Abstract
To analyze the role of sensitive cardiac troponin I (scTnI) and high-sensitive troponin T (hscTnT) in the determination of myocardial injury caused by volume and pressure load due to pulmonary hypertension (PH) and to investigate if these markers may be useful in the management of PH in childhood. Twenty-eight patients with congenital heart disease (CHD) with left to right shunt and PH, 29 patients with CHD with left to right shunt but without PH, and 18 healthy children, in total 75 individuals, were included in the study. All cases were aged between 4 and 36 months. Echocardiographic evaluation was performed in all cases, and invasive hemodynamic investigation was performed in 33 cases. Blood samples were obtained from all cases, for the measurement of brain natriuretic peptide (BNP), pro-brain natriuretic peptide (pro-BNP), sensitive cardiac troponin I (scTnI), and high-sensitive troponin T (hscTnT) levels. The mean BNP, pro-BNP, scTnI, and hsTnT levels were statistically significantly higher in patients with PH than in the patients without PH (p < 0.001). A statistically significant positive correlation was determined between pulmonary artery systolic pressure and scTnI and hscTnT levels (r = 0.34 p = 0.01, r = 0.46 p < 0.001, respectively) levels. Pulmonary hypertension determined in congenital heart diseases triggers myocardial damage independently of increased volume or pressure load and resistance, occurring by disrupting the perfusion via increasing ventricular wall tension and the myocardial oxygen requirement. Serum scTnI and hscTnT levels may be helpful markers to determine the damage associated with PH in childhood.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital heart diseases (CHDs) with left to right shunt are the main causes of pulmonary hypertension (PH) in childhood [1, 2]. The defects associated with left to right shunt, if untreated, result in irreversible alterations in the pulmonary vascular bed, which is called pulmonary vascular obstructive disease [2]. At this stage, surgical correction is impossible. Hence, the most essential point in the treatment of pulmonary arterial hypertension that has developed as a result of CHD is the timing of surgery [3, 4]. Although right heart catheterization is the gold standard test determining PH, it is not convenient for screening, as it is an invasive technique [5]. Transthoracic echocardiography is a non-invasive and more practical way of diagnosing PH, but it is less sensitive and specific than catheterization [6]. Moreover, recently, some biomarkers have been defined relevant for the diagnosis and follow-up of pulmonary hypertension, including brain natriuretic peptide (BNP), uric acid, troponin T, carcinoembryonic antigen 125, and intercellular adhesion molecule-1 [7,8,9,10,11].
Cardiac troponins are the most sensitive and specific biochemical markers of cardiac muscle injury and especially of acute coronary syndrome and acute myocardial infarction [12]. CHDs with large left to right shunts, according to their anatomical locations, may result in an augmentation of right or left ventricular volume load, as well as a rise in right ventricular pressure by increasing pulmonary arterial pressure [13]. Increased pressure and/or volume load results in myocardial injury. In recent years, some newly developed and sensitive methods for the determination of cardiac troponins have been suggested to be useful in the evaluation of myocardial injury in children with congenital heart diseases [14,15,16]. Only a few studies have been performed with sensitive cardiac troponin I (scTnI) in children and, to the best of our knowledge, none with high-sensitive troponin T (hsTnT).
The aim of this study was to analyze the role of scTnI and hsTnT in the determination of myocardial injury caused by hemodynamic load due to PH secondary to left to right shunt and to investigate if these markers may be used in PH management in childhood.
