Abstract
After an arterial switch operation (ASO), serial imaging is necessary to monitor for maladaptive changes. We compared cardiac magnetic resonance imaging (CMR) to 2-D transthoracic echocardiography (TTE) in assessing post-operative ASO patients. We performed a retrospective review of patients at a single tertiary care center who underwent an ASO and subsequently had a CMR performed from 7/2010 to 7/2016. Those with single ventricle anatomy, congenitally corrected transposition of the great arteries, or previous atrial switch operation were excluded. TTE obtained within 6 months of the CMR was used for comparison. Parameters compared included ventricular size and systolic function, semilunar valve regurgitation, neo-aortic root dimension, and the presence of branch pulmonary artery (PA) stenosis (on CMR by the Nakata index or right/left flow differential; on TTE by peak velocity > 2 m/s or PA diameter Z score < − 2). Forty-seven patients with 90 CMR and 86 TTE studies met inclusion criteria. CMR and TTE assessment of right ventricular (RV) and left ventricular function did not statistically differ. RV dilation was overdetected by TTE (p = 0.046). Right pulmonary artery and left pulmonary artery (LPA) visualization by TTE was worse than CMR (p < 0.01). There was no statistically significant difference between CMR and TTE assessment of branch PA stenosis; however, there was poor agreement between the use of Z score and velocity when determining branch PA stenosis by TTE (κ < 0). Assessment of neo-pulmonary regurgitation (PR) and neo-aortic regurgitation (AR) was significantly different between CMR and TTE (p < 0.05). Assessment for delayed enhancement was performed in 18% of CMR studies (n = 16), with perfusion defects appreciated in three patients. Substantial differences between CMR and TTE exist when examining the post-operative ASO patient. CMR was superior for evaluation of the branch PAs, which commonly require re-intervention. TTE failed to recognize altered ventricular function in several cases. Differences between TTE and CMR could alter management is some cases. Incorporation of CMR into the routine surveillance of patients who received an ASO is warranted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lesions characterized by parallel pulmonary and systemic circulations, including transposition of the great arteries (TGA) or double outlet right ventricle (DORV) with sub-pulmonary ventricular septal defect (VSD), generally require neonatal surgical correction. The arterial switch operation (ASO) is currently the treatment of choice with 25-year survival approaching 97% in some centers [1]. Though the ASO restores in-series cardiopulmonary circulation, patients who undergo this surgical procedure have a re-intervention rate of nearly 25% at 25 years [1]. Thus, close follow-up is essential, and most cardiologists follow these patients at least on a yearly basis.
Non-invasive imaging of the post-operative anatomy is integral to the management of patients who have undergone an ASO. Commonly employed imaging modalities for anatomic and functional cardiac assessment include transthoracic echocardiography (TTE) and cardiac magnetic resonance imaging (CMR). Both TTE and CMR have relative advantages and disadvantages. Currently, little data are available to clinicians to guide selection of either modality for serial monitoring of post-operative changes after the ASO.
Methods
This study was approved by the Baylor College of Medicine Institutional Review Board. We performed a retrospective review of patients who underwent both an ASO at our tertiary level institution and subsequently received a CMR from 07/2010 to 07/2016. Patients were included if they had a TTE performed within 6 months of a CMR, and change in body surface area (BSA) of no greater than 10%. Patients with single ventricle anatomy, congenitally corrected transposition of the great arteries, those who previously had an atrial switch operation, as well as patients who received a surgical or catheter-based intervention between CMR and TTE studies were excluded. Only data provided in the imaging study reports were used for analysis. Parameters analyzed included demographic data, right ventricular (RV) and left ventricular (LV) size and systolic function, semilunar valve function, neo-pulmonary (PA), and neo-aorta (Ao) size. To allow for more direct comparisons, quantitative data were often grouped into qualitative categories.
On CMR, the threshold for RV dilation was a right ventricular end-diastolic volume (RVEDV) of 107 mL/m2 [2]. Right ventricular ejection fraction (EF) of ≥ 48% was defined as normal, 40–47% was mildly depressed, 30–39% was moderately depressed, and < 30% was severely depressed. By TTE, RV size and function were assessed qualitatively. On CMR, the threshold for left ventricular dilation using the left ventricular end-diastolic volume (LVEDV) was 104 mL/m2 [2]. On TTE, LVEDV was calculated with available data from Bullet or Simpson’s biplane methods for ventricular function calculation. With respect to LV systolic function, based on the availability of data, LV EF was determined either by Simpson’s Biplane method (preferred for comparison), Bullet method, or reported qualitative analysis. Left ventricular systolic function was deemed normal, mildly depressed, moderated depressed, or severely depressed based on an EF of ≥ 55, 40–54, 30–39, and < 30% [3], respectively.
