Abstract
The optimal red blood cell transfusion threshold for postoperative pediatric cardiac surgery patients is unknown. This study describes the stated red blood cell transfusion practice of physicians who treat postoperative pediatric cardiac surgery patients in intensive care units. A scenario-based survey was sent to physicians involved in postoperative intensive care of pediatric cardiac surgery patients in all Canadian centers that perform such surgery. Respondents reported their red blood cell transfusion practice in four postoperative scenarios: acyanotic or cyanotic cardiac lesion, in a neonate or an infant. In part A of each scenario, the patient was critically ill, but stabilized; in part B, the patient became unstable. Response rate was 58 % (71 of 123), with 45 respondents indicating direct involvement in postoperative intensive care. There was a wide variability in stated transfusion threshold, ranging from <7.0–14.0 g/dL for stabilized cases. There was no significant difference between neonates and infants in stated transfusion threshold. The mean hemoglobin level below which respondents would transfuse a stabilized patient was 9 g/dL for acyanotic and 11.2 g/dL for cyanotic patients, a statistically significant difference (2.2 ± 0.9 g/dL, p < 0.001). All clinical determinants of instability significantly increased transfusion threshold. Hemodynamic instability increased transfusion threshold by 2.3 ± 1.3 g/dL in acyanotic patients and by 1.3 ± 1.1 g/dL in cyanotic patients. Cyanotic lesion and clinical instability, but not patient age, increased stated red blood cell transfusion threshold. Significant variation in reported red blood cell transfusion practice exists among physicians treating pediatric patients in intensive care following cardiac surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Red blood cell (RBC) transfusion is common in the care of pediatric cardiac surgery patients, with reported transfusion rates up to 79 and 55 % for surgery with and without bypass, respectively [1]. However, RBC transfusions are not without risk. Though transfusion-related infectious complications of RBC transfusions have decreased in recent years [2], significant non-infectious serious hazards of transfusion remain, including storage lesions and transfusion-related immunomodulation [2–4]. RBC transfusion in pediatric cardiac surgery patients has been associated with longer ventilation time, prolonged hospital stay and increased infections [5–7]. Furthermore, RBC transfusion is associated with increased morbidity and mortality in adults with cardiac disease [8–10]. Indeed, a restrictive RBC transfusion strategy was not inferior to a liberal strategy in clinical trials of critically ill adults [11], critically ill children [12], and critically ill children after cardiac surgery [13, 14]. Whether these studies have changed clinical practice is unknown.
Three scenario-based surveys have been published on stated transfusion practice in pediatric intensive care units (PICU); none specifically addressed cardiac patients [15–17]. We therefore surveyed physicians caring for postoperative cardiac surgery patients in PICU in order to describe stated RBC transfusion practice and the determinants that influence transfusion decision making.
Materials and Methods
Study Design
We developed a cross-sectional self-administered scenario-based survey. The questionnaire was designed to determine which patient, respondent, and center-related characteristics modulate the hemoglobin (Hb) concentration below which physicians prescribe a RBC transfusion.
Study Population
We aimed to contact physicians directly involved in the postoperative care of pediatric cardiac surgery patients in all seven pediatric cardiac surgery programs in Canada. Names and contact details of pediatric intensivists, cardiologists, and cardiac surgeons were obtained from websites of Stollery Children’s Hospital, Montreal Children’s Hospital, Centre Hospitalier Universitaire de Québec, Children’s Hospital of Eastern Ontario, British Columbia Children’s Hospital, Hospital for Sick Children and CHU Sainte-Justine. Each center was telephoned to confirm the information. Respondents were asked to indicate if they were directly involved in postoperative ICU care of pediatric cardiac surgery patients and if not, to return the survey blank.