Methods
Between January 2013 and January 2015, a study was conducted with a total of 75 children: 28 patients with mean pulmonary arterial pressure ≥ 25 mmHg in catheter angiography and/or tricuspid insufficiency (TI) flow rate ≥ 2.8 m/s in echocardiography, together with the presence of at least two echocardiographic findings of PH; 29 patients with CHD with left to right shunt without PH who were under follow-up in the Pediatric Cardiology Department; and 18 healthy controls drawn from children who attended the Pediatric Cardiology Department with suspected heart cardiac murmur but were found to have no detectable cardiac pathology. For the standardization of the study, only patients with moderate and/or large post-tricuspid shunts such as a ventricular septal defect (VSD) and patent ductus arteriosus (PDA) were included. Since serum cardiac troponin and brain natriuretic peptide (BNP) levels may be high in the first three months of life, only infants or children aged between 4 and 36 months were included in the study [17, 18]. The gender, diagnoses, diagnosis dates, symptoms, and treatments of the cases were analyzed. Detailed physical examination was performed in all cases, together with evaluation of the patients’ telecardiograms and electrocardiograms (ECGs). Cardiac catheterization and angiography were required in only 33 (22 with PH and 11 without PH) patients. Hemodynamic data were obtained during the procedures.
Blood samples were obtained for BNP, pro-brain natriuretic peptide (pro-BNP), scTnI, and hsTnT. Patients with acute infections, diabetes mellitus, sepsis, or renal failure, patients under cardiotoxic medication, or patients with a history of cardiac operations, were not included in the study, since cardiac troponin levels may be affected in these circumstances.
Transthoracic Echocardiography
Echocardiography was performed using Philips iE33 xMATRIX (Amsterdam, Netherlands) echocardiography with the aid of 3.5 MHz probes. Images were obtained in subcostal, parasternal long axis, short axis, apical four-chamber view, five spaces, and suprasternal positions, and M-mod, two-dimensional, and Doppler echocardiographic investigations were performed. Tricuspid insufficiency (TI) velocity obtained by Doppler echocardiography was evaluated in many windows. The window with the best imaging for TI envelope borders and maximum velocity was used in measurements. Using the Bernoulli equation, right ventricle systolic pressure was calculated from the TI flow. Systolic pulmonary artery pressure (sPAP) was determined by the addition of right atrium pressure (5 mmHg) with the obtained value. Patients with a TI flow rate of ≥ 2.8 m/s were regarded as having pulmonary hypertension [19].
Catheter Angiography
In the angiography procedure, after local anesthesia with lidocaine and premedication with 0.1 mg/kg intravenous midazolam, the femoral vein and artery were catheterized percutaneously. The pressures of right atrium, right ventricle, and left atrium were measured by using 5,6,7 NIH catheters (Cordis Corporation, Miami, USA) by age group and the pressure of pulmonary capillary wedge was measured by using 5 and 6 F multipurpose catheters. The measurements of pressures were obtained using fluid-filled catheters which were balanced with the zero level at the midaxillary line and connected to pressure transducers. The pulmonary and systemic blood flows were calculated by the Fick equation using the measured oxygen consumption and oxygen content derived from oxygen saturation.
The pulmonary vascular resistance was calculated from the equation of the ratio, difference between mean pulmonary arterial pressure and left atrial pressure or pulmonary arterial capillary wedge pressure to pulmonary blood flow.
The systemic vascular resistance was calculated as the ratio of the difference between mean arterial pressure and right atrium pressure to systemic blood flow.
Cardiac Troponin Levels
For the determination of hsTnT, blood samples obtained from peripheral veins were analyzed with a new third-generation quantitative electrochemiluminescence immunoassay method using Elecys 2010 (Roche Diagnostics, Mannheim, Germany). This method is specific for troponin T with an analytical range of 3–10,000 ng/L. The upper reference limit for hscTnT (99 percentile, CV < 10%) is 14 ng/L (pg/mL) [20, 21].
Serum scTnI levels were studied by the first-generation immunometric immunoassay method using Ortho Vitros ECi/ES (Johnson & Johnson, Buckinghamshire, UK). In this evaluation, the minimum quantifiable value is 0.012 ng/mL with an upper reference limit (99 percentile, CV < 10%) of 0.034 ng/mL [22, 23].