On CMR, branch pulmonary stenosis (PS) was determined by Nakata index < 100 mm2/BSA or presence of pulmonary blood flow differential with < 40% flow to the affected lung [4]. On TTE, branch PS was determined by a velocity > 2.0 m/s or 2-D measurement with a z score < − 2.0. By CMR, neo-pulmonary regurgitation (PR) and neo-aortic regurgitation (AR) were grouped into the following categories: none/trivial, mild, moderate, or severe based on a regurgitant fraction of 1–3, 4–20, 21–40, or > 40%, respectively. On TTE, PR and AR were qualitatively reported by the cardiologist, typically based on color Doppler assessment of the regurgitant jet and other factors such as presence of downstream diastolic flow-reversal.
To compare neo-aortic and neo-pulmonary arterial diameters between CMR and TTE, the largest dimension measured on CMR was used for comparison to the measurement obtained by TTE. Additional data gathered that were unique to CMR include the presence of late gadolinium enhancement (LGE) for assessment of myocardial fibrosis and scar.
To address possible selection bias, we compared 50 TTEs from 50 patients who received an ASO but had no CMR performed, to those who had both a TTE and CMR study. Patients in the “TTE only” group were randomly selected from a TTE database.
Statistical analysis was performed with SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA). Data are reported as frequency (n) with proportion (%), or median with interquartile range (IQR, 25th–75th percentile). Statistical analysis included linear mixed-effects, Wilcoxon rank test, t test, Fisher’s exact for paired tests, generalized estimating equations, and Cohen’s kappa co-efficient where appropriate.
Results
Altogether, we identified 259 patients who underwent an ASO at our institution, of which 60 patients had a total of 146 CMR studies performed between 07/2010 and 07/2016. Forty-two distinct patients met inclusion criteria and provided 90 CMR and 86 TTE studies for analysis. Reasons for CMR referral were not comprehensively listed. Data on 50 additional patients who had TTE but no CMR performed were also collected, and demographics of both groups are displayed in Table 1. Parameters compared between CMR and TTE in patients who received an ASO are given in Table 2.
Table 3 demonstrates the degree of agreement between CMR and TTE as assessed by Cohen’s Kappa co-efficient (values < 0 indicate no agreement, 0–0.20 show slight agreement, 0.21–0.40 fair agreement, 0.41–0.60 moderate, 0.61–0.80 substantial agreement, and 0.81–1 is near perfect agreement [5]). There was “fair” agreement only when comparing CMR and TTE for RV function. Otherwise, there was only “slight” or “no agreement” when comparing other parameters. Transthoracic echocardiogram underdetected LV dysfunction in four studies and overstated dysfunction in three studies. Right ventricular dysfunction was underdetected in two studies and overstated in one study by TTE.
To assess for patient selection bias, we compared TTE data from ASO patients who received a CMR to TTE data from ASO patients who did not receive CMR (Table 4). In patients who did not receive CMR, TTE detected RV dilation in 2 (4%) patients, all of whom had normal RV function. Qualitative assessment showed 1 (2%) patient had mild LV dilation and 1 (2%) patient had moderate LV dilation. The LV was mildly hypertrophied in 1 (2%) patient and severely hypertrophied in 1 (2%). In 1 (2%) patient, the LV function was deemed mildly depressed by qualitative assessment. The median LV EF, calculated in 42 patients, was 63% (IQR 61–66). The MPA, RPA, and LPA were measured by TTE in 4 (8%), 20 (40%), and 17 (34%) patients, respectively (Table 5). There was no reported stenosis by 2-D measurement (z score < − 2.0) of the MPA or RPA by TTE, and only 1 (6%) study showed stenosis of the LPA when the vessel was measured. Echocardiogram reports documented Doppler interrogation of the MPA, RPA, and LPA in 20 (40%), 14 (28%), and 14 (28%) of studies, respectively. Among those who underwent Doppler interrogation, using peak velocities > 2 m/s, stenosis was reported in the MPA, RPA, and LPA in 9 (45%), 9 (64%), and 9 (64%) of studies, respectively. In patients who did not receive CMR, TTE demonstrated moderate and severe AR in 1 (2%) and 1 (2%) patients, respectively. In the same patient population, moderate PR was observed in 2 (6%) patients.
Unique to the patients who underwent a CMR, delayed enhancement was performed in 16 (18%) studies, with perfusion defects appreciated in 3 (19%) patients. Additionally, coronary artery stenosis was incidentally found in 1 patient by CMR.
