Abstract
Interstage mortality remains significant for patients undergoing staged palliation for hypoplastic left heart syndrome and other related single right ventricle malformations (HLV). The purpose of this study was to identify factors related to demographics, socioeconomic position, and perioperative course associated with post-Norwood hospital discharge, pre-stage 2, interstage mortality (ISM). Medical record review was conducted for patients with HLV, born from 1/2000 to 7/2009 and discharged alive following the Norwood procedure. Sociodemographic and perioperative factors were reviewed. Patients were determined to have ISM if they died between Norwood procedure hospital discharge and stage 2 palliation. Univariable and multivariable logistic regressions were performed to identify risk factors associated with ISM. A total of 273 patients were included in the analysis; ISM occurred in 32 patients (12 %). Multivariable analysis demonstrated that independent risk factors for interstage mortality included teen mothers [adjusted odds ratio (AOR) 6.6, 95 % confidence interval (CI) 1.9–22.5], single adult caregivers (AOR 4.1, 95 % CI 1.2–14.4), postoperative dysrhythmia (AOR 2.7, 95 % CI 1.1–6.4), and longer ICU stay (AOR 2.7, 95 % CI 1.2–6.1). Anatomic and surgical course variables were not associated with ISM in multivariable analysis. Patients with HLV are at increased risk of ISM if born to a teen mother, if they lived in a home with only one adult caregiver, suffered a postoperative dysrhythmia, or experienced a prolonged ICU stay. These risk factors are identifiable, and thus these infants may be targeted for interventions to reduce ISM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hypoplastic left heart syndrome and other related single right ventricle malformations (HLV) are among the most serious of congenital heart diseases, accounting for 25 % of cardiac mortality in the first week of life in the absence of surgical intervention [14]. Although operative care has brought about improvements in survival rates, mortality and morbidity remain significant. The highest risk period following hospital discharge is the first interstage period, the time between Norwood hospital discharge and second stage palliation, with mortality rates between 10 and 15 % [1, 12]. There are limited data regarding specific risk factors for interstage mortality (ISM), the time period between hospital discharge from the Norwood procedure and stage 2 palliation. Identification of risk factors for ISM may assist in the formation of target patient groups for increased education or monitoring during the interstage period.
The literature to date has primarily described the effects of anatomic and physiologic factors on the risk of ISM [5, 9, 13]. A recent Pediatric Heart Network study found that in addition to surgical and anatomic factors, socioeconomic status as measured by census block, patient ethnicity, and gestational age were associated with ISM [8]. The aim of this study was to assess the influence of factors related to social position on ISM. Defining the profile of those at risk of ISM is important to enhance resource investment and direction in interstage monitoring programs. Improved understanding of risk factors for ISM will be valuable to allow efficient direction of resources and interventions.
Methods
A medical record review was conducted for patients with HLV born between January 1, 2000, and June 30, 2009, who had undergone the Norwood procedure at the University of Michigan C. S. Mott Children’s Hospital. This study protocol was approved by the Institutional Review Board of the University of Michigan; written informed consent was not required. Patients were excluded if they died prior to hospital discharge from the Norwood procedure or remained in the hospital until stage 2 palliation. Patients were also excluded if they received cardiac transplantation rather than proceeding with staged palliation, or if deemed not a candidate for stage 2 palliation. Interstage mortality was defined as death after hospital discharge from the Norwood procedure and before admission for stage 2 palliation (Fig. 1). The time frame studied preceded development of the formal home monitoring program at our center.
Variables related to demographics and socioeconomic position (maternal age, family structure, insurance status, census block group variables, access to care variables, and race), underlying anatomy (anatomic subtype, the presence of obstructed pulmonary veins, ascending aortic diameter), surgical course [age at Norwood, shunt type, need for extracorporeal membrane oxygenation (ECMO), necrotizing enterocolitis (NEC), intensive care unit (ICU) length of stay (LOS)], and the postoperative period [tricuspid valve regurgitation, right ventricular systolic function, dysrhythmias, use of nasogastric (NG) tube at discharge] were reviewed. Insurance status was defined as having public or private insurance at the most recent hospital discharge.
Each patient was linked by current patient address, as recorded in the medical record, to his or her respective census block group from the 2000 U.S. census. Neighborhood Z-scores were calculated as a summary measure of overall neighborhood socioeconomic status, according to the methods of Diez-Roux et al. This metric comprises high school and college graduation percentages, median household income, median housing value, percent of households with interest/dividend/rent income, and percent of households with executive/manager/professional occupations [2]. In our study sample, a higher neighborhood Z-score reflects higher socioeconomic status for a given neighborhood. Additional census variables analyzed included percent unemployment, percent receiving public assistance, and percent with family income less than 200 % of the poverty level.
