Abstract
Retrograde Intra-Renal Surgery (RIRS) plays a primary role in renal stone treatment context. Energy, frequency and width of laser impulse can be modulated by surgeons to achieve better outcomes. In our study, patients with single renal stone sized 10–20 mm were retrospectively divided into two groups. Patients of Group 1 underwent RIRS with Low-Energy (LE) High-Frequency (HF) settings using Lumenis® 120-W high-power Ho:YAG laser. Patients of Group 2 (control) underwent RIRS using “standard” settings by means of Sphinx® Jr 30 W Ho:YAG system. Follow-up was conducted with a CT scan at 3 months after RIRS in both groups. Procedure success was defined as stone-free or presence of ≤ 4 mm fragments (Clinical Insignificant Residual Fragments—CIRF). A total number of 199 patients were included: 86 LE/HF RIRS (Group 1) vs 113 “conventional” RIRS (Group 2). Mean operative time was 56.6 (± 19.4) min in Group 1 vs 65.2 (± 25.2) min in Group 2 (p = 0.01). Mean hospitalization time was 2.5 ± 1.7 days for Group 1 vs 2.9 ± 3.2 days for Group 2 (p = 0.2). Peri-operative complications were counted: eight in Group 1 and 11 in Group 2 (p > 0.05). At 3-month control, stone-free rate was 69% (59/86 patients) in Group 1 vs 65% (73/113 patients) in Group 2 (p = 0.6). Success rate was 93% (80/86) in Group 1 in comparison to 82% (93/113) in Group 2 (p = 0.03). In conclusion, LE/HF RIRS seems to be a feasible and effective technique with a reduction of operative time and optimal results in terms of “stone-free” and “success” rates. Further studies are needed to ensure the validity of our results and to give evidence-based statements.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retrograde IntraRenal Surgery (RIRS) is one of the first line treatments for < 20 mm renal stones [1, 2] and can be applied also for bilateral renal stones [3].
Holmium:Yttrium aluminum garnet (Ho:YAG) laser lithotripsy can be considered the gold standard tool for stone vaporization during upper urinary tract endoscopy [4, 5].
Nowadays, the advent of more powerful and pliable laser systems is changing the features of this intervention. 100–120 W Holmium lasers make available an almost limitless number of Energy/Frequency combinations. Defining general rules for the different settings and methods of laser application could be the key to “jump to the next level” in terms of RIRS procedure evolution.
In this specific issue, the classical dichotomy consists of these two different approaches: fragmentation vs dusting.
“Fragmentation” means utilization of high energy pulses to shatter the stone into fragments for subsequent removal, which is completed usually by stone retrieval baskets. The advantages of fragmentation consist of minor lithotripsy time and reduced dispersion of fragments in the kidney calyces, along with a prolonged time for fragment extraction. Another advantage can be represented by the possibility of stone analysis after procedure, for diagnosis, and post-operative medical therapy of urolithiasis.
On the other hand, “dusting” means reducing to