Discussion
This study is the first to our knowledge to directly compare CMR to TTE for assessment of post-operative changes after the ASO. We confirm that CMR imaging is superior to TTE for visualization of the branch pulmonary arteries, as well as detecting RPA stenosis in patients who have undergone an ASO. Mild AR, as well as mild and moderate PR, was underdetected by TTE. Furthermore, TTE over-reported RV dilation.
In general, agreement between TTE and CMR assessment of cardiac structures and function was poor, with CMR considered to be the “gold standard” for anatomical and functional diagnosis between the two modalities. With respect to ventricular systolic function, there was no statistically significant differences as a group; however, TTE failed to detect LV systolic dysfunction in 4 cases. This is important because LV dysfunction is a clinically actionable finding and cardiologists will often start pharmacotherapy when detected.
To assess for possible selection bias, we analyzed TTE findings in patients who had an ASO but did not have a CMR. When compared to the group who received CMR, ASO patients who received only TTE appeared to have less RV dilation and mild AR. Given the limitations of TTE in the assessment of right ventricular size, this may be one reason for referral for CMR in our study population. Other than these parameters, these two groups did not statistically differ, indicating our study sample was representative of a “typical” cohort of patients who underwent an ASO. Therefore, the study population is less likely to be “biased” to have an over-representation of a particular post-operative pathology and is consistent with ASO patient populations from previously described studies [6].
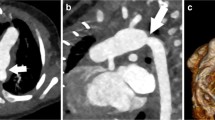
Transthoracic echocardiography is often the clinician’s imaging modality of choice due to ubiquity in the field of cardiology, availability in the majority of settings, and relatively low expense [7]. However, patient body habitus, imaging technique, and certain anatomical arrangements and structures can significantly limit TTE assessment of a patient’s post-operative status [8]. In the ASO, the LeCompte maneuver places the branch PAs anterior to the aorta which can make visualization by TTE difficult. This has clinically important implications because branch PA stenosis after the LeCompte maneuver is frequently seen and is the most common cause for re-intervention after the ASO [9]. Important discrepancies between the detection of at least mild branch PA stenosis were observed in TTE studies; branch PA stenosis detection rate was much higher than direct branch PA 2-D visualization rate by TTE. There was also significant discrepancy between TTE stenosis detection by 2-D and Doppler which highlights the difficulty in using this modality for branch PA evaluation. Often, the RPA diameter measured normal in size by 2-D, but was reported to have flow acceleration of 2 m/s or greater indicating stenosis. This may be due to the stretching of the branch PAs during the LeCompte maneuver, which no longer have a cylindrical shape and limited orthogonal views possible by 2-D. Perhaps the RPA was more likely to be imaged in the sagittal plane and not well seen in the coronal or axial planes, giving the echocardiographer an overestimate of vessel caliber size. Differences between LPA assessment by 2-D and Doppler assessment were not as striking. Doppler interrogation is critical as 2-D measurements alone may lead to false security that the branch PAs are unobstructed. Our study demonstrates that thorough evaluation of the branch PAs is best accomplished by CMR. We should note, however, that there are instances where CMR may not be superior to TTE in evaluation of the branch PAs after ASO, such as in patients who have a PA stent or other foreign material which would obscure CMR images.
In addition to post-operative changes affecting the MPA and branch PAs after the ASO, there is potential for the development of neo-aortic root dilation. Neo-aortic root dilation after the ASO can be progressive and is associated with neo-aortic regurgitation [6].
Post-operatively, there is also a risk of coronary artery “kinking” and myocardial ischemia after coronary artery translocation which requires evaluation. As patients age, acoustic windows on TTE typically change which can result in suboptimal images which may be difficult to interpret. Coronary arteries post ASO are much better imaged by CMR, especially when evaluating older and larger patients [10]. Additional benefits of CMR include detection of myocardial scar by LGE which can indicate issues with the previously manipulated coronary arteries. Currently, the significance of the presence of LGE on CMR among patients who have had an ASO is not known.
The findings in this study demonstrate TTE is inadequate to fully assess the post-operative anatomy after ASO and may miss clinically actionable findings. Therefore, we suggest that practitioners obtain a baseline CMR when the study can be tolerated without anesthesia (usually around 8 years of age), unless otherwise warranted. Additionally, CMR should be incorporated at least intermittently in the routine surveillance of older children and adults who previously had an ASO [11, 12].
