-
(d)
Other
-
(a)
-
20.
If you do not follow the guidelines, what would you need to see to convince you to follow them?
-
21.
How long have you been in practice?
-
22.
Number of devices you place per year?
-
23.
Do you have same regimen for epicardial and TV systems?
-
24.
If not, what do you do different?
-
25.
If not, why not?
Rights and permissions
About this article
Cite this article
Chen, S.Y., Ceresnak, S.R., Motonaga, K.S. et al. Antibiotic Prophylaxis Practices in Pediatric Cardiac Implantable Electronic Device Procedures: A Survey of the Pediatric And Congenital Electrophysiology Society (PACES). Pediatr Cardiol 39, 1129–1133 (2018). https://doi.org/10.1007/s00246-018-1865-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-1865-0