Abstract
Few previous studies have addressed exercise capacity in patients with corrected congenital heart disease (CHD) and significant anatomical residua. The aim of this study was to determine the aerobic fitness and peak cardiac function of patients with corrected CHD with complete or incomplete repairs, as determined by resting echocardiography. Children, adolescents and young adults (<40 years) with CHD from both sexes, who had previously undergone biventricular corrective therapeutic interventions (n = 73), and non-CHD control participants (n = 76) underwent cardiopulmonary exercise testing. The CHD group was further divided according to the absence/presence of significant anatomical residua on a resting echocardiogram (“complete”/“incomplete” repair groups). Aerobic fitness and cardiac function were compared between groups using linear regression and analysis of covariance. Peak oxygen consumption, O2 pulse and ventilatory threshold were significantly lower in CHD patients compared with controls (all p < 0.01). Compared with the complete repair group, the incomplete repair group had a significantly lower mean peak work rate, age-adjusted O2 pulse (expressed as % predicted) and a higher VE/VCO2 ratio (all p ≤ 0.05). Peak oxygen consumption was comparable between the subgroups. Patients after corrected CHD have lower peak and submaximal exercise parameters. Patients with incomplete repair of their heart defect had decreased aerobic fitness, with evidence of impaired peak cardiac function and lower pulmonary perfusion. Patients that had undergone a complete repair had decreased aerobic fitness attributed only to deconditioning. These newly identified differences explain why in previous studies, the lowest fitness was seen in patients with the most hemodynamically significant heart malformations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The survival of children with congenital heart disease (CHD) has improved dramatically over the last two decades, and most young patients will now reach adulthood [12]. However, besides the issue of an ever-aging population group, adults with CHD have an increased risk of morbidity and mortality compared to the general healthy population—mostly from cardiovascular disease [32, 45]. Results have shown that during aging, exercise capacity and cardiac function of adults with CHD decline [24], probably due to a combination of both intrinsic factors and physical inactivity. Children with CHD also have a higher prevalence of obesity and physical inactivity compared to healthy children [30, 34], conditions which likely lay the foundations for the increased morbidity and mortality observed later in adulthood. For example in one study, exercise intolerance and activity restrictions were significantly and positively associated with increased body mass index (BMI) and BMI percentiles in children with CHD; furthermore, activity restriction was found to be the strongest predictor of risk of becoming overweight and obese [38].
Exercise training programs for children with CHD may help them in maintaining a healthy lifestyle, while decreasing the risks of adulthood morbidity. A recent systematic review of such programs in children and young adults with CHD concluded that most studies did show a positive effect of exercise training [15]. It was also concluded that exercise training was safe in this population. Nevertheless, when prescribing exercise to a CHD patient, several factors should be taken into account, e.g., the type of exercise to be performed, the intensity and duration; the type of heart malformation and the corrective procedures performed; the presence or lack of anatomical residua; ventricular function; pulmonary arterial pressure; the initial fitness level; and the presence or lack of exercise-induced rhythm abnormalities [7, 20, 39].
Patients with CHD are usually followed up using resting echocardiography and cardiac magnetic resonance imaging [2, 35, 44]. These modalities assess cardiac morphology and function at rest, which do not necessarily reflect maximal and dynamic cardiac capacity, as observed during exercise [1, 36]. By using resting measures alone, the cardiologist or exercise specialist are limited in making an accurate assessment of the patient’s exercise capacity, and in providing personalized exercise recommendations and prescription.
Cardiopulmonary exercise testing (CPET) can evaluate maximal aerobic performance and cardiac function and can provide important information on functional outcomes and the safety of exercise [36, 41]. Furthermore, CPET results can be used to predict survival in adults with CHD [13, 14, 22], making CPET also an important prognostic tool. For these reasons, clinical guidelines support the routine use of CPET in the periodic evaluation of children and adults with CHD [7, 39].