Questionnaire Development
We asked 26 physicians at our center (cardiac surgeons, cardiologists, intensivists, and PICU fellows) to list all clinical and laboratory data that would prompt them to prescribe RBC transfusion in a postoperative cardiac surgery patient. Fourteen clinical and nine laboratory items were identified. Three authors (KH, JL, and NP) selected final items using the Delphi method. After two iterations, 11 possible determinants were retained: age, cyanotic cardiopathy, desaturation, pulmonary hypertension, hypotension, hypovolemia, increased inotropes, hyperlactatemia, decreased mixed venous saturation (SvO2), active bleeding, and extracorporeal membrane oxygenation (ECMO) support. A self-administered survey was constructed with four scenarios (Table 1 and see electronic supplementary material for all four scenarios) describing the postoperative condition of a neonate or infant with a cyanotic (palliated) or acyanotic (corrected) cardiac malformation. Mean Hb level and lower limit of normal by age group were provided as a reference. Part A of each scenario described a hemodynamically stable patient, who became unstable in part B. In each scenario, clinical determinants of stability were changed one at a time and respondents asked to indicate their Hb transfusion threshold. The survey also requested information on physician and PICU characteristics (Table 2).
Questionnaire Pretesting
Three PICU attending physicians, four PICU fellows, and one pediatric cardiac surgeon rated the final version of the questionnaire for discriminality, clarity, utility, face validity, content validity, construct validity, and absence of redundancy [18] using a 7-point Likert scale ranging from one (complete disagreement) to seven (complete agreement). Responses between five and seven were considered satisfactory. The respondents considered 84 % of questions satisfactory, with a mean Likert score of 5.6 for all quality criteria.
Questionnaire Administration
The survey was distributed according to the principles of Dillman et al. [19]. It was mailed in June 2009; reminders with survey attached were sent 3 and 4 months after the first mailing.
Statistics
Three variable categories were considered possible determinants of RBC transfusion in critically ill children: disease (scenarios), clinical patient characteristics, and characteristics of respondents and ICUs.
First, baseline mean and standard deviation (SD) of stated transfusion threshold were calculated for each scenario. Second, the effect of each respondent’s characteristic on baseline Hb was analyzed separately, using two-way ANOVA with scenarios and respondent characteristics as independent variables. Third, changes from baseline transfusion threshold were calculated for each determinant by scenario and compared to uncover statistically significant changes between determinants. The effect of scenarios 1–4 on baseline transfusion threshold was assessed by one-way ANOVA. The effect of determinants on differences between baseline Hb transfusion threshold in each scenario and determinant-defined transfusion threshold was evaluated by two-way ANOVA. Significant interactions between scenarios and determinants were explored: Thus, one-way ANOVAs (factor = scenario) were performed for each determinant to estimate the effect of scenarios and likewise, one-way ANOVAs (factor = determinants) were carried out for each scenario to estimate the effect of determinants. The latter analysis compared the mean change associated with each determinant for each scenario separately. Pairwise comparisons between determinants were carried out, and a Tukey’s HSD post hoc test was used to account for multiplicity. Analyses were done by a statistician (Thierry Ducruet) with SAS program (v. 9.3, SAS Institute Inc., Cary, NC).
Results
The survey was sent to 123 physicians; 71 responded (58 %), of whom 45 (63 %) indicated direct involvement in postoperative cardiac surgery ICU care. Only 17 responses were missing (17/2520 = 0.7 %) in the surveys that we received; most unanswered questions were about physician age (6 of 17 unanswered questions) and number of PICU beds (5 of 17).
Physician and PICU characteristics are described in Table 2. Average age of respondents was 43 ± 9 years. Pediatrics was the primary specialty for 32 of 45 (71 %). Most (62 %) had ten or more years of practice as attending physician. Average number of PICU beds was 16 ± 5.9. 73 % of respondents stated their institution performed 0–200 operations per year using cardiopulmonary bypass (CPB). 18 of 45 physicians answered that 26–50 % of cardiac surgeries were performed on patients aged under 30 days.
