Abstract
The objective of this study was to describe a contemporary cohort of pediatric patients hospitalized for clinically suspected myocarditis. A retrospective chart review was performed at seven tertiary pediatric hospitals. Electronic medical records were searched between 2008 and 2012 for patients ≤18 years admitted with an ICD-9 code consistent with myocarditis. Patients were excluded if the admitting or consulting cardiologist did not suspect myocarditis during the admission or an alternative diagnosis was determined. One hundred seventy-one patients were discharged or died with a primary diagnosis of myocarditis. Median age was 13.1 years (IQR 2.1, 15.9), with a bimodal distribution; 24% <2 years and 46% between 13 and 18 years. Patients with moderate or severe systolic dysfunction were younger, had higher BNPs at admission, but had lower troponin. Mortality, heart transplantation, and readmission did not differ between patients who received only IVIG, only steroids, IVIG and steroids, and no immunotherapy. Ninety-four patients (55%) were discharged on heart failure medications, 16 were transplanted, and seven died. The presence at the time of admission of gastrointestinal (GI) symptoms (p = 0.01) and lower echo shortening fraction (SF) (p < 0.01) was associated with death/transplant. Within one year 16% had a readmission, one underwent heart transplant, and 39% received heart failure therapy. Pediatric myocarditis has a bimodal age distribution. The use of IVIG and steroids is not associated with mortality/heart transplantation. The presence of GI symptoms and lower echo SF may identify patients at risk for death and/or transplantation during the admission.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An analysis of the pediatric health information system (PHIS) utilizing ICD-9 coding showed myocarditis that accounts for approximately 0.05% of all pediatric admissions to tertiary care hospitals [1]. Despite its rarity, myocarditis is a significant etiology of acute and chronic heart failure, often leading to dilated cardiomyopathy and need for heart transplantation [2].
While the classical myocarditis patient presents with a preceding viral illness followed by heart failure symptoms, clinical presentations range from mild chest pain with normal systolic function to cardiogenic shock and electrophysiological disturbances [3,4,5]. In the recent era, the role of diagnostic criteria including endomyocardial biopsy (EMBx), cardiac magnetic resonance imaging (MRI), and laboratory findings are evolving and remain controversial. Given the wide range of clinical presentations and lack of a uniform gold-standard diagnostic modality, pediatric cardiologists are often left with a difficult task of making a clinical diagnosis of myocarditis.
Previous studies in pediatric myocarditis have been small cohort single center institutional reviews or large multi-center database analyses [6, 7]. Single center reviews have provided important information; however, the small number of patients limit further statistical analysis and may not represent the experience of the community. In contrast, multi-center databases are often missing specific valuable data that can also limit further analysis [7]. Also, previous studies restricting the diagnosis to those confirmed by gold-standard techniques exclude multiple patients with suspected myocarditis and do not reflect clinical practice. The aim of this study was to perform a large multi-institutional retrospective review of inpatient pediatric myocarditis in order to compare clinical signs and symptoms, diagnostic tests, therapeutics, short-term outcomes, and risk factors for poor outcomes.
Methods
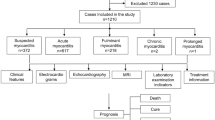
Medical records at seven tertiary care children’s hospitals were searched for inpatient admissions with ICD-9 codes consistent with myocarditis between the years of 2008–2012. Patients were included if they were admitted for suspected or confirmed myocarditis, ≤18 years of age, and did not have a previous diagnosis of myocarditis. Medical records were reviewed by each institution’s primary investigator and patients were excluded if the admitting or consulting cardiologist did not suspect myocarditis during the hospitalization or if another etiology of heart failure was identified. Outpatient and inpatient records were reviewed to obtain follow-up data for up to one year following initial hospitalization.
Institutional review board approval was obtained at each participating institution. Data were entered into Medical University of South Carolina’s Research Electronic Data Capture (REDCap®).