Few previous studies have addressed the issue of exercise capacity in CHD patients with significant anatomical residua. It was found that hemodynamically significant lesions such as pulmonary stenosis or pulmonary insufficiency can result in reduced exercise capacity [29, 37]. Patients after tetralogy of Fallot (TOF) repair with significant residual pulmonary stenosis had lower maximal oxygen consumption than patients with lesser residual gradients [26]. In addition, it had been shown that cardiorespiratory fitness normalized after pulmonary valve replacement in children and adolescents with repaired TOF with pulmonary regurgitation [16]. However, data on the relationships between the level of CHD corrections, mainly regarding the presence of anatomical residua, and functional parameters obtained from CPET are scarce and had not been reported to date for other cardiac lesions.
The aim of this study was to determine the aerobic fitness and peak cardiac function of patients with corrected CHD with complete or incomplete repairs, as determined by resting echocardiography, compared with a non-CHD comparison group. We hypothesized that patients that had undergone a complete correction of their heart defect would demonstrate normal peak cardiac function in maximal exercise, while those that still have a hemodynamically significant lesion would have a decreased cardiac function.
Methods
Participants
The study population included 73 CHD patients (53 males, 20 females) younger than 40 years of age who had previously undergone biventricular corrective therapeutic interventions (catheterization/surgery), had no other significant comorbidities and who were referred to our exercise laboratory for CPET as part of their regular cardiology follow-up.
The CHD patient group was further divided into two subgroups, according to the absence/presence of significant anatomical residua on a resting 2-dimensional echocardiogram. The first group included 49 CHD patients that underwent repair and had no significant anatomical residua (“complete repair”). This group included patients after correction of TOF (n = 13), transposition of the great arteries (n = 11, all after an arterial switch operation), ventricular septal defect (VSD, n = 9), coarctation of the aorta (n = 6), Ross procedure (n = 3), pulmonary valvuloplasty (n = 1), pulmonary valvuloplasty and VSD repair (n = 1), atrioventricular canal repair (n = 1), mitral valvuloplasty (n = 1), closure of a patent ductus arteriosus (n = 1), partial anomalous pulmonary venous return repair (n = 1) and bypass of a left main coronary due to atresia (n = 1). The second group included 24 CHD patients that underwent repair of their congenital heart defect, yet had significant anatomical residua (“incomplete repair”).
Patients in the incomplete repair group all had a hemodynamically significant anatomical residue on resting echocardiogram, as determined by an experienced pediatric cardiologist (author Uriel Katz). Valvular lesions were considered hemodynamically significant if graded as moderate or severe according to the 2014 AHA/ACC guideline for the management of patients with valvular heart disease [33]. Ventricular dysfunction was considered significant if graded as moderate or severe according to the ASE/EAE recommendations for chamber quantification [27]. The heart defects and procedures in this group were TOF repair with residual pulmonic insufficiency (n = 8), pulmonary stenosis after a Rastelli procedure (n = 5), transposition of the great arteries after a Mustard procedure (n = 3), left ventricular dysfunction after transposition of the great arteries or TOF repair (n = 4), pulmonary stenosis after a Ross procedure (n = 2), aortic stenosis (n = 1) and aortic insufficiency (n = 1).
The non-CHD comparison group included 76 healthy children and young adults (<40 years), who were referred for exercise testing due to clinical complaints (e.g., chest pain, dyspnea, palpitations). All had a normal cardiac echocardiogram, were evaluated by a pediatric cardiologist and a sports medicine specialist and concluded as having no evidence of cardiac, ventilatory or circulatory abnormality.
Participants were not included in the study if they were receiving any medication that had potential cardiovascular effects (e.g., diuretics, beta-blockers, digoxin, angiotensin-converting enzyme inhibitors, methylphenidate) or had any other chronic medical condition other than their known heart disease (in the CHD group) or overweight/obesity. In addition, CHD patients that had undergone a single ventricle repair were not included, nor were participants whose exercise tests were stopped before reaching maximal ability due to an overt lack of cooperation.