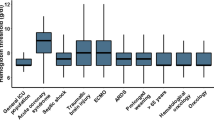
Figure 1 reports the number of times each Hb transfusion threshold was chosen in the four hemodynamically stable scenarios. For neonates, the average Hb transfusion threshold for an acyanotic patient (arterial switch) was 9.2 ± 1.3 g/dL and was 11.3 ± 1.6 g/dL for a cyanotic patient (systemic-pulmonary shunt for tetralogy of Fallot with pulmonary atresia). For infant cases, the mean Hb transfusion threshold was 8.8 ± 1.3 g/dL for an acyanotic patient (corrective surgery for complete atrioventricular canal) and 11.1 ± 1.4 g/dL for a cyanotic patient (stage 2 cavopulmonary shunt palliation for hypoplastic left heart syndrome).
Distribution of hemoglobin (Hb) threshold for hemodynamically stable patients (Part A in all scenarios). The mean Hb threshold below which respondents would prescribe packed red blood cells transfusion was statistically different between acyanotic scenarios and cyanotic scenarios (p < 0.0001). Diagonal lines 6 days of age, arterial switch. White bar 6 days, systemic-pulmonary shunt. Dots 5 months atrioventricular canal. Black bar 5 months Glenn for hypoplastic left heart syndrome
Mean transfusion threshold was higher in cyanotic than in acyanotic patients, by 2.2 g/dL (95 % confidence interval 2.0–2.4, p < 0.001) in stabilized patients and by 1.3 g/dL (95 % CI, 1.1–1.6, p < 0.001) in unstable patients (part B of the scenarios). Age was not a significant factor: The difference between mean transfusion threshold for neonates and infants was 0.3 g/dL (95 % CI −0.1 to 0.8, p = 0.17) in stabilized patients and 0.2 g/dL (95 % CI −0.1 to 0.6, p = 0.14) in unstable patients.
Physician and PICU characteristics did not significantly affect stated threshold Hb in all scenarios (Table 2). Transfusion threshold was lower in higher-volume centers (>200 cardiopulmonary bypass cases/year), but this was not statistically significant (p = 0.08).
Table 3 shows the average increase in Hb transfusion threshold for each possible clinical determinant within each scenario; all clinical determinants significantly increased transfusion threshold. Hemodynamic instability (part B vs. part A of the scenarios) was also associated with important increases in transfusion threshold over baseline for all scenarios. In acyanotic cases, the most important increase over baseline Hb transfusion threshold was observed with ECMO (+2.2 ± 1.4 g/dL), active bleeding (+2.0 ± 1.2 g/dL), and decreased SvO2 (+2.0 ± 1.3 g/dL). In cyanotic cases, decreased SvO2 (+1.2 ± 1.1 g/dL), oxygenation difficulties (+1.0 ± 1.0 g/dL), and active bleeding (+1.0 ± 1.0 g/dL) were also important clinical determinants. The increase in Hb transfusion threshold for acyanotic cases was significantly higher than in cyanotic cases for the actively bleeding child and for ECMO.
Discussion
This study describes the stated RBC transfusion practice pattern of physicians in the postoperative ICU care of pediatric cardiac surgery patients. We also characterized clinical, practitioner, and center-dependent determinants of RBC transfusion. Significant variability of Hb transfusion threshold was noted among physicians when presented four different clinical scenarios, ranging from <7.0 to 14.0 g/dL for cyanotic patients and<7.0 to 12.0 g/dL for acyanotic stabilized patients. This wide variation reflects the lack of consensus in the medical community regarding Hb transfusion threshold for pediatric postoperative cardiac surgery patients.
