Abstract
Atrioventricular valve regurgitation (AVVR) influences morbidity and mortality in the atrioventricular canal defect (AVC). Fetal cardiac structures are subject to hemodynamic changes, as well as growth and maturation during gestation, which may alter the degree of AVVR and affect prognosis. We sought to investigate the frequency of change in degree of AVVR documented by fetal echocardiography (echo) between different periods of gestational age. Subjects with AVC seen in the Fetal Heart Program between January 2008 and September 2010 were identified. Degree of AVVR was assessed by color Doppler imaging and categorized as Grade 0 (no AVVR), Grade 1 (hemodynamically insignificant AVVR = trivial or mild), and Grade 2 (hemodynamically important AVVR = ≥moderate). Levels of AVVR between periods were compared. Forty-three fetuses were analyzed. Overall, 60 % had no change, 14 % had a decrease, and 26 % had an increase in AVVR grade. Two fetuses progressed from Grade 0 or 1 to Grade 2, while one fetus decreased from Grade 2 to Grade 0. Trisomy 21 and heterotaxy syndrome were not risk factors for AVVR progression. Transitional and incomplete canal defects may be more susceptible to AVVR progression. Sixty percent of fetuses with AVC will not exhibit progression of AVVR between the second and third trimesters of gestation. In those who exhibit change, it is most often within a hemodynamically insignificant range between none and mild regurgitation (Grades 0 and 1). These findings have implications for the counseling, follow-up, and delivery plans of the fetus with AVC defect.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fetal cardiac structures and cardiovascular hemodynamics are subject to changes in utero following organogenesis, as well as growth and maturation. As gestation progresses, there is an increase in preload as overall blood volume increases, as well as a decrease in placental impedance, causing a decrease in afterload [9, 11, 14]. In addition, the heart grows with the fetus and the atrioventricular (AV) valve apparatus matures as gestational age (GA) progresses.
In patients with atrioventricular canal defects, the structure of the AV valve can result in variable amounts of AV valve regurgitation, which can affect the hemodynamics of the fetal circulation [3, 15]. Patient morbidity and mortality are significantly influenced by the degree of AV valve regurgitation [1, 5, 12]. Some data suggest that the amount of regurgitation present in fetal life is typically similar to that in postnatal life [3, 6, 10, 13, 18]. In addition, the degree of regurgitation prior to surgical intervention in more than half of patients does not improve postoperatively [9, 11, 14, 16]. Due to the significant impact of AV valve regurgitation on clinical outcomes, the degree of regurgitation assessed in utero impacts the manner of counseling, frequency of patient follow-up, delivery plan, and overall prognostic assessment [3, 4, 7, 15]. However, the natural history of AV valve regurgitation throughout gestation has not yet been studied in a serial, longitudinal manner in the fetus with AV canal defect.
Methods
This is a retrospective, descriptive study investigating the natural history and frequency of change in the degree of AV valve regurgitation of fetuses with AV canal defects diagnosed by echocardiography at different periods of gestation. A secondary aim of the study is to assess whether trisomy 21 or heterotaxy syndrome represent risk factors for progression of AV valve regurgitation between mid- and late gestation. Fetuses with incomplete (no ventricular septal defect), transitional (restrictive ventricular septal defect), and complete (large ventricular septal defect) common AV canal anomalies who underwent fetal echocardiography within the Fetal Heart Program at the Children’s Hospital of Philadelphia (CHOP) between January 01, 2008, and September 30, 2010, were identified. Patients were included for analysis if they underwent a fetal echocardiogram at both ≤28-weeks gestation and ≥32-weeks gestation. If more than two fetal echocardiograms were performed, we recorded information from the first and last fetal studies to create the largest window of time of gestational maturation between analyses.
Fetal echocardiograms were performed on Siemens Acuson Sequoia Ultrasound Machines (Mountain View, CA) with a 6C2 curvilinear probe with a default setting for color scale set between 60 and 80 cm/s. Degree of atrioventricular valve regurgitation (AVVR) can be graded in multiple ways by echocardiography. In addition to qualitative assessment, our imaging laboratory guidelines for assessment of AVVR use the general principles of semiquantitative assessment of AVVR by Doppler color flow using the ratio of the regurgitant jet area to the atrial area. The percentage of regurgitant color jet area in comparison with the atrial area <30 % is mild, 30–50 % moderate, and >50 % severe AVVR [1, 5, 12, 17].