The study was ethically approved by the Institutional Review Board of Sheba Medical Center, Tel Hashomer, Israel, and conducted according to the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Data Collection
Demographic and clinical information on medical history and current medication use were collected from the participants’ hospital records and CPET reports. Prior to the exercise test, a frontal interview with the patient/guardian was performed by a physician (authors Gal Dubnov-Raz or Uriel Katz), who inquired about past and current medical history and treatment, and reviewed the participant’s medical record. If more than one cardiac lesion was present, the lesion considered as the most significant hemodynamically was recorded as the main diagnosis.
Anthropometry Measures
Stature was measured using a wall-mounted stadiometer (Seca 206, Seca gmbh, Hamburg, Germany), to the nearest 0.1 cm. Body mass was measured using an electronic scale (Tanita BC418-MA, Tokyo, Japan) to the nearest 0.1 kg. BMI was calculated as mass in kg divided by the square of stature in meters.
Cardiopulmonary Exercise Testing
Resting Pulmonary Measurements
All participants underwent inspiratory and expiratory spirometry prior to exercise testing. The spirometry maneuver was explained and demonstrated prior to the test. Maximal voluntary ventilation (MVV) was estimated by multiplying the forced expiratory volume in the first second (FEV1) by 40 [46] and used to calculate the breathing reserve after exercise termination.
Exercise Protocol
The CPET protocol used included an incremental progressive exercise test on an electronically braked cycle ergometer (Ergoselect 100, Ergoline GmbH, Bitz, Germany). After unloaded pedaling for 3 min, the work rate was increased gradually by 5, 10, 15 or 20 W min−1, according to the predetermined estimation of the individual’s predicted peak work rate [19] for children, and according to individual predicted peak oxygen uptake for adults [21]. The increase in work rate was calculated so that exercise duration would last between 8 and 12 min. Participants were instructed to maintain a pedaling rate (cadence) of 60–65 rpm. The exercise test was symptom-limited and terminated when the participant asked to stop, while reporting maximal ability and showing clinical signs of intense effort (e.g., very heavy breathing, facial flushing), or when the required cadence could not be maintained for 5 s or more. Intense verbal encouragement was provided by the staff throughout the test.
Electrocardiographic Measurements
A standard 12-lead electrocardiogram was used to analyze cardiac rhythm at rest and throughout the exercise test. Because peak heart rate during bicycle exercise is usually 5–10 % lower than treadmill exercise, the predicted maximal heart rate for each individual was calculated as 208 − 0.7*age [40] multiplied by a factor of 0.925 [6, 36].
Gas Exchange Measurements and Definitions
Oxygen uptake (VO2), carbon dioxide production (VCO2) and minute ventilation (VE) were measured by a computerized breath-by-breath analyzer (ZAN ErgoSpiro 680, nSpire Health, Inc. Longmont, CO, USA). The predicted peak VO2 was calculated using regression equations published for adults (>18 years) [21] and for children and adolescents [9]. Low aerobic fitness was defined as a peak VO2 < 85 % of predicted. Respiratory exchange ratio (RER), the ratio between VCO2 and VO2, was measured continuously, and the value at peak exercise was used. The ventilatory threshold (VAT) was identified by an experienced exercise physiologist using the V-slope method [5] and expressed both as relative values (mL O2 kg−1 min−1) and as a percentage of the predicted peak VO2. The O2 pulse, analogous to stroke volume [36, 46], was calculated as VO2/heart rate at peak exercise. The predicted maximal O2 pulse was obtained from published sources for adults [46] and for children [10]. The O2 pulse data were expressed both as absolute values (in mL O2 beat−1) and as a percentage of the predicted age- and sex-specific value. Low O2 pulse was defined as <85 % of predicted.
The VE/VCO2 ratio, a marker of ventilatory efficiency and cardiac function [11], was measured at the VAT. A value below 30 was considered normal [3]. Breathing reserve was calculated as MVV minus peak VE and expressed in liters.
Statistical Analysis
Descriptive mean and SD values were calculated for all variables. Proportions were compared by the Chi-square test. Measures of cardiac function were compared between CHD and comparison groups using multiple linear regression techniques and analysis of covariance. Adjustment for age was made by analysis of covariance where appropriate. Age and sex were also controlled for by the use of ‘percentage of the predicted values’ in those variables which have age-dependent norms, i.e., peak VO2 and peak O2 pulse. Similar comparisons were made between the two CHD subgroups. IBM SPSS Statistics software version 21 was used for statistical analyses. Two-tailed p values of ≤0.05 were considered as statistical significance.