Few trials have attempted to define the ideal Hb transfusion threshold in pediatric cardiac surgery. They studied different transfusion thresholds, populations and outcomes, making comparisons difficult. In acyanotic patients, two randomized controlled trials sought to determine the lowest acceptable hematocrit level during CPB. The first study showed in 113 children younger than 9 months that hemodilution during CPB to hematocrit of 21.5 % (Hb ≈ 7.5 g/dL) compared to 27.8 % (Hb ≈ 9.3 g/dL) was associated with lower Bayley Psychomotor Development index at 1 year of age (81.9 ± 15.7 vs. 89.7 ± 14.7, p = 0.008) [20]. However, in a different study of 124 patients, the same psychomotor development index was similar at 1 year of age in subjects with hematocrits of 24.8 % (Hb ≈ 8.3 g/dL) and 32.6 % (Hb ≈ 10.9 g/dL) during CPB [21]. A subgroup analysis of 125 infants enrolled in the TRIPICU study after cardiac surgery [12] showed no significant difference in incidence of multiple organ dysfunction syndrome and death (12.7 vs. 6.3 %; p = 0.36) when comparing restrictive and liberal transfusion groups (Hb: 7.0 vs. 9.5 g/dL); however, neonates and patients with cyanotic heart disease were excluded from this trial [14]. Finally, a single-center randomized controlled trial in children with acyanotic congenital heart defects requiring elective cardiac surgery [22] demonstrated that a restrictive transfusion strategy (Hb < 8.0 g/dL) in the operating room and ICU, compared to a liberal one (Hb < 10.8 g/dL), was associated with shorter length of hospital stay. These studies suggest that Hb concentrations over 8.3 g/dL during CPB and over 7.0 g/dL in the PICU are likely safe in acyanotic pediatric cardiac surgery patients.
Less is known about the appropriate transfusion threshold for cyanotic postoperative patients. Physicians target higher Hb values for critically ill children with cyanotic heart disease [23]. A study of adults with cyanotic heart disease showed direct correlation between oxygen saturation and ideal Hb [24]. Yet, whether maintaining higher Hb levels in cyanotic postoperative cardiac surgery patients improves morbidity or mortality is unknown. To date, only one small randomized controlled trial addressed the question by allocating 60 children with cyanotic cardiac lesions to either a restrictive or liberal transfusion strategy (Hb < 9.0 vs. < 13.0 g/dL); no difference was observed in the postoperative blood lactate level [13]. Unfortunately, Beekman’s [25] statement in 1985 that “the optimal Hb concentration for children with cyanotic heart disease has yet to be determined” remains true three decades later.
Patient age did not significantly influence stated Hb transfusion threshold of respondents, with an increase of only 0.3 g/dL for neonates compared to infants. This differs from two previous surveys on stated transfusion practice in PICU patients, each including one cardiac scenario. In 2002, Laverdière et al. reported a mean increase of 0.9 g/dL Hb transfusion threshold for neonates compared to infants after correction of tetralogy of Fallot [15]. Twelve years later, Du Pont-Thibodeau et al. reported a smaller increase of 0.6 g/dL for the same scenario [17].
All nine determinants of hemodynamic instability increased Hb transfusion threshold in every scenario. Hb transfusion threshold for ECMO and for active bleeding was significantly higher for acyanotic cases compared to cyanotic cases. This may suggest a ceiling effect in transfusion thresholds, as cyanotic cases in our survey began with a higher baseline stated Hb transfusion threshold.
Whether there is a benefit to transfusing whole blood versus packed red cells or an optimal length of blood storage time remains a question of interest in this population. In this survey, 96 % of respondents state that they use packed red cells rather than whole blood. Twenty-two respondents (49 %) reported that there was a policy to use “fresh” RBC units transfused to their cardiac patients (Table 2), though 77 % stated that they did not know the average length of red cell storage prior to transfusion. Spinella [26] asked the same question to American blood bankers and pediatric intensivists: Most children’s hospitals (≥40 %) responded that they use RBC units stored less than 8 days in pediatric cardiac patients. It would be interesting to compare the outcomes of pediatric cardiac patients who received or did not receive RBC units stored less than a week.