This study was designed to identify major changes in AVVR that could significantly affect clinical outcome. As a result, report descriptions of AVVR were divided into three broad classifications: Grade 0 represents no AV valve regurgitation; Grade 1 represents hemodynamically insignificant AV valve regurgitation, while Grade 2 represents hemodynamically significant AV valve regurgitation. The designation of hemodynamic significance applies to the range of regurgitation equal to or greater than moderate regurgitation. These are degrees of insufficiency that could potentially place a fetus at risk of heart failure with possible hydrops and/or impairment of growth and development, or would engender a consideration for possible need for surgical attention at the time of operative repair. If right and/or left AV regurgitation was described, the highest degree of regurgitation was used for analysis. Data were compiled and described in categorical form. Chi-squared and Fisher’s exact tests were used to perform statistical analysis with significance set at p < 0.05.
Results
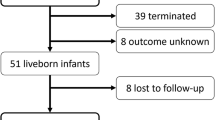
During the study period, 100 patients with AV canal defects were evaluated in the Fetal Heart Program at The Children’s Hospital of Philadelphia. Of this group, 43 patients qualified for inclusion in this study with serial fetal echocardiograms performed at both ≤28-weeks gestation and ≥32-weeks gestation to allow for comparison. Patients excluded from the analysis had a similar distribution of the type of AV canal defect and the presence of heterotaxy syndrome and Down syndrome. Eighty-eight percent of the cases were complete AV canal defects, while 12 % were transitional or incomplete AV canal defects. Within the group of complete AV canal patients, 58 % (22/38) had relatively well-balanced ventricles, while 42 % (16/38) had unbalanced ventricular arrangement, resulting in hypoplasia of one of the ventricular chambers. Within the group of 43 subjects, five had pulmonary atresia, five had significant right ventricular outflow tract obstruction or valvar pulmonary stenosis, while three had aortic arch hypoplasia requiring arch augmentation or reconstruction at postnatal surgery.
The average GA at the first study evaluated was 22.7 ± 3.0 weeks for patients included in the analysis. The average GA at the final study evaluated was 35.3 ± 1.4 weeks. In fetuses with a GA of ≤28-weeks, 13/43 (30 %) had Grade 0 AVVR, 23/43 (53 %) had Grade 1 AVVR, and 7/43 (16 %) had Grade 2 AVVR. In the follow-up study at a GA of ≥32-weeks, 10/43 (23 %) had Grade 0 AVVR, 25/43 (58 %) had Grade 1, and 8/43 (19 %) had Grade 2 AVVR (Table 1).
Change in AVVR grade was then analyzed and demonstrated that 26 of 43 patients (60 %) evaluated had no change in AVVR. Six of 43 patients (14 %) had a decrease in AVVR. Eleven of 48 patients (26 %) had an increase in AVVR (Fig. 1). Four of five (80 %) subjects with a transitional or incomplete AV canal defect had an increase in AVVR. Despite the high rate of increased regurgitation within this subgroup, the change in AVVR was hemodynamically insignificant, increasing from Grade 0 to Grade 1. Only two patients (2/43, 5 %) demonstrated an increase in AVVR with progression from a score of 0 or 1 to a score of 2, representing a hemodynamically significant change in regurgitation. Both of these patients had complete AV canal defects. The first patient had trisomy 21 with balanced ventricles that were normal in size, as well as mild aortic valve and transverse arch hypoplasia. The other subject had heterotaxy syndrome with segments {S,L,D}, a common atrium, unbalanced atrioventricular canal favoring the right ventricle, and double outlet right ventricle with transverse arch hypoplasia and coarctation of the aorta.
Distribution of comparison of AVVR recorded in mid-gestation and late gestation within the study group. X-axis represents the number of patients with a specific grade of regurgitation at ≤28-weeks gestation, while the Y-axis represents the specific grade of regurgitation at ≥32-weeks gestation (graphics by Microsoft Word)
Analysis of the genetic and syndromic status of the fetuses in the study group demonstrates that 21 subjects had trisomy 21, 14 were diagnosed with heterotaxy syndrome based on anatomical features, one had chromosome 8p deletion, five had no known abnormalities, and two had an unknown genetic/syndromic status. There was no statistically significant association between trisomy 21 and heterotaxy syndrome and progression of AVVR; however, the number of subjects with AVVR progression and the overall number of subjects without these syndromes were low (Fig. 2).