Limitations
The retrospective nature and limitations of the inclusion criteria of this study may have biased the data toward patients who have a higher degree of residual lesion. As aforementioned, there were few differences between our study and a “control” ASO group so we believe our results are relevant to patients who have had an ASO. We did not find a trend of improved agreement or additional TTE findings over time. However, as echocardiography technology continues to improve, the differences between TTE and CMR may lessen. Additionally, our study included only patients who received surgical intervention at our institution, and because of differences in surgical outcomes between centers, there may be some limitations with general applicability of these data. Furthermore, other institutions may have different/additional data reported on TTE or CMR reports which could change the findings in this study. The patients included in this study were relatively young in age and if this study were repeated in an older population, results could significantly differ due to factors such as patient cooperation, worse acoustic windows, or progressive post-operative changes. A future, prospective study comparing imaging modality assessment of post-operative changes after an ASO with inclusion of the adult congenital population is warranted.
Conclusion
In patients who received an ASO, CMR is superior to TTE for evaluation of branch PAs. Differences between TTE and CMR could alter management in some cases. Incorporation of CMR in routine surveillance of patients who received an ASO is warranted. Future studies are needed to determine recommended timing interval of CMR evaluation, and may delineate additional differences between the imaging modalities when assessing post-operative changes after an ASO.
References
Khairy P, Clair M, Fernandes SM et al (2013) Cardiovascular outcomes after the arterial switch operation for D-transposition of the great arteries. Circulation 127(3):331–339. https://doi.org/10.1161/CIRCULATIONAHA.112.135046
Robbers-Visser D, Boersma E, Helbing WA (2009) Normal biventricular function, volumes, and mass in children aged 8 to 17 years. J Magn Reson Imaging 29(3):552–559. https://doi.org/10.1002/jmri.21662
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the american society of echocardiography and the european association of cardiovascular imaging. J Am Soc Echocardiogr 28(1):1–39. https://doi.org/10.1016/j.echo.2014.10.003
Nakata S, Imai Y, Takanashi Y et al (1984) A new method for the quantitative standardization of cross-sectional areas of the pulmonary arteries in congenital heart diseases with decreased pulmonary blood flow. J Thorac Cardiovasc Surg 88(4):610–619
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Shepard CW, Germanakis I, White MT, Powell AJ, Co-Vu J, Geva T (2016) Cardiovascular magnetic resonance findings late after the arterial switch operation. Circ Cardiovasc Imaging. https://doi.org/10.1161/CIRCIMAGING.116.004618
Pignatelli RH, McMahon CJ, Chung T, Vick GW 3rd (2003) Role of echocardiography versus MRI for the diagnosis of congenital heart disease. Curr Opin Cardiol 18(5):357–365
Krupickova S, Muthurangu V, Hughes M et al (2017) Echocardiographic arterial measurements in complex congenital diseases before bidirectional Glenn: comparison with cardiovascular magnetic resonance imaging. Eur Heart J Cardiovasc Imaging 18(3):332–341. https://doi.org/10.1093/ehjci/jew069
Losay J, Touchot A, Serraf A et al (2001) Late outcome after arterial switch operation for transposition of the great arteries. Circulation 104(12 Suppl 1):I121-6
Kilner PJ (2011) Imaging congenital heart disease in adults. Br J Radiol 84(3):S258–258. https://doi.org/10.1259/bjr/74240815
Safi LM, Bhatt AB (2017) Update on the management of adults with arterial switch procedure for transposition of the great arteries. Curr Treat Options Cardiovasc Med 19(1):4. https://doi.org/10.1007/s11936-017-0505-y
Cohen MS, Eidem BW, Cetta F et al (2016) Multimodality imaging guidelines of patients with transposition of the great arteries: a report from the american society of echocardiography developed in collaboration with the society for cardiovascular magnetic resonance and the society of cardiovascular computed tomography. J Am Soc Echocardiogr 29(7):571–621. https://doi.org/10.1016/j.echo.2016.04.002
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Christopher R. Broda, Svetlana B. Shugh, Rohan B. Parikh, YunFei Wang, Tobias R. Schlingmann, and Cory V. Noel declare that they have no conflicts of interest.
Ethical Approval
This retrospective chart review study was approved by the IRB at Baylor College of Medicine. Due to the nature of the study, inclusion of patient data was exempt from a requirement of obtaining informed consent.
Research Involving Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Broda, C.R., Shugh, S.B., Parikh, R.B. et al. Post-operative Assessment of the Arterial Switch Operation: A Comparison of Magnetic Resonance Imaging and Echocardiography. Pediatr Cardiol 39, 1036–1041 (2018). https://doi.org/10.1007/s00246-018-1858-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-1858-z