Statistical Analysis
The data were recorded with the Statistical Package for the Social Sciences program version 21 (SPSS, SPSS, Inc., Chicago, IL, USA). The distributions of continuous variables were analyzed with the Shapiro–Wilk test. The descriptive statistics were defined as mean ± standard deviation for normally distributing data and as median (minimum–maximum) for non-normally distributing data. The significance of the differences in mean values between two independent groups was analyzed with the Student t test, and the differences in mean values between more than two independent groups were analyzed with one-way variance analysis (ANOVA). If the result of one-way variance analysis proved to be significant, the condition causing this difference was determined with the post-hoc Tukey test. The significance of the differences in median values between two independent groups was analyzed with the Mann–Whitney U test, and the differences in median values between more than two independent groups were analyzed with the Kruskal–Wallis test. If the result of the Kruskal–Wallis test proved to be significant, the condition causing this difference was determined by Conover's non-parametric multiple comparison tests. For the determination of the sensitivity, specificity, and positive and negative predictive value of biomarkers, receiver operating characteristics (ROC) curve analysis was performed. p < 0.05 was regarded as statistically significant.
Ethical Considerations
The study protocol was approved by the ethics committee of University of Health Sciences, Keçiören Training and Research Hospital (number: 02.06.2010/004) and performed in accordance with the Declaration of Helsinki. Written informed consent was obtained in advance of the study from the parents of the study participants.
Results
Baseline Characteristics
Twenty-eight patients with CHD with left to right shunt causing PH, 29 patients having CHD with left to right shunt but without PH, and 18 healthy children, a total of 75 cases, were included in the study, which was conducted between January 2013 and January 2015.
Among the 28 patients with PH, 27 had a VSD and 1 had PDA. Among the 29 patients without PH, 23 had a VSD and six had PDA. Participants’ ages ranged between 4 and 36 months. There was no statistically significant difference between CHD groups with PH (PH group) or without PH (non-PH group) in terms of age or gender (p = 0.08, p = 0.6). Fatigue, weight loss, and frequent infections were reported in 22 (78.6%) of the PH group and in six patients (20.7%) in the non-PH group. At admission, 21 (75%) patients in the PH group and 18 (65.5%) patients in the non-PH group were receiving at least one of the diuretic and/or angiotensin converting enzyme inhibitor treatments. The demographic and clinical data on the study participants are summarized in Table 1.
Hemodynamic Data Obtained by Catheter Angiography
Catheter angiography was performed in 22 patients of the PH group and in 11 patients of the non-PH group. Systemic and pulmonary flow ratio (Qp/Qs) mean value was higher in PH group than non-PH group (2.74 ± 1.18, 1.97 ± 0.71, respectively). But this difference was not statistically significant (p = 0.08). However, Qp/Qs values were higher than 1.5 in both patient groups indicated that defects size were moderate or large. Mean pulmonary arterial pressure (mPAP), Qp (pulmonary flow), Rp (pulmonary resistance), Pp/Ps (pulmonary pressure, systemic pressure ratio), and Rp/Rs (pulmonary resistance, systemic resistance ratio) values were determined to be statistically significantly different in the PH group from the non-PH group (p < 0.001, p = 0.02, p = 0.03, p < 0.001, p = 0.002, respectively).
Correlation of Hemodynamic Data with Biochemical Marker Levels
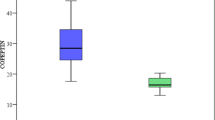
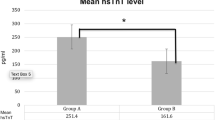
scTnI, hscTnT, BNP, and pro-BNP levels were determined to be higher in the PH group (Fig. 1). There was a statistically significant difference between groups regarding BNP, pro-BNP, scTnI, and hscTnT levels (p < 0.01). For all markers, the difference was created by the PH group. Among hemodynamic parameters obtained by catheter, Qp and Qp/Qs (pulmonary flow, systemic flow ratio) values were found to have a positive correlation with all biochemical parameters. Whereas the mPAP values were correlated with BNP, pro-BNP, and hscTnT, no correlation with scTnI was found (Table 2).