Patient access to care was also assessed using information obtained from the American Hospital Association database. Access to care was defined as distance from patient residence to the nearest hospital with a listed pediatric intensive care unit (PICU), calculated using Esri ArcMap v9.3 (Esri, Redlands, CA).
Demographic and clinical data were presented as frequency (%) for categorical variables and mean ± standard deviation (SD) or median [interquartile range (IQR)] for normally and non-normally distributed continuous variables, respectively. Associations with ISM were analyzed with Chi-square tests or Fisher’s exact tests, as appropriate, for categorical variables and t tests for normally distributed continuous variables.
Continuous variables that were not normally distributed were dichotomized either at the 75th percentile or at a clinically meaningful cutoff, including maternal age (teen mother was defined as ≤19 years of age vs >19 years) and number of home caregivers (single adult caregiver vs >1 adult caregiver). Univariable and multivariable logistic regressions based on the available data were used to calculate unadjusted and adjusted odds ratios (OR) and 95 % confidence intervals (CI) for factors associated with ISM. Variables with at least five events and P < 0.20 on univariable analysis were considered for multivariable regression. Given a correlation between race and single caregiver status, and the high number of missing values for race, race was not included as a candidate variable for the multivariable model. Similarly, hospital LOS was strongly correlated with ICU LOS; ICU LOS was included in the multivariable model rather than hospital LOS given the stronger association of ICU LOS with ISM on univariable analysis. Education and income variables were components of the overall neighborhood Z-score and thus would have created inherent redundancies in the model. Shunt type remained in the model given the finding from the Pediatric Heart Network’s Single Ventricle Reconstruction (SVR) Trial which demonstrated that an aorto-pulmonary artery shunt was associated with increased risk of ISM [11].
Model selection from multivariable logistic regressions was conducted using backward stepwise method with improvements in the model fit evaluated by the model Chi-square statistics. Multicollinearity for the variables included in the multivariable model was examined using variance inflation factor (VIF). If VIF for each variable in the model is less than 10, then it is acceptable to include all variables in the model, as VIF > 10 suggests multicollinearity. VIF for each variable in this model was <1.0. All analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC) with a significance set at P ≤ 0.05.
Results
Patient Characteristics
A total of 360 patients diagnosed with HLV who underwent the Norwood procedure were reviewed, and 273 patients (76 %) met inclusion criteria. Of the 273 patients included, 70 % were males, 78 % Caucasian, 8 % African-American, and 14 % other/unknown race (Table 1). There were 32 interstage deaths (12 %).
Univariable Analysis
Demographic Factors
On univariable analysis, African-American race (P = 0.0002), younger maternal age (≤19 years) (P = 0.004), and living with a single adult caregiver in the home (P = 0.02) were associated with increased risk of ISM (Table 1).
Census Block Group and Neighborhood Z-Score
Census block group and access to care analyses are summarized in Table 1. Census information was available for 258 subjects (95 %). Twelve of the unavailable subjects (4 %) listed addresses as post office box only, two addresses (<1 %) were not found in the geocoding software, and one patient lived in a census block group with only seven residents, and thus census block information was not available. Risk of ISM was elevated in census block groups with lower average percentage of high school graduates (P = 0.05), and lower average rent or dividend income (P = 0.05). There was a trend toward increased risk of ISM with lower mean combined neighborhood Z-score (P = 0.10), but this did not meet statistical significance. Rate of unemployment and need for public assistance showed no significant relationship with ISM.
Access to Care
Access to care variables were available for 259 subjects (94.9 %). Among these subjects, median distance to the nearest PICU was 21.7 miles (IQR 9.4–44.3 miles). There was no association between distance to nearest PICU and ISM (P = 0.83).
Surgical Factors
Risk of ISM was not associated with cardiac diagnosis or other anatomic variables. Four percent of patients with RVPA shunts and 13 % of patients with BT shunts experienced ISM, although this difference did not meet statistical significance (P = 0.09).
Perioperative Factors
Interstage mortality was increased for subjects with post-Norwood ICU LOS greater than or equal to 15 days (P = 0.009). Similarly, hospital LOS greater than or equal to 29 days demonstrated a trend toward increased risk of ISM, though this was not statistically significant (P = 0.10). Postoperative dysrhythmia was associated with increased risk of ISM (P = 0.03).