Results
Demographic and anthropometric characteristics of all participants are presented in Table 1. Participants in the CHD group were older on average and had a higher mean stature, body mass and BMI than the non-CHD comparison group. There was no significant difference in the male/female ratio.
Exercise Performance in CHD Versus Non-CHD Comparison Groups
Table 2 presents the physiological parameters obtained at peak exercise. Peak exercise performance, expressed as either peak oxygen consumption or as age-adjusted peak load obtained, was significantly decreased in CHD patients compared with the comparison group (p < 0.001). Age-adjusted O2 pulse was also significantly lower in the CHD group (p = 0.012). A greater proportion of participants from the CHD group had a significantly decreased fitness and decreased O2 pulse, compared with controls (p < 0.001 and p = 0.009, respectively).
Table 3 presents submaximal exercise parameters in CHD patients and the non-CHD comparison group. The ventilatory threshold was significantly lower in the CHD group (p < 0.001). The VE/VCO2 ratio was increased in the CHD group compared with the non-CHD comparison group, and the proportion of participants with an abnormal VE/VCO2 ratio was significantly higher in the CHD group (p = 0.001 and p = 0.021, respectively).
Exercise Parameters in Participants With Complete Versus Incomplete CHD Repair
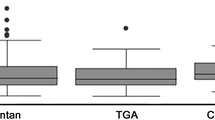
Tables 2 and 3 also present exercise parameters in the two CHD subgroups compared with the non-CHD group. Figure 1 displays the relative difference in several parameters between the two CHD subgroups and the non-CHD comparison group. Participants from both subgroups had a significantly decreased aerobic function as compared with controls, with no significant between-group difference (p > 0.05). The proportion of participants with low fitness also did not differ significantly between the two CHD subgroups (p > 0.05). The incomplete repair group had a significantly lower peak work rate expressed either as absolute or age adjusted compared with the complete repair group. Age-adjusted O2 pulse was also lower in both subgroups compared with controls, with a lower value found in the incomplete repair group compared with the complete repair group, which approached statistical significance (p = 0.06). However, when expressed as a percentage of age- and sex-specific predicted values, the lower O2 pulse value was statistically significant (p = 0.047). The proportion of participants with a decreased O2 pulse did not differ significantly between the CHD subgroups (p > 0.05). After adjustment for age, maximal ventilation (VE) was lower in the incomplete repair group only, compared with the non-CHD comparison group (p = 0.05).
Relative reduction in several exercise parameters in the two CHD subgroups as compared to controls. MHR—maximal heart rate, as percent of predicted values; peak VO2—as percent of predicted values; VAT—ventilatory threshold, as percent of predicted peak VO2; peak WR—peak work rate, age adjusted; O2 pulse—as percent of predicted values; VE—maximal ventilation, age adjusted; VE/VCO2 ratio—expressed as 1 minus the difference from the maximal normal value of 30, in order to graphically display higher VE/VCO2 values as a functional decrease. * Statistically significant difference (p < 0.05) compared to controls. † Statistically significant difference (p < 0.05) compared to other CHD subgroup
The mean VE/VCO2 ratio was slightly higher in the incomplete repair group compared with the complete repair group (p = 0.05). The proportion of participants with an elevated VE/VCO2 ratio did not differ significantly between the CHD subgroups. A lower end-tidal CO2 pressure was found in the incomplete repair group compared with the complete repair group and controls (p = 0.038 and p = 0.050, respectively).