Correlation of Pulmonary Artery Systolic Pressures with Biochemical Marker Levels
Pulmonary artery systolic pressure values obtained by echocardiography were correlated with all biochemical markers. (BNP r = 0.45, p = 0.001, pro-BNP r = 0.42 p = 0,001, scTnI r = 0.34 p = 0.01, hscTnT r = 0.46 p < 0.001).
Sensitivity of Biochemical Markers in the Prediction of Pulmonary Hypertension
The sensitivity and specificity of serum scTnI levels in the prediction of pulmonary hypertension were determined as 75 and 79%, respectively. The cutoff value for scTnI in the prediction of PH was found to be 0.0125 ng/L (Fig. 1: area under the curve: 0.866, 95% confidence interval 0.775–0.956).
The sensitivity and specificity of serum hscTnT levels in the prediction of pulmonary hypertension were determined as 78 and 80%, respectively. The cutoff value for hscTnT in the prediction of PH was found to be 11.9 ng/L (Fig. 1: area under the curve: 0.89, 95% CI 0.81–0.969).
In multivariance regression analysis, only scTnI and hscTnT levels were determined to be independent biomarkers in the prediction of PH. According to this analysis, in patients with CHD having higher serum scTnI and hscTnT levels, there is an increased probability of the presence of pulmonary hypertension (odds ratio 1.15; 95% CI 1.02–1.29; p = 0.02, odds ratio 1.36; 95% CI 1.1–1.68; p = 0.004, respectively).
Discussion
In the diagnosis, follow-up, and treatment of patients with PH in the pediatric age group, the advice and the criteria adopted for adult PH patients are usually followed, owing to the lack of research with pediatric PH patients. In recent years, many biomarkers have been identified that may be helpful, especially in the follow-up of PH patients [7,8,9,10,11]. The role of these biomarkers in the follow-up of pulmonary arterial hypertension has attracted attention, but no consensus on this matter has yet been achieved.
Among these biomarkers, natriuretic peptides, synthesized from cardiac myositis with the increased wall tension due to the left to right shunt, are especially useful in the diagnosis and follow-up of heart failure. In different studies, BNP and pro-BNP levels were found to rise [24, 25] with an increase in the left to right shunt level. Many studies performed on adults have investigated the effects of increased BNP levels in the determination of pulmonary hypertension severity and life expectancy [26,27,28]. However, studies in the pediatric age group are few. In a study by Takatsuki et al. on 88 children with PH, a positive correlation was reported between BNP and pro-BNP levels and Pp/Ps, mean right atrium pressure, and TI [29]. Both BNP and pro-BNP were found to be effective in defining clinical and hemodynamic alterations in pediatric PH cases, and pro-BNP in particular was reported to be more significantly correlated with echocardiographic findings. In another study performed on 78 patients with childhood PH, although there was no strong correlation between the BNP levels at admission and echocardiographic and hemodynamic findings, there was a strong correlation between alterations of echocardiographic and hemodynamic parameters and BNP measurements in time [30].
In the present study on children with CHD, 28 with PH and 29 without PH, serum BNP and pro-BNP levels were determined to be higher than in the healthy controls. There was a high positive correlation between both markers (r = 0.94, p < 0.001). There was a statistically significant positive correlation between BNP and pro-BNP levels and hemodynamically measured Qp, Qp/Qs, and mPAP values. Moreover, there was a positive correlation between systolic pulmonary arterial pressure and both biochemical markers. In the light of these data, we believe that serum BNP and pro-BNP levels are valuable markers for reflecting increased wall tension due to increased pulmonary flow and in the prediction of increased pulmonary arterial pressure.