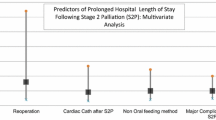
Multivariable Analysis
Candidate risk factors included in multivariable modeling are shown in Table 2. The final multivariable logistic regression demonstrated that independent risk factors for ISM included teen mothers (AOR 6.6, 95 % CI 1.9–22.5), single adult caregivers (AOR 4.1, 95 % CI 1.2–14.4), postoperative dysrhythmia (AOR 2.7, 95 % CI 1.1–6.4), and longer ICU LOS (AOR 2.7, 95 % CI 1.2–6.1) (Table 3).
Discussion
We found that ISM occurred in 12 % of subjects during the study period, which is consistent with the multicenter SVR trial results [8, 11]. The study period predates development of the formal home monitoring program at our center. We did find an association between sociodemographic factors and ISM; an increased risk of ISM was independently associated with a greater than 2-week stay in the ICU, having a teenage mother, and living in a home with only one adult caregiver as well as postoperative dysrhythmia.
In this study, we focused on addressing demographic factors and variables related to socioeconomic position in three ways: (1) analyzing census information, (2) assessing proximity to care, and (3) understanding social factors at the individual level.
Perhaps our most novel findings were that independent risk factors for ISM included children of teenage mothers and children with only one adult caregiver. These variables may relate to socioeconomic status, which is historically difficult to define and is especially difficult in this retrospective review. However, it is also possible that children of teenage mothers and those with only one adult caregiver may have an increased risk of ISM which is independent of socioeconomic status. Children with HLV have multiple medical needs after discharge from the Norwood procedure. In households with few (and young) caregivers, it may be an even greater challenge with more limited resources to manage medically complex children given limited time resources.
Mackie and colleagues found that low socioeconomic status, as defined by living in a low-income zip code (<$30,000 average household income per year), reduced the likelihood of readmission after congenital cardiac surgery, suggesting that reduced access to care may impact this population [10]. In addition, analysis of the Pediatric Heart Network’s SVR data demonstrated that children living in a census block at 5.4–13 % below the poverty line were at higher risk of ISM than those living in areas with fewer than 5.4 % below the poverty line, or greater than 13 % below the poverty line [8].
To examine the role of race specifically, Fixler et al. [3] demonstrated that in the first 5 years of life for infants with HLV, non-Hispanic blacks had an adjusted risk of death that was 41 % higher than that of non-Hispanic whites. The SVR study demonstrated that Hispanic ethnicity is an independent risk factor for ISM in multivariable analysis [8]. Further, in the American Association of Pediatrics review of health disparities over a 56-year period, it was found that children in all major US minority groups, including non-Hispanic blacks, had substantially greater risks of all-cause mortality after congenital heart surgery than whites [4]. Thus, in studies of patients with a variety of congenital heart diseases, including single ventricle lesions, racial minorities, and patients with families of low socioeconomic status were at a survival disadvantage, supporting the findings in our specific population.
Our finding that post-Norwood dysrhythmias were associated with increased risk of ISM is consistent with the findings from Simsic et al. [13], who found that arrhythmia in the postoperative period and decreased ventricular function at hospital discharge were independent risk factors for ISM in patients who have undergone the Norwood procedure. We also found that longer ICU stay was associated with an increased risk of ISM. Prolonged ICU LOS is likely a surrogate variable for the sickest patients. In fact, having a higher number of postoperative complications correlated with longer total LOS and was an independent risk factor for ISM in the SVR study [9].
Data from the SVR study demonstrated that ISM was higher among subjects with an aorto-pulmonary shunt compared to those who had been randomized to a right ventricle-to-pulmonary artery shunt. In our study, shunt type was not randomized, though some of our study’s subjects were from the era where patients were randomized in the SVR study. Interstage mortality for the group in our study with a Blalock–Taussig or central shunt at the Norwood procedure was 13 % compared to only 4 % of those with a right ventricle-to-pulmonary artery shunt. Thus, while not statistically significant, these point estimates are consistent with the findings from the SVR study.