Discussion
Fetal echocardiography not only evaluates the anatomy of a structural heart defect, but also provides information on the function and pathophysiology of the cardiovascular system of the fetus [3, 6–8, 10, 13, 18]. Serial prenatal cardiovascular imaging is now regularly performed on patients diagnosed with congenital heart disease in utero. As a result, we are now able to observe the natural history of physiological changes that occur during gestation after the heart has formed and continues to mature. AV canal defects represent a type of congenital heart disease that can be appreciated in the four-chamber view in screening obstetric ultrasounds [2]. As a result, the diagnosis of an AV canal defect is commonly made with fetal imaging [2, 9, 11, 14, 16].
In this study, we focused our observations on the degree of AV valve regurgitation in patients with AV canal defects at ≤28-weeks gestation and at ≥32-weeks gestation. There was an increase in AVVR in 26 %, most notably seen in patients with transitional or incomplete canal defects. This suggests that incomplete or transitional canal defects may be susceptible to AVVR progression in utero to a greater degree than those with complete AV canal defect; however, the number of subjects with this diagnosis was small. Patients with incomplete or transitional AV canal defects may have differences in valve and subvalvar architectural structure when compared to complete AV canal defects. Dense chordal attachments to the septum in those without a large ventricular septal defect may place such patients at risk of progression of regurgitation. Nevertheless, the majority of patients with worsening AVVR, including all the patients with incomplete or transitional AV canal defects, did not demonstrate a major change in AVVR that resulted in hemodynamic compromise.
Despite physiological changes during gestation, as well as growth and maturation of the fetal heart, 95 % of patients with AV canal defects demonstrated no hemodynamically significant change in AV valve regurgitation from mid-gestation to late gestation (grade remained 0 or 1). There were two patients within the cohort that demonstrated a hemodynamically significant change in AVVR during gestation. One subject had Down syndrome and a balanced Rastelli type C complete AV canal. The other patient had heterotaxy syndrome with an unbalanced AV canal and double outlet right ventricle. A unifying feature of the cardiac disease of both patients was transverse arch hypoplasia. A potential mechanistic explanation for the progression of AV valve regurgitation in these patients could be that evolution of arch obstruction over the course of gestation contributes to an increase in afterload for the ventricle over time, resulting in worsening AV valve regurgitation. Obstruction to outflow could represent a risk factor for the development of worsening AVVR during gestation; however, the small numbers in this study limit the generalizability of these data.
In a previous analysis, we retrospectively evaluated the same group of patients with diagnosis of AV canal defect by fetal echocardiography and investigated the likelihood of progression of AV valve regurgitation from fetal life to the first month of postnatal life [3, 4, 7, 15]. Our analysis demonstrated that 90 % of patients diagnosed with AV canal defects display no hemodynamically significant change in AV valve regurgitation from fetal to postnatal life despite the significant hemodynamic changes associated with the transition from fetus to neonate at birth. Furthermore, we also analyzed postnatal echocardiograms performed at ≥1 month of age in unrepaired patients, none of whom were receiving prostaglandin E1 therapy. Of these patients, 18/22 (82 %) exhibited no hemodynamically significant AVVR progression from fetal life to ≥1 month of life. Other studies have demonstrated that AV valve regurgitation seen postnatally prior to operative repair is a risk factor for AV valve incompetence requiring reoperation after complete repair [1, 5, 12, 17].
There are several limitations to this study. This was a retrospective analysis subject to referral bias of patients with complex congenital heart disease presenting to our tertiary care center. Patients with complex findings were more likely to require close surveillance with frequent studies and were therefore more likely to meet the inclusion criteria for the study. However, the high rate of trisomy 21 and heterotaxy syndrome, as well as additional cardiac abnormalities, is consistent with other studies in the literature [3, 6–8, 10, 13, 18]. One hundred patients were diagnosed with AV canal defect in fetal life during the study period, and 43 had two studies for analysis. The excluded patients had similar characteristics to those included in the study.
The findings of this analysis indicate that the AV valve regurgitation in patients with AV canal defects evaluated by fetal echocardiography performed at mid-gestation is predictive of that seen in the final fetal echocardiogram in the late third trimester, closer to delivery. Our data suggest that fetuses with AV canal defects with hemodynamically insignificant AV valve regurgitation and no obstruction to outflow at mid-gestation may not require frequent follow-up imaging for the sole purpose of the evaluation of AV valve regurgitation prior to the final fetal echocardiogram before birth. AV valve regurgitation affects overall prognosis, and as a result, prediction of the degree and fluctuation of AV valve regurgitation as the child grows is important for assessment of outcomes. Our study suggests that the fetal assessment of AV valve regurgitation at mid-gestation is good predictor of long-term AV valve regurgitation, and therefore provides a good foundation for accurate individualized counseling and estimation of prognosis for families of these children when the diagnosis is made in fetal life.