Whereas pre-tricuspid shunts mainly result in volume load, post-tricuspid shunts generally cause both volume and pressure loads [31]. The right ventricle especially, being thinner and more flexible, is forced to resist the afterload mismatch caused by increased pulmonary flow and consequently increased pulmonary resistance. In order to increase the right heart flow, right ventricle dilatation takes place. As specified in Laplace’s law, all these alterations result in an increase in thickness of the right ventricular wall at the same time. In previous studies, it was reported that both ventricular hypertrophy and tension on the ventricular wall due to left to right shunts disrupt the myocardial perfusion [32, 33]. Moreover, increased intra-wall pressure due to the tension also disrupts the coronary perfusion [34]. As a result of all these alterations, the left to right shunt due to CHD and increased pulmonary flow results in myocardial ischemia. Besides, with the development of new-generation sensitive cardiac troponins, the determination of cardiac troponin levels at much lower serum concentrations is possible [35, 36]. This condition enables the early diagnosis of myocardial injury, as well as the usage of cardiac troponins in conditions other than acute coronary syndromes, such as CHD with left to right shunts having partial myocyte injury [37,38,39].
Sugimoto et al. investigated the scTnI levels in children with atrial septal defect (ASD) and VSD and reported that the levels were higher in children with VSD. They found that scTnI levels were associated with the pulmonary pressure/systemic pressure ratio measured hemodynamically. In the present study, significant volume and pressure load was determined to cause myocardial damage independently of the resistance [40]. In a study by Eerola et al. performed with children, patients were divided into two groups: those with pressure load, such as with aortic coarctation or aortic and pulmonary valve stenosis, and those with volume load, such as with ASD or PDA. In patients with pressure load, cardiac Troponin I levels were determined to be statistically significantly higher [41].
In our patients, both scTnI and hscTnT levels were statistically significantly higher in the PH group compared with the healthy control cases and CHD cases with normal pulmonary artery pressure (the non-PH group) (p < 0.05). mPAP values determined with angiography were only correlated with hscTnT, while the sPAP value obtained with echocardiography was correlated with both scTnI and hscTnT. Moreover, there was a positive correlation between cardiac troponins and hemodynamically determined Qp and Qp/Qs values. This suggests that increased pulmonary blood flow may cause myocardial damage without any increase in pulmonary resistance.
In our study, in all the patient groups, hscTnT was at measurable levels, and in 25 patients it was high (14 ng/L or higher). Twenty (80%) patients with elevated hscTnT levels were in the PH group. During the study, two patients who died after surgery had also had elevated hscTnT levels. There was a high positive correlation also between scTnI and hscTnT levels (r = 0.71, p < 0.001). However, in PH patients, hscTnT levels, compared with scTnI, were determined to be statistically more significantly associated with PH. In logistic regression analysis, although both parameters were defined to be valuable for the prediction of PH, hscTnT was observed to be statistically more sensitive for the purpose (scTnI odds ratio 1.15; 95% CI 1.02–1.29; p = 0.02, hscTnT odds ratio 1.36; 95% CI 1.1–1.68; p = 0.004). The main cause of this condition may be the measurement of hscTnT with a more sensitive third-generation method compared with the first-generation method of scTnI.
There is a limited number of studies in the literature comparing the sensitivity of cardiac troponins with B-type natriuretic peptides in the determination of PH in childhood.
In a study on adults conducted by Filush et al., the hscTnT level was investigated in order to define its importance in the functional and prognostic evaluation of patients with PH; positive correlations between hsTnT levels and right ventricular systolic strain (r = 0.95, p = 0.0018) and strain rate (r = 0.82, p = 0.0021) were found in 55 patients with PH [42]. Moreover, it was suggested that hsTnT may identify World Health Organization functional class II and higher classes better than pro-BNP or heart fatty acid binding protein.
Sugimoto et al. also found a strong positive correlation between cTnI and pro-BNP values (r = 0.728; p < 0.001), and myocardial damage was suggested to be associated with advanced congestive heart failure due to increased pressure and volume load [40].
In the present study, there was a positive correlation between hscTnT levels and both BNP and pro-BNP (r = 0.51, p < 0.01; r = 0.45, p < 0.01, respectively) levels. However, there was no statistically significant association between scTnI and BNP or pro-BNP levels.