There are several limitations to our study. First, this is a retrospective study and as such, there could be inherent biases secondary to our clinical practices. In addition, the American Hospital Association data were limited in completeness and based on institution self-report. Potentially, hospitals with reported pediatric care may have had very limited pediatric care, and others who could provide this care may not have thoroughly reported their work. We were unable to identify which pediatric intensive care units were part of a hospital that is designated as a tertiary care facility, nor were we able to discern which pediatric intensive care units had a strong pediatric cardiology presence. Thus, there are limitations to the access to care analyses. Finally, this study’s event size is small (32 interstage deaths), and we have tested multiple variables for their relationship to ISM, which may raise the possibility of false associations.
Despite these limitations, the finding that some subjects may be identifiable as having increased risk of ISM prior to hospital discharge is valuable, in order to effectively focus efforts to improve interstage survival. There has been interest in providing home monitoring to all infants during the interstage period; some reports on home monitoring have shown no interstage deaths in those patients who were monitored [6, 7]. Although the results are encouraging, resource-intensive home monitoring programs may not be possible for all infants who have undergone the Norwood procedure. Our findings provide a potential target population for home monitoring, increased home nursing visits, or more educational initiatives for parents prior to hospital discharge.
References
Azakie T, Merklinger SL, McCrindle BW, Van Arsdell GS, Lee KJ, Benson LN et al (2001) Evolving strategies and improving outcomes of the modified Norwood procedure: a 10-year single institution experience. Ann Thorac Surg 72:1349–1353
Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ et al (2001) Neighborhood of residence and incidence of coronary heart disease. N Engl J Med 345:99–106
Fixler DE, Nembhard WN, Salemi JL, Ethen MK, Canfield MA (2010) Mortality in first 5 years in infants with functional single ventricle born in Texas, 1996 to 2003. Circulation 121:644–650
Flores G, Committee on Pediatric Research (2010) Technical report—racial and ethnic disparities in the health and health care of children. Pediatrics 125(4):979–1020
Furck AK, Uebing A, Hansen JH, Scheewe J, Jung O, Fischer G et al (2010) Outcome of the Norwood operation in patients with hypoplastic left heart syndrome: a 12-year single-center survey. J Thorac Cardiovasc Surg 139:359–365
Ghanayem NS, Hoffman GM, Mussatto KA, Cava JR, Frommelt PC, Rudd NA et al (2003) Home surveillance program prevents interstage mortality after the Norwood procedure. J Thorac Cardiovasc Surg 126(5):1367–1377
Ghanayem NS, Cava JR, Jaquiss RDB, Tweddell JS (2004) Home monitoring of infants after stage one palliation for hypoplastic left heart syndrome. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 7:32–38
Ghanayem NS, Allen KR, Tabbutt S, Atz AM, Clabby ML, Cooper DS et al (2012) Interstage mortality after the Norwood procedure: results of the multicenter Single Ventricle Reconstruction trial. J Thorac Cardiovasc Surg 144(4):896–906
Hehir DA, Dominguez TE, Ballweg JA, Ravishankar C, Marino BS, Bird GL et al (2008) Risk factors for interstage death after stage 1 reconstruction of hypoplastic left heart syndrome and variants. J Thorac Cardiovasc Surg 136:94–99
Mackie AS, Gauvreau K, Newburger JW, Mayer JE, Erickson LC (2004) Risk factors for readmission after neonatal cardiac surgery. Ann Thorac Surg 78:1972–1978
Ohye RG, Sleeper LA, Mahony L, Newburger JW, Pearson GD, Lu M, Pediatric Heart Network Investigators et al (2010) Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med 362(21):1980–1992
Pearl JM, Nelson DP, Schwartz SM, Manning PB (2002) First stage palliation for hypoplastic left heart syndrome in the twenty-first century. Ann Thorac Surg 73:331–340
Simsic JM, Bradley SM, Stroud MR, Atz AM (2005) Risk Factors for interstage death after the Norwood procedure. Pediatr Cardiol 26:400–403
Watson DG, Rowe RD (1962) Aortic-valve atresia. Report of 43 cases. JAMA 179(1):14–18
Acknowledgments
We acknowledge the University of Michigan SBRP (Student Biomedical Research Program) and the University of Michigan MCRiT (Multidisciplinary Clinical Researchers in Training) Program for their financial support for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report.
Rights and permissions
About this article
Cite this article
Taylor, L.C., Burke, B., Donohue, J.E. et al. Risk Factors for Interstage Mortality Following the Norwood Procedure: Impact of Sociodemographic Factors. Pediatr Cardiol 37, 68–75 (2016). https://doi.org/10.1007/s00246-015-1241-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1241-2