Data obtained from each patient’s chart included demographics, presenting signs and symptoms, diagnostic tests, therapeutics, and short-term outcomes. Relevant heart failure laboratories at admission and peak values were recorded. The first complete echocardiogram during the admission was entered into the database. Recorded diagnostic tests included cardiac MRI, EMBx, as well as viral studies (PCR and titers) performed to identify the causative agent. Therapies recorded included heart failure medications, vasoactive or inotropic medications, mechanical ventilation or circulatory support, anti-arrhythmics, and immune modulators (IVIG, steroids). Outcome data included status at discharge (alive, transplanted, death), medications at discharge, and cardiac readmissions within 1 year.
Patients were stratified by degree of ventricular dysfunction and by the presence of confirmed myocardial inflammation. Ventricular dysfunction was defined as severe if ejection fraction (EF) was <30%, moderate if EF was 30–39%, mild if EF was 40–49%, and normal for 50% or higher. If EF was not calculated then shortening fraction (SF) was used, severe was defined as a SF <14, moderate if SF was 14–21%, mild if SF was 22–28%, and normal if SF was >28%. Confirmed myocardial inflammation was defined by a positive biopsy or MRI with gadolinium enhancement as defined by institutional standards.
Descriptive statistics were reported as median and interquartile range (IQR). Risk factor analysis began with univariate analysis to determine possible associations between covariates and the outcome of interest. Covariates that were associated with the outcome in univariate analysis (p ≤ 0.05) were then evaluated using a logistic regression model to determine independent associations. Comparison between groups of patients was performed using univariate non-parametric statistical tests.
Results
Patients
There were 212 patients who met study inclusion criteria. Of those 212, 41(19%) were found to have a diagnosis other than myocarditis prior to discharge. Therefore further analysis was performed on the 171 patients who were discharged or died with the primary diagnosis of myocarditis. Median age was 13.1 years (IQR 2.1, 15.9). There was a bimodal age distribution, with 24% of patients <2 years of age and 46% between 13 and 18 years (Fig. 1). Within this myocarditis cohort, 71 (42%) were female, 89 (52%) were Caucasian, 44 (26%) were African-American, 25 (15%) were Hispanic/Latino, and 13 (7%) were other.
Severity of Ventricular Dysfunction
Of the 171 patients, 164 patients had a recorded EF or SF at admission. In total there were 67 patients with normal ventricular function, 23 with mild ventricular dysfunction, 29 with moderate ventricular function, and 45 with severe ventricular function. Further analysis was performed by dichotomizing patients based upon degree of ventricular dysfunction (moderate–severe vs. mild–normal).
Patients with moderate to severe ventricular dysfunction were more likely to be younger, female, and present with symptoms of respiratory distress, GI symptoms (including nausea, emesis, diarrhea, or poor appetite), and malaise/fatigue (Table 1). Not surprisingly, physical findings of heart failure were more common in patients with worse ventricular function (Table 1). Patients with normal or mildly depressed ventricular function were more likely to present with chest pain.
Comparisons between degree of ventricular dysfunction and admission laboratories, diagnostic tests, immunotherapy administered, and hospital outcomes are summarized in Table 1. Of note patients with moderate–severe dysfunction who presented with lower admission troponin and higher BNP, were more likely to have positive biopsy and PCR. Patients with moderate–severe dysfunction were also more likely to receive IVIG or steroids, have a longer hospital stay and die, or be transplanted (Table 1). Patients admitted with moderate–severe ventricular dysfunction had a median discharge EF of 51 versus 61% for those with mild–normal function at admission (p = 0.01, Fig. 2).