Discussion
The aims of this study were to determine the aerobic fitness and cardiac function of patients with corrected CHD and to compare measures of cardiac and ventilatory functions between CHD patients with complete or incomplete repair. Both peak and submaximal exercise parameters were significantly decreased in CHD patients compared with controls. However, we have shown for the first time that participants with an incomplete repair of their heart defect had a significantly lower peak work rate, age-adjusted O2 pulse, age-adjusted maximal ventilation (VE) and a higher mean VE/VCO2 ratio compared to CHD patients that had undergone a complete repair (Fig. 1). These findings reflect an impaired cardiac function and lower pulmonary perfusion that can be brought about by several possible mechanisms depending on the specific residual abnormalities: decreased right ventricular function, left ventricular diastolic dysfunction or significant valvular regurgitation.
Our findings should alert clinicians to the possibility that a CHD patient with a hemodynamically significant anatomical residue on resting echocardiogram possesses lower aerobic fitness and maximal cardiac function. As aerobic fitness is a major determinant of health and longevity [4], this possibility should be taken into consideration when prescribing exercise to these individuals. As the medical care of CHD patients continuously improves, survivorship is set to increase. Yet, the natural history of young adults with CHD is a progressive decline in exercise performance [18, 25, 31]. Continuous administration of exercise prescription and healthy lifestyle recommendations can be expected to improve their overall health, increase prognosis and decrease the medical and financial burden.
Very few previous studies focused on exercise testing in CHD patients with significant residual lesions. Studies mainly dealt with pulmonary regurgitation or stenosis, and usually in the context of TOF repair [8, 16, 23, 29, 37]. Collectively, these studies described lower exercise times, lower peak heart rates and reduced work capacity. For example, Roos-Hesselink et al. [37] studied 38 adult patients, 22–23 years after surgery for pulmonary stenosis repair, and found reduced maximal work capacity—which was even lower in those with severe pulmonary regurgitation and right ventricular dilatation. In all of these former studies, CHD patients who underwent corrective procedures, yet remained with significant anatomical residua, had a reduced exercise capacity demonstrated by a variety of methods. However, no clear association was found between the severity of the residual findings and the degree of exercise intolerance; patients with milder residual findings were not significantly different than the more severe ones. This finding, described as “striking” by Luijnenburg et al. [29], was attributed to possible diastolic dysfunction, sinus node dysfunction and other causes effecting cardiac function. Our findings suggest to the contrary; the lower aerobic capacity observed in CHD patients with mild residual findings is likely the result of deconditioning, with no significant impairment of cardiac function.
The lower exercise capacity found in our study participants is in agreement with previous studies in children [28, 43] and adults [17, 29, 37, 42] with CHD. The largest series had been published by Kempny et al. [24], who evaluated the results of over 4400 CPET examinations in adults with various types of CHD. Most patients had a reduced exercise capacity compared to normal values, with decreasing fitness levels seen with increasing severity of the heart defect. Our study extends these findings, as Kempny et al. [24] did not specifically differentiate between the levels of corrections that the patients underwent and only focused on adults. Our findings, of a decreased cardiac function in the incomplete repair group, may partially explain why the lowest peak VO2 values seen in the former studies were in adult CHD patients that still had an abnormal anatomy and/or function, e.g., Eisenmenger’s syndrome, complex CHD, Fontan circulations and Ebstein’s anomaly [24].
By analyzing a wide range of exercise parameters, we demonstrated that, as we hypothesized, the limitation to exercise following complete repair of CHD is not caused by reduced cardiac function; it is more likely the result of deconditioning. Exercise training is therefore expected to improve fitness in this population, as had been previously described [15]. The expansion of the multi-disciplinary team that treats CHD patients to include exercise trainers, clinical physiologists or sports medicine personnel, which will utilize available published resources regarding exercise in CHD [e.g., 7, 20, 39], would be advantageous for the care of this population. Such a dedicated person would be able to administer a safe, efficient and personally tailored exercise prescription to each patient, in order to improve her/his health and well-being.
As with all studies, several limitations should be acknowledged. Our sample size was limited due to strict inclusion and exclusion criteria. This may be one explanation why the lower mean peak VO2 found in the incomplete repair group was not statistically significant, while other measures of peak exercise performance were decreased, compared with the complete repair group. Another potential limitation of our study is that the data are derived from a single center. Different cardiac surgeons and interventional cardiologists may have slightly different practices, which in turn may result in slight hemodynamic differences between patients that are not necessarily identified by the echocardiogram. Different physicians may also differ in their approaches to physical activity and exercise in patients following CHD repair. Finally, there was a significant difference in mean age between CHD patients and controls. We addressed this difference by adjusting for age in our analyses and by presenting data that are highly age dependent, such as peak VO2 and peak O2 pulse, as percent of age- and sex-predicted reference values.