In all hscTnT measurements, the manufacturer is the same, the same calibrator and similar antibodies are in use, and thus there is no problem with the standardization of the method. However, many methods have been developed for the measurement of cTnI. Since the target regions may differ in different methods, the results may change by an order of 40–60 times [43,44,45]. Thus, the absence of standardization for scTnI produces significant confusion. We believe that the variance between the results obtained in this study for scTnI and those of other studies in the literature may be due to differences in the methods used.
This study is important, since it is one of only a few studies performed in the pediatric age group. Moreover, to the best of our knowledge, it is the first study to evaluate hscTnT levels in PH associated with CHD.
Study Limitations
The present study has some limitations. The most important limitation of this study is that baseline evaluation and classification of the patient groups were made according to clinical assessment and echocardiographic findings. Hemodynamic data could be obtained only in 57 patients. As this was a single-center study, the number of cases was very small, although sufficient to perform multivariate analysis. Also, follow-up information on the patients would have improved the study. Further studies should be performed with a larger number of subjects from multiple centers.
Conclusion
PH in CHDs triggers myocardial damage independently of increased volume or pressure load and resistance, disrupting the perfusion via increasing ventricular wall tension and the myocardial oxygen requirement. Serum scTnI and hscTnT levels are helpful markers to determine the damage associated with PH.
In the light of our results, we suggest that, in the management of childhood PH, determination of high-risk groups, identifying damage earlier, and taking precautions, assessment with sensitive cardiac troponins may be helpful.
References
Olguntürk R (2010) Pediatric pulmonary hypertension and pulmonary arterial hypertension secondary to congenital heart diseases. Anadol Kardiyol Derg 10:50–56
Lammers AE, Apitz C, Zartner P, Hager A, Dubowy KO, Hansmann G (2016) Diagnostics, monitoring and outpatient care in children with suspected pulmonary hypertension/paediatric pulmonary hypertensive vascular disease. Expert consensus statement on the diagnosis and treatment of paediatric pulmonary hypertension. The European Paediatric Pulmonary Vascular Disease Network, endorsed by ISHLT and DGPK. Heart 102:1–13
Haworth SG (2006) The management of children with congenital heart disease. Pulmonary Arterial Hypertension Related to Congenital Heart Disease 1st ed. London
Joshi R, Kalra R, Kumar N, Aggarwal N (2016) Critical decision of operability in congenital heart disease patient with severe pulmonary hypertension. Ann Card Anaesth 19:744
Apitz C, Hansmann G, Schranz D (2016) Hemodynamic assessment and acute pulmonary vasoreactivity testing in the evaluation of children with pulmonary vascular disease. Expert consensus statement on the diagnosis and treatment of paediatric pulmonary hypertension. The European Paediatric Pulmonary Vascular Disease Network, endorsed by ISHLT and DGPK. Heart 102:23–29
Hoeper MM, Lee SH, Voswinckel R, Palazzini M, Jais X, Marinelli A (2006) Complications of right heart catheterization procedures in patients with pulmonary hypertension in experienced centers. J Am Coll Cardiol 48:2546–2552
Pattathu J, Gorenflo M, Hilgendorff A, Koskenvuo JW, Apitz C, Hansmann G, Alastalo TP (2016) Genetic testing and blood biomarkers in paediatric pulmonary hypertension. Expert consensus statement on the diagnosis and treatment of paediatric pulmonary hypertension. The European Paediatric Pulmonary Vascular Disease Network, endorsed by ISHLT and DGPK. Heart 102:36–41