References
Boening A, Scheewe J, Heine K et al (2002) Long-term results after surgical correction of atrioventricular septal defects. Eur J Cardiothorac Surg 22:167–173
Craig B (2006) Atrioventricular septal defect: from fetus to adult. Heart 92:1879–1885. doi:10.1136/hrt.2006.093344
Davey B, Thacker D, Rychik J (2013) Atrioventricular valve regurgitation in the fetus with atrioventricular canal defect: transition from prenatal to postnatal life. Pediatr Cardiol. doi:10.1007/s00246-013-0711-7
Gembruch U, Knöpfle G, Chatterjee M et al (1991) Prenatal diagnosis of atrioventricular canal malformations with up-to-date echocardiographic technology: report of 14 cases. Am Heart J 121:1489–1497
Harmandar B, Aydemir NA, Karaci AR et al (2012) Results for surgical correction of complete atrioventricular septal defect: associations with age, surgical era, and technique. J Card Surg 27:745–753. doi:10.1111/jocs.12016
Huggon IC, Cook AC, Smeeton NC et al (2000) Atrioventricular septal defects diagnosed in fetal life: associated cardiac and extra-cardiac abnormalities and outcome. J Am Coll Cardiol 36:593–601
Jone P-N, Schowengerdt KO (2009) Prenatal diagnosis of congenital heart disease. Pediatr Clin North Am 56:709–715. doi:10.1016/j.pcl.2009.04.002
Khoo NS, Van Essen P, Richardson M, Robertson T (2008) Effectiveness of prenatal diagnosis of congenital heart defects in South Australia: a population analysis 1999–2003. Aust N Z J Obstet Gynaecol 48:559–563. doi:10.1111/j.1479-828X.2008.00915.x
Kiserud T (2005) Physiology of the fetal circulation. Semin Fetal Neonatal Med 10:493–503. doi:10.1016/j.siny.2005.08.007
Langford K, Sharland G, Simpson J (2005) Relative risk of abnormal karyotype in fetuses found to have an atrioventricular septal defect (AVSD) on fetal echocardiography. Prenat Diagn 25:137–139. doi:10.1002/pd.1037
Marek J, Tomek V, Skovránek J et al (2011) Prenatal ultrasound screening of congenital heart disease in an unselected national population: a 21-year experience. Heart 97:124–130. doi:10.1136/hrt.2010.206623
Michielon G, Stellin G, Rizzoli G et al (1995) Left atrioventricular valve incompetence after repair of common atrioventricular canal defects. ATS 60:S604–S609
Rasiah SV, Ewer AK, Miller P et al (2008) Outcome following prenatal diagnosis of complete atrioventricular septal defect. Prenat Diagn 28:95–101. doi:10.1002/pd.1922
Rychik J (2004) Fetal cardiovascular physiology. Pediatr Cardiol 25:201–209. doi:10.1007/s00246-003-0586-0
Silverman NH, Kleinman CS, Rudolph AM et al (1985) Fetal atrioventricular valve insufficiency associated with nonimmune hydrops: a two-dimensional echocardiographic and pulsed Doppler ultrasound study. Circulation 72:825–832
Suzuki K, Tatsuno K, Kikuchi T, Mimori S (1998) Predisposing factors of valve regurgitation in complete atrioventricular septal defect. J Am Coll Cardiol 32:1449–1453
Wu YT, Chang AC, Chin AJ (1993) Semiquantitative assessment of mitral regurgitation by Doppler color flow imaging in patients aged <20 years. Am J Cardiol 71:727–732
Yıldırım G, Gungorduk K, Yazıcıoğlu F et al (2009) Prenatal diagnosis of complete atrioventricular septal defect: perinatal and neonatal outcomes. Obstet Gynecol Int 2009:958496. doi:10.1155/2009/958496
Acknowledgments
We wish to acknowledge the efforts of the cardiovascular imaging specialists at The Fetal Heart Program at The Children’s Hospital of Philadelphia, Zhiyun Tian, MD, Peggy McCann, RCDS, and Debra Soffer, RCDS, for their contributions to image acquisition. Dr. Rychik is supported in part by the Robert and Dolores Harrington Endowed Chair in pediatric cardiology at The Children’s Hospital of Philadelphia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Davey, B.T., Rychik, J. The Natural History of Atrioventricular Valve Regurgitation Throughout Fetal Life in Patients with Atrioventricular Canal Defects. Pediatr Cardiol 37, 50–54 (2016). https://doi.org/10.1007/s00246-015-1237-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1237-y