Box plot of ejection fraction at time of discharge grouped by ventricular function at admission. Median ejection fraction for patients with moderate to severe ventricular dysfunction at admission had a median EF of 51% at discharge versus 61% for patients with mild dysfunction to normal function at admission
When evaluating only the 74 patients with moderate–severe ventricular dysfunction, only nine did not receive IVIG. Patients who received IVIG at admission did not differ from those who did not receive IVIG with regards to age at admission (p = 0.6), admission BNP (p = 0.34), SF at presentation (p = 0.8), frequency of hospital death (2/9 vs. 5/65, p = 0.2), transplantation (1/9 vs. 11/65, p = 1), and length of admission (11 vs. 16d, p = 0.16). Patients who received IVIG did not have different SF at discharge versus those who did not receive IVIG (29.9 vs. 23.6%, p = 0.42) or had different SF from admission to discharge (12.4 vs. 14.5%, p = 0.77).
Confirmed Myocarditis versus Clinically Diagnosed Myocarditis
Comparisons between patients with evidence of myocardial inflammation (+EMBx or MRI) versus those who had no evidence of inflammation or were unknown are summarized in Table 2. Patients with evidence of inflammation were more likely to receive IVIG and anti-arrhythmics, had a longer length of hospitalization, and more likely to be sent home on heart failure medication.
Of the 55 patients with confirmed myocarditis, 44 received IVIG. Differences between those who received IVIG and those who did not are shown in Table 3. Those who received IVIG were younger, had worse ventricular function, and longer hospital stay.
Poor Outcome and Readmission
Outcomes were assessed for the initial hospitalization. There were 149 cases of transplant-free survival to discharge (87%) and 22 cases (13%) of death/transplant. Of these 22 patients with poor outcomes in the initial hospitalization, 16 required transplantation (9%) and seven died (4%; 1 after transplant). Those with poor outcomes (death and/or transplant) were younger and more likely to be female (Table 4). Echocardiographic factors associated with poor outcome included higher LVEDd z-score at presentation.
The majority of patients who had transplant-free survival were discharged home on heart failure medications (95/149). Most common discharge medications were ACE inhibitors (72/149, 48%) followed by beta-blockers (32/149, 21%).
During the one year follow-up, twenty-three (16%) patients were readmitted for heart failure symptoms, with a total of 32 admissions. Those readmitted were more likely to be female (57 vs. 35%, p = 0.048) and had a longer initial length of stay (11 vs. 5 days, p = 0.03). Groups did not differ in the use of mechanical circulatory support, inotropes, or mechanical ventilation. There was no difference in the use of corticosteroids, IVIg, or other immunomodulatory therapy. Those who were readmitted were more likely to be discharged on heart failure medication (81 vs. 51%, p = 0.01) and followed by an identified heart failure specialist (65 vs. 34%, p < 0.01). However, SF at the time of initial discharge did not differ between readmission groups (p = 0.37). ACE inhibitors (69 vs. 42%, p = 0.01) were more commonly used in patients requiring readmission; beta-blockers (35 vs. 18%, p = 0.06) trended towards being utilized more frequently in readmitted patients.
Discussion
In this large multi-center study of clinically diagnosed pediatric myocarditis, clinical presentation and risk factors for poor outcomes, including readmission, death, and heart transplant were identified. The study demonstrates the heterogeneous clinical manifestations of myocarditis; however, 87% of pediatric myocarditis admissions survive to discharge without heart transplantation.
The use of clinically diagnosed myocarditis does lead to possible inclusion of patients who did not have myocarditis. However, less than half of the patients in our study underwent “gold standard” biopsy and/or MRI, highlighting the fact that current “gold standard” diagnostics are either clinically difficult to obtain or not are deemed useful. There were differences between patients with confirmed myocarditis versus clinical diagnosis, such as hospital stay and use of anti-arrhythmics. However, the two groups did not differ in risk for poor outcome or ventricular function at discharge. Restricting our inclusion criteria to only confirmed myocarditis by MRI or EMBx would not reflect actual clinical practice. “Real-World Evidence” that reflects clinical practice is receiving more emphasis from important institutions such as the FDA and NIH [8, 9]. Therefore, our study provides descriptive statistics and risk factors for poor outcomes that are easily applied to the clinical setting.