Pezzuto B, Badagliacca R, Poscia R, Ghio S, D’Alto M, Vitulo P, Mulè M, Albera C, Volterrani M, Fedele F, Vizza CD (2015 Mar) Circulating biomarkers in pulmonary arterial hypertension: update and future direction. J Heart Lung Transplant 34:282–305
Yilmaz MB, Zorlu A, Dogan OT, Karahan O, Tandogan I, Akkurt I (2011) Role of CA-125 in identification of right ventricular failure in chronic obstructive pulmonary disease. Clin Cardiol 34:244–248
Oguz MM, Oguz AD, Sanli C, Cevik A (2014) Serum levels of soluble ICAM-1 in children with pulmonary artery hypertension. Tex Heart Inst J 4:159–164
Yıldırım A, Güzelmeriç F, Öner CN, Karaağaç AT, Şaşmazel A, Erdem H, Özdemir O, Baysal A (2014) Prognostic significance of sICAM-1 and sVCAM-1 molecules for cardiac surgery in pediatric patients with pulmonary hypertension. Anadolu Kardiyol Derg 14:274–279
Garg P, Morris P, Fazlanie AL, Vijayan S, Dancso B, Dastidar AG, Plein S, Mueller C, Haaf P (2017) Cardiac biomarkers of acute coronary syndrome: from history to high-sensitivity cardiac troponin. Intern Emerg Med 12:147–155
Hafez MO, Morsy SM, Mahfoz RA, Ali AR (2015) Myocardial injury in children with unoperated congenital heart diseases. Cardiol Res Pract. https://doi.org/10.1155/2015/104818
Torbicki A, Kurzyna M, Kuca P, Fijałkowska A, Sikora J, Florczyk M et al (2003) Detectable serum cardiac troponin T as a marker of poor prognosis among patients with chronic precapillary pulmonary hypertension. Circulation 108:844–848
Antman EM (2002) Decision making with cardiac troponin tests. N Engl J Med 346:2079–2082
Mair J (2014) High-sensitivity cardiac troponins in everyday clinical practice. World J Cardiol 6:175–182
Kunii Y, Kamada M, Ohtsuki S, Araki T, Kataoka K, Kageyama M et al (2003) Plasma brain natriuretic peptide and the evaluation of volume overload in infants and children with congenital heart disease. Acta Med Okayama 57(4):191–197
Bader D, Kugelman A, Lanir A, Tamir A, Mula E, Riskin A (2006) Cardiac troponin I serum concentrations in newborns: a study and review of literature. Clin Chin Acta 371(1–2):61–65
Bossone E, D’Andrea A, D’Alto M, Citro R, Argiento P, Ferrara F et al (2013) Echocardiography in pulmonary arterial hypertension: from diagnosis to prognosis. J Am Soc Echocardiogr 26:1–14
Apple FS, Wu AHB, Jaffe AS (2002) European Society of Cardiology and American College of Cardiology guidelines for redefinition of myocardial infarction: how to use existing assays clinically and for clinical trials. Am Heart J 144:981–986
Apple FS, Wu AHB (2001) Myocardial infarction redefined: role of cardiac troponin testing. Clin Chem 47:377–379
Antman EM, Tanasijevic MJ, Thompson B et al (1996) Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Eng J Med 335:1342–1349
Venge P, Langerquist B, Diderholm E et al (2002) On behalf of the FRISC II Study Group. Clinical Performance of three cardiac troponin assays in patients with unstable coronary artery disease (FRISC II substudy). Am J Cardiol 89:1035–1041
Özhan H, Albayrak S, Uzun H,et al (2007) Correlation of plasma B Type natriuretic peptide with shunt severity in patients with atrial or ventricular septal defect. Pediatr Cardiol 28:272–275
Holmström H, Hall C, Thaulow E (2001) Plasma levels of natriuretic peptides and hemodynamic assessment of patent ductus arteriosus in preterm infants. Acta Paediatr 90:184–191
Leuchte HH, Holzapfel M, Baumgartner RA et al (2005) Characterization of brain natriuretic peptide in long-term follow-up of pulmonary arterial hypertension. Chest 128:2368–2374