One strength of this study is that we reached physicians across Canada involved in the postoperative care of pediatric cardiac surgery patients; our results represent national practice. The questionnaire’s scenarios were well validated and identified the most important determinants for practitioners. More importantly, this is the first survey of Hb transfusion threshold in pediatric cardiac surgery. There are, however, limitations to this study. Although considerable efforts were made to reach every physician providing postoperative cardiac PICU care in Canada, some may not have been reached. Survey response rate was 58 %. While it is possible that many of the non-respondents were not in fact direct participants in postoperative ICU patient care, we were not able to confirm this through this study. Systematic reviews of postal questionnaires reported a mean response rate of 54 % [27] to 61 % [28] for physicians. Our rate would be considered good, though not optimal, by experts in the field [29]. The results of this survey must be interpreted cautiously because its sample size is small. Furthermore, our results may not represent practice in other countries. Finally, generalizability of stated practice to actual practice is limited by desirability bias and the challenge to create scenarios that fully capture the complexity of real life cases.
In conclusion, there is a wide variation in reported RBC transfusion practice among Canadian physicians treating postoperative pediatric cardiac surgery patients in the ICU. Presence of cyanotic lesion and clinical determinants of instability, but not patient age, increased stated Hb transfusion threshold.
References
Keung CY, Smith KR, Savoia HF, Davidson AJ (2009) An audit of transfusion of red blood cell units in pediatric anesthesia. Pediatr Anesth 19:320–328. doi:10.1111/j.1460-9592.2009.02939.x
Hendrickson JE, Hillyer CD (2009) Noninfectious serious hazards of transfusion. Anesth Analg 108:759–769. doi:10.1213/ane.0b013e3181930a6e
Zubair AC (2009) Clinical impact of blood storage lesions. Am J Hematol 85:117–122. doi:10.1002/ajh.21599
Vamvakas EC, Blajchman MA (2007) Transfusion-related immunomodulation (TRIM): an update. Blood Rev 21:327–348. doi:10.1016/j.blre.2007.07.003
Kipps AK, Wypij D, Thiagarajan RR et al (2011) Blood transfusion is associated with prolonged duration of mechanical ventilation in infants undergoing reparative cardiac surgery. Pediatr Crit Care Med 12:52–56. doi:10.1097/PCC.0b013e3181e30d43
Salvin JW, Scheurer MA, Laussen PC et al (2011) Blood transfusion after pediatric cardiac surgery is associated with prolonged hospital stay. Ann Thorac Surg 91:204–210. doi:10.1016/j.athoracsur.2010.07.037
Székely A, Cserép Z, Sápi E et al (2009) Risks and predictors of blood transfusion in pediatric patients undergoing open heart operations. Ann Thorac Surg 87:187–197. doi:10.1016/j.athoracsur.2008.09.079
Shaw RE, Johnson CK, Ferrari G et al (2013) Blood transfusion in cardiac surgery does increase the risk of 5-year mortality: results from a contemporary series of 1714 propensity-matched patients: long-term outcome of blood transfusion. Transfus (Paris) 54:1106–1113. doi:10.1111/trf.12364
Murphy GJ, Reeves BC, Rogers CA et al (2007) Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circ 116:2544–2552. doi:10.1161/CIRCULATIONAHA.107.698977
Du Pont-Thibodeau G, Harrington K, Lacroix J (2014) Anemia and red blood cell transfusion in critically ill cardiac patients. Ann Intensive Care 4:16. doi:10.1186/2110-5820-4-16
Hébert PC, Wells G, Blajchman MA et al (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 340:409–417. doi:10.1056/NEJM199902113400601
Lacroix J, Hébert PC, Hutchison JS et al (2007) Transfusion strategies for patients in pediatric intensive care units. N Engl J Med 356:1609–1619. doi:10.1056/NEJMoa066240