There was an observed bimodal age distribution to admissions for pediatric myocarditis. This trend has been reported in previous reports [7]. Patients with moderate–severe ventricular dysfunction were much younger than those with normal to mildly depressed ventricular function. The mechanistic relationship between age and severity of illness is not well understood. However, hormonal changes and age have been shown in mice models to affect infectivity of viral myocarditis agents and may thereby influence the clinical phenotype [10, 11]. It is also plausible that teenage patients are more likely to come to medical attention with their ability to articulate symptoms, where as younger patients are more reliant on caregiver observations therefore creating a selection bias. Interestingly, our data suggest that female gender was associated with worse ventricular function at admission, death/transplant during admission, and cardiac readmission within 1 year. Animal models have shown a gender difference in infectivity and immune system response in Coxsackie myocarditis; however, these studies have suggested worse outcomes for males [12]. Future clinical and biological research into pediatric myocarditis should explore the effect of age and gender on pathogenicity and treatment.
Though the majority of patients admitted with myocarditis had a favorable outcome, 13% still suffered from death or transplantation. Factors associated with poor outcomes included younger age, female gender, signs and symptoms of heart failure, and/or poor perfusion with worse ventricular function on echocardiogram. In adult myocarditis, worse clinical status and evidence of inflammation are associated with worse outcomes [13]. In our analysis, myocardial inflammation was not a risk factor for death/transplant, but it was associated with longer hospital stay. Of note, only 49% of our patients had an MRI and/or EMBx to assess for inflammation, therefore limiting our analysis of the effect of myocardial inflammation on outcome. Previous retrospective studies have found an association between the MRI findings of inflammation and poor outcomes [14].
Most patients survived till discharge with many discharged on oral heart failure medications. Previous adult myocarditis studies have displayed improved outcomes with beta blockade; however in this study, the use of heart failure medications and follow-up with pediatric heart failure specialists were associated with cardiac readmissions despite no difference in discharge echocardiograms [13]. These findings likely represent a selection bias of aggressive treatment and follow-up for high-risk patients but should be further assessed. Studies with longer follow-up should help determine any possible benefit to heart failure medications in patients after pediatric myocarditis.
In the mid 90s, Drucker et al. reported an improvement in ventricular function in pediatric myocarditis patients treated with IVIG [6]. This led to rapid adoption of IVIG in pediatric myocarditis; however, subsequent single center reviews and multi-center database analyses have not reproduced a benefit of IVIG7,15–18. IVIG use continues to be popular with approximately two-thirds of our study population receiving IVIG. Those who received IVIG and/or steroids showed no improvement in hospital mortality and shortening fraction at discharge or cardiac readmission within 1 year. While there was an increase in heart transplantation in those patients who received IVIG and/or steroids, this association is likely from a significant selection bias. Patients who received immunotherapy were more likely to be younger and have worse ventricular function at admission. In multivariable analysis, immunotherapy was not an independent risk factor for poor outcomes. Given the design of this study, the role that IVIG or other immunomodulators plays in pediatric myocarditis is still an area of future clinical research and will likely require a prospective study.
Limitations
While our study showed no association between IVIG and/or steroids with clinical outcomes, the high frequency in which IVIG and steroids were used and the low incidence of death, transplant, and cardiac readmissions may make robust statistical analysis more difficult to perform. The choice of who received IVIG or other immunomodulators may have included patient characteristics, laboratory findings, or clinician preference that were not collected in this study and therefore may introduce bias not accounted for. The follow-up time period for the cohort was relatively short. Future studies should be performed to assess associations between heart failure severity and heart failure medications.
Conclusion
Pediatric myocarditis is a disease that presents with multiple symptoms and has a bimodal age distribution. Overall survival for the index hospitalization is very good. The presence of worse ventricular function and GI symptoms may help identify patients at higher risk for death/transplant. IVIG and other immunomodulators were used frequently but their impact on outcomes remains unclear.