The strengths of our study are the large variety of heart malformations included, both in the complete and in the incomplete groups, while only patients with pulmonary regurgitation/insufficiency were used for studies on exercise capacity in the presence of anatomical residua. We performed symptom-limited CPETs to exertion, while several previous studies used submaximal tests. Finally, our analyses included a large number of maximal and submaximal cardiac and ventilatory parameters obtained from the exercise test.
In summary, this study found that peak and submaximal exercise parameters were significantly decreased in CHD patients compared with controls. The major new finding was that CHD patients with incomplete repair of their heart defect had evidence of impaired maximal cardiac function and lower pulmonary perfusion, while participants that underwent complete repair had no evidence of a cardiac or a ventilatory limitation to exercise, signifying proper maximal function of these systems. Clinicians should be aware that CHD patients with significant anatomical residua could have decreased exercise performance and heart function and therefore could provide appropriate, individually tailored exercise prescription to enhance aerobic fitness.
References
Albouaini K, Egred M, Alahmar A, Wright DJ (2007) Cardiopulmonary exercise testing and its application. Heart 93:1285–1292
Bailliard F, Hughes ML, Taylor AM (2008) Introduction to cardiac imaging in infants and children: techniques, potential, and role in the imaging work-up of various cardiac malformations and other pediatric heart conditions. Eur J Radiol 68:191–198
Balady GJ, American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Peripheral Vascular Disease; Interdisciplinary Council on Quality of Care and Outcomes Research et al (2010) Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American heart association. Circulation 122:191–225
Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, Blair SN (2014) Fitness vs. fatness on all-cause mortality: a meta-analysis. Prog Cardiovasc Dis 56:382–390
Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60:2020–2027
Braden DS, Carroll JF (1999) Normative cardiovascular responses to exercise in children. Pediatr Cardiol 20:4–10
Budts W, Börjesson M, Chessa M, van Buuren F, Trigo Trindade P, Corrado D, Heidbuchel H, Webb G, Holm J, Papadakis M (2013) Physical activity in adolescents and adults with congenital heart defects: individualized exercise prescription. Eur Heart J 34:3669–3674
Carvalho JS, Shinebourne EA, Busst C, Rigby ML, Redington AN (1992) Exercise capacity after complete repair of tetralogy of Fallot: deleterious effects of residual pulmonary regurgitation. Br Heart J 67:470–473
Cooper DM, Weiler-Ravell D, Whipp BJ, Wasserman K (1984) Aerobic parameters of exercise as a function of body size during growth in children. J Appl Physiol Respir Environ Exerc Physiol 56:628–634
Cooper DM, Weiler-Ravell D, Whipp BJ, Wasserman K (1984) Growth-related changes in oxygen uptake and heart rate during progressive exercise in children. Pediatr Res 18:845–851
Cooper DM, Kaplan MR, Baumgarten L, Weiler-Ravell D, Whipp BJ, Wasserman K (1987) Coupling of ventilation and CO2 production during exercise in children. Pediatr Res 21:568–572
Deanfield J, Thaulow E, Warnes C, Task Force on the Management of Grown Up Congenital Heart Disease, European Society of Cardiology; ESC Committee for Practice Guidelines et al (2003) Management of grown up congenital heart disease. Eur Heart J 24:1035–1084
Diller GP, Dimopoulos K, Okonko D, Li W, Babu-Narayan SV, Broberg CS, Johansson B, Bouzas B, Mullen MJ, Poole-Wilson PA, Francis DP, Gatzoulis MA (2005) Exercise intolerance in adult congenital heart disease: comparative severity, correlates, and prognostic implication. Circulation 112:828–835