Cholette JM, Rubenstein JS, Alfieris GM et al (2011) Children with single-ventricle physiology do not benefit from higher hemoglobin levels post cavopulmonary connection: results of a prospective, randomized, controlled trial of a restrictive versus liberal red-cell transfusion strategy*. Pediatr Crit Care Med 12:39–45. doi:10.1097/PCC.0b013e3181e329db
Willems A, Harrington K, Lacroix J et al (2010) Comparison of two red-cell transfusion strategies after pediatric cardiac surgery: a subgroup analysis. Crit Care Med 38:649–656. doi:10.1097/CCM.0b013e3181bc816c
Laverdière C, Gauvin F, Hébert PC et al (2002) Survey on transfusion practices of pediatric intensivists. Pediatr Crit Care Med 3:335–340. doi:10.1097/01.PCC.0000031371.88694.2B
Nahum E, Ben-Ari J, Schonfeld T (2004) Blood transfusion policy among european pediatric intensive care physicians. J Intensive Care Med 19:38–43. doi:10.1177/0885066603257966
Du Pont-Thibodeau G, Tucci M, Ducruet T, Lacroix J (2014) Survey on stated transfusion practices in PICUs*. Pediatr Crit Care Med 15:409–416. doi:10.1097/PCC.0000000000000121
Cook DJ, Guyatt GH, Jaeschke R et al (1995) Determinants in canadian health care workers of the decision to withdraw life support from the critically ill. Canadian critical care trials group. JAMA 273:703–708
Dillman DA (1978) Mail and telephone surveys: the total design method. John Wiley and Sons, New York
Jonas RA, Wypij D, Roth SJ et al (2003) The influence of hemodilution on outcome after hypothermic cardiopulmonary bypass: results of a randomized trial in infants. J Thorac Cardiovasc Surg 126:1765–1774. doi:10.1016/j.jtcvs.2003.04.003
Newburger JW, Jonas RA, Soul J et al (2008) Randomized trial of hematocrit 25 % versus 35 % during hypothermic cardiopulmonary bypass in infant heart surgery. J Thorac Cardiovasc Surg 135(347–354):e4. doi:10.1016/j.jtcvs.2007.01.051
Gast-Bakker DH, Wilde RBP, Hazekamp MG et al (2013) Safety and effects of two red blood cell transfusion strategies in pediatric cardiac surgery patients: a randomized controlled trial. Intensive Care Med 39:2011–2019. doi:10.1007/s00134-013-3085-7
Demaret P, Tucci M, Ducruet T et al (2014) Red blood cell transfusion in critically ill children (CME). Transfus (Paris) 54:365–375. doi:10.1111/trf.12261 (quiz 364)
Broberg CS, Jayaweera AR, Diller GP et al (2011) Seeking optimal relation between oxygen saturation and hemoglobin concentration in adults with cyanosis from congenital heart disease. Am J Cardiol 107:595–599. doi:10.1016/j.amjcard.2010.10.019
Beekman RH, Tuuri DT (1985) Acute hemodynamic effects of increasing hemoglobin concentration in children with a right to left ventricular shunt and relative anemia. J Am Coll Cardiol 5:357–362
Spinella PC, Dressler A, Tucci M et al (2010) Survey of transfusion policies at us and canadian children’s hospitals in 2008 and 2009: transfusion policy survey in children. Transfus (Paris) 50:2328–2335. doi:10.1111/j.1537-2995.2010.02708
Asch DA, Jedriewski MK, Christakis NA (1997) Response rates to mail surveys published in medical journals. J Clin Epidemiol 50:1129–1136
Cummings SM, Savitz LA, Konrad TR (2001) Reported response rates to mailed physician questionnaires. Health Serv Res 35:1347–1355
Burns KEA, Duffett M, Kho ME et al (2008) A guide for the design and conduct of self-administered surveys of clinicians. Can Med Assoc J 179:245–252. doi:10.1503/cmaj.080372
Acknowledgments
We thank the Fonds de la Recherche en Santé du Québec, Grant #24460 for the support of our study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
The return of a completed survey was considered to indicate consent to participate, as per institutional ethics committee guidance.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tremblay-Roy, JS., Poirier, N., Ducruet, T. et al. Red Blood Cell Transfusion in the Postoperative Care of Pediatric Cardiac Surgery: Survey on Stated Practice. Pediatr Cardiol 37, 1266–1273 (2016). https://doi.org/10.1007/s00246-016-1427-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1427-2