References
Klugman D, Berger JT, Sable CA, He J, Khandelwal SG, Slonim AD (2010) Pediatric patients hospitalized with myocarditis: a multi-institutional analysis. Pediatr Cardiol 31(2):222–228. doi:10.1007/s00246-009-9589-9
Savla J, Lin KY, Lefkowitz DS, Paridon SM, Gaynor JW, Hammond R, Shaddy RE, Rossano JW (2014) Adolescent age and heart transplantation outcomes in myocarditis or congenital heart disease. J Heart Lung Transplant 33(9):943–949. doi:10.1016/j.healun.2014.04.018
Batra AS, Epstein D, Silka MJ (2003) The clinical course of acquired complete heart block in children with acute myocarditis. Pediatr Cardiol 24(5):495–497. doi:10.1007/s00246-002-0402-2
Chang YJ, Chao HC, Hsia SH, Yan DC (2006) Myocarditis presenting as gastritis in children. Pediatr Emerg Care 22(6):439–440. doi:10.1097/01.pec.0000221346.64991.e7
Durani Y, Egan M, Baffa J, Selbst SM, Nager AL (2009) Pediatric myocarditis: presenting clinical characteristics. Am J Emerg Med 27(8):942–947. doi:10.1016/j.ajem.2008.07.032
Drucker NA, Colan SD, Lewis AB, Beiser AS, Wessel DL, Takahashi M, Baker AL, Perez-Atayde AR, Newburger JW (1994) Gamma-globulin treatment of acute myocarditis in the pediatric population. Circulation 89(1):252–257
Ghelani SJ, Spaeder MC, Pastor W, Spurney CF, Klugman D (2012) Demographics, trends, and outcomes in pediatric acute myocarditis in the United States, 2006 to 2011. Circ Cardiovasc Qual Outcomes 5(5):622–627. doi:10.1161/CIRCOUTCOMES.112.965749
FDA (2016) FDA Guidance: Use of Real-World Evidence to Support Regulatory Decision-Making for Medical Devices
Brief NI (2015) NEHI Issue Brief: Real World Evidence: A New Era for Health Care
Lyden D, Olszewski J, Huber S (1987) Variation in susceptibility of Balb/c mice to coxsackievirus group B type 3-induced myocarditis with age. Cell Immunol 105(2):332–339
Lyden DC, Olszewski J, Feran M, Job LP, Huber SA (1987) Coxsackievirus B-3-induced myocarditis. Effect of sex steroids on viremia and infectivity of cardiocytes. Am J Pathol 126(3):432–438
Fairweather D, Cooper LT Jr, Blauwet LA (2013) Sex and gender differences in myocarditis and dilated cardiomyopathy. Curr Probl Cardiol 38(1):7–46. doi:10.1016/j.cpcardiol.2012.07.003
Kindermann I, Kindermann M, Kandolf R, Klingel K, Bultmann B, Muller T, Lindinger A, Bohm M (2008) Predictors of outcome in patients with suspected myocarditis. Circulation 118(6):639–648. doi:10.1161/CIRCULATIONAHA.108.769489
Sachdeva S, Song X, Dham N, Heath DM, DeBiasi RL (2015) Analysis of clinical parameters and cardiac magnetic resonance imaging as predictors of outcome in pediatric myocarditis. Am J Cardiol 115(4):499–504. doi:10.1016/j.amjcard.2014.11.029
Acknowledgements
The authors would like to acknowledge Yuk Law, MD for his leadership and support of the study.
Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to report.
Informed Consents
Not obtained due to retrospective study design.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Butts, R.J., Boyle, G.J., Deshpande, S.R. et al. Characteristics of Clinically Diagnosed Pediatric Myocarditis in a Contemporary Multi-Center Cohort. Pediatr Cardiol 38, 1175–1182 (2017). https://doi.org/10.1007/s00246-017-1638-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-017-1638-1