Dimopoulos K, Okonko DO, Diller GP, Broberg CS, Salukhe TV, Babu-Narayan SV, Li W, Uebing A, Bayne S, Wensel R, Piepoli MF, Poole-Wilson PA, Francis DP, Gatzoulis MA (2006) Abnormal ventilatory response to exercise in adults with congenital heart disease relates to cyanosis and predicts survival. Circulation 113:2796–2802
Duppen N, Takken T, Hopman MT, ten Harkel AD, Dulfer K, Utens EM, Helbing WA (2013) Systematic review of the effects of physical exercise training programmes in children and young adults with congenital heart disease. Int J Cardiol 168:1779–1787
Eyskens B, Reybrouck T, Bogaert J, Dymarkowsky S, Daenen W, Dumoulin M, Gewillig M (2000) Homograft insertion for pulmonary regurgitation after repair of tetralogy of Fallot improves cardiorespiratory exercise performance. Am J Cardiol 85:221–225
Fredriksen PM, Chen A, Veldtman G, Hechter S, Therrien J, Webb G (2001) Exercise capacity in adult patients with congenitally corrected transposition of the great arteries. Heart 85:191–195
Giardini A, Hager A, Pace Napoleone C, Picchio FM (2008) Natural history of exercise capacity after the Fontan operation: a longitudinal study. Ann Thorac Surg 85:818–821
Godfrey S (1974) The response of normal children to exercise. In: Godfrey S (ed) Exercise testing in children. W.B. Saunders C, London, p 68
Graham TP Jr, Driscoll DJ, Gersony WM, Newburger JW, Rocchini A, Towbin JA (2005) Task force 2: congenital heart disease. J Am Coll Cardiol 45:1326–1333
Hansen JE, Sue DY, Wasserman K (1984) Predicted values for clinical exercise testing. Am Rev Respir Dis 129(2 Pt 2):S49–S55
Inuzuka R, Diller GP, Borgia F, Benson L, Tay EL, Alonso-Gonzalez R, Silva M, Charalambides M, Swan L, Dimopoulos K, Gatzoulis MA (2012) Comprehensive use of cardiopulmonary exercise testing identifies adults with congenital heart disease at increased mortality risk in the medium term. Circulation 125:250–259
Jonsson H, Ivert T, Jonasson R, Holmgren A, Björk VO (1995) Work capacity and central hemodynamics thirteen to twenty-six years after repair of tetralogy of Fallot. J Thorac Cardiovasc Surg 110:416–426
Kempny A, Dimopoulos K, Uebing A, Moceri P, Swan L, Gatzoulis MA, Diller GP (2012) Reference values for exercise limitations among adults with congenital heart disease. Relation to activities of daily life—single centre experience and review of published data. Eur Heart J 33:1386–1396
Kipps AK, Graham DA, Harrild DM, Lewis E, Powell AJ, Rhodes J (2011) Longitudinal exercise capacity of patients with repaired tetralogy of Fallot. Am J Cardiol 108:99–105
Lambert J, Ferguson RJ, Gervais A, Gilbert G (1980) Exercise capacity, residual abnormalities and activity habits following total correction for tetralogy of Fallot. Cardiology 66:120–131
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Longmuir PE, Tremblay MS, Goode RC (1990) Postoperative exercise training develops normal levels of physical activity in a group of children following cardiac surgery. Pediatr Cardiol 11:126–130
Luijnenburg SE, de Konig WB, Romeih S, van den Berg J, Vligen HW, Mulder BJM, Helbing WA (2012) Exercise capacity and ventricular function in patients treated for isolated pulmonary valve stenosis or tetralogy of Fallot. Int J Cardiol 158:359–363
McCrindle BW, Williams RV, Mital S, Clark BJ, Russell JL, Klein G, Eisenmann JC (2007) Physical activity levels in children and adolescents are reduced after the Fontan procedure, independent of exercise capacity, and are associated with lower perceived general health. Arch Dis Child 92:509–514
Müller J, Ewert P, Hager A (2015) Only slow decline in exercise capacity in the natural history of patients with congenital heart disease: a longitudinal study in 522 patients. Eur J Prev Cardiol 22:113–118