Fijalkowska A, Kurzyna M, Torbicki A et al (2006) Serum N-terminal brain natriuretic peptide as a prognostic parameter in patients with pulmonary hypertension. Chest 129:1313–1321
Conen D, Pfisterer M, Martina B (2006) Substantial intraindividual variability of BNP concentrations in patients with hypertension. J Hum Hypertens 20:387–391
Takatsuki S, Wagner BD, Ivy D (2012) B-type natriuretic peptide and amino-terminal pro-B-type natriuretic peptide in pediatric patients with pulmonary arterial hypertension. Congenit Heart Dis 7(3):259–267
Bernus A, Wagner BD, Accurso F et al. (2009) Brain natriuretic peptide levels in managing pediatric patients with pulmonary arterial hypertension. Chest 135(3):745–751
Galie N, Manes A, Palazzini M et al (2008) Management of pulmonary arterial hypertension associated with congenital systemic-to-pulmonary shunts and Eisenmenger’s syndrome. Drugs 68:1049–1066
Kubo T, Kitaoka H, Okawa M et al (2010) Serum cardiac troponin I is related to increased left ventricular wall thickness, left ventricular dysfunction, and male gender in hypertrophic cardiomyopathy. Clin Cardiol 33:E1–E7
Petersen SE, Jerosch-Herold M, Hudsmith LE et al (2007) Evidence for microvascular dysfunction in hypertrophic cardiomyopathy: new insights from multiparametric magnetic resonance imaging. Circulation 115:2418–2425
Galderisi M (2007) Epicardial coronary vessels and coronary microcirculation in pressure overload hypertrophy: a complex interaction. Am J Hypertens 20:285–286.
Apple FS (2009) A new season for cardiac troponin assays: it’s time to keep a scorecard. Clin Chem 55:7 1303–1306
Xu RY, Zhu XF, Yang Y, Ye P (2013) High-sensitive cardiac troponin T. J Geriatr Cardiol 10:102–109
Colvin KL, Dufva MJ, Delaney RP, Ivy DD, Stenmark KR, Yeager M (2014) Biomarkers for pediatric pulmonary arterial hypertension—a call to collaborate. Front Pediatr 2:1–12
Zelniker T, Uhlmann L, Spaich S, Friedrich J, Preusch MR, Meyer FJ et al. (2015) Novel biomarkers for risk stratification in pulmonary arterial hypertension. ERJ Open Res 1:00008-2015
Eggers KM, Lindahl B (2017) Application of cardiac troponin in cardiovascular diseases other than acute coronary syndrome. Clin Chem 63:223–235
Sugimoto M, Ota K, Kajihama A, Nakau K et al (2011) Volume overload and pressure overload due to left-to-right shunt- induced myocardial injury: evaluation using a highly sensitive cardiac troponin I assay in children with congenital heart disease. Circ J 75:2213–2219
Eerola A, Jokinen EO, Savukoski TI et al (2013) Cardiac troponin I in congenital heart defects with pressure or volume overload. Scand Cardiovasc J 47:154–159
Filusch A, Giannitsis E, Katus HA, Meyer FJ (2010) High-sensitive troponin T: a novel biomarker for prognosis and disease severity in patients with pulmonary arterial hypertension. Clin Sci 119:207–213
Apple FS (1999) Clinical and analytical standardization ıssues confronting cardiac troponin I. Clin Chem 45(1):18–20
Labugger R, Organ L, Collier C et al (2000) Extensive troponin I and T modification detected in serum from patients with acute myocardial infarction. Circulation 102:1221–1226
Tate JR, Heathcote D, Rayfield J, Hickman PE (1999) The lack of standardization of cardiac troponin I assay systems. Clin Chim Acta 284:141–149
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Rights and permissions
About this article
Cite this article
Kayali, S., Ertugrul, I., Yoldas, T. et al. Sensitive Cardiac Troponins: Could They Be New Biomarkers in Pediatric Pulmonary Hypertension Due to Congenital Heart Disease?. Pediatr Cardiol 39, 718–725 (2018). https://doi.org/10.1007/s00246-018-1811-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-1811-1