Nieminen HP, Jokinen EV, Sairanen HI (2007) Causes of late deaths after pediatric cardiac surgery: a population-based study. J Am Coll Cardiol 50:1263–1271
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O’Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD, American College of Cardiology, American Heart Association Task Force on Practice Guidelines (2014) 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63:e57–e185
Pinto NM, Marino BS, Wernovsky G, de Ferranti SD, Walsh AZ, Laronde M, Hyland K, Dunn SO Jr, Cohen MS (2007) Obesity is a common comorbidity in children with congenital and acquired heart disease. Pediatrics 120:e1157–e1164
Puranik R, Muthurangu V, Celermajer DS, Taylor AM (2010) Congenital heart disease and multi-modality imaging. Heart Lung Circ 19:133–144
Rhodes J, Ubeda Tikkanen A, Jenkins KJ (2010) Exercise testing and training in children with congenital heart disease. Circulation 122:1957–1967
Roos-Hesselink JW, Meijboom FJ, Spitaels SE, vanDomburg RT, vanRijen EH, Utens EM, Bogers AJ, Simoons ML (2006) Long-term outcome after surgery for pulmonary stenosis (a longitudinal study of 22–33 years). Eur Heart J 27:482–488
Stefan MA, Hopman WM, Smythe JF (2005) Effect of activity restriction owing to heart disease on obesity. Arch Pediatr Adolesc Med 159:477–481
Takken T, Giardini A, Reybrouck T, Gewillig M, Hövels-Gürich HH, Longmuir PE, McCrindle BW, Paridon SM, Hager A (2012) Recommendations for physical activity, recreation sport, and exercise training in paediatric patients with congenital heart disease: a report from the Exercise, Basic & Translational Research Section of the European Association of Cardiovascular Prevention and Rehabilitation, the European Congenital Heart and Lung Exercise Group, and the Association for European Paediatric Cardiology. Eur J Prev Cardiol 19:1034–1065
Tanaka H, Monahan KD, Seals DR (2001) Age-predicted maximal heart rate revisited. J Am Coll Cardiol 37:153–156
Ten Harkel AD, Takken T (2010) Exercise testing and prescription in patients with congenital heart disease. Int J Pediatr. doi:10.1155/2010/791980
Therrien J, Fredriksen P, Walker M, Granton J, Reid GJ, Webb G (2003) A pilot study of exercise training in adult patients with repaired tetralogy of Fallot. Can J Cardiol 19:685–689
Tomassoni TL (1996) Role of exercise in the management of cardiovascular disease in children and youth. Med Sci Sports Exerc 28:406–413
Valente AM, Cook S, Festa P, Ko HH, Krishnamurthy R, Taylor AM, WarnesCA Kreutzer J, Geva T (2014) Multimodality imaging guidelines for patients with repaired tetralogy of Fallot: a report from the American Society of Echocardiography: developed in collaboration with the Society for Cardiovascular Magnetic Resonance and the Society for Pediatric Radiology. J Am Soc Echocardiogr 27:111–141
Verheugt CL, Uiterwaal CS, van der Velde ET, Meijboom FJ, Pieper PG, van Dijk AP, Vliegen HW, Grobbee DE, Mulder BJ (2010) Mortality in adult congenital heart disease. Eur Heart J 31:1220–1229
Wasserman K, Hansen JE, Sue DY, Stringer WW, Sietsema KE, Sun XG, Whipp BJ (eds) (2010) Clinical exercise testing. In: Principles of exercise testing and interpretation, 5th edn. Lippincott, Philadelphia
Acknowledgments
This study was performed in partial fulfillment of the requirements for an MD degree by Dr. Omer Rosenblum at the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Omer Rosenblum and Uriel Katz have contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Rosenblum, O., Katz, U., Reuveny, R. et al. Exercise Performance in Children and Young Adults After Complete and Incomplete Repair of Congenital Heart Disease. Pediatr Cardiol 36, 1573–1581 (2015). https://doi.org/10.1007/s00246-015-1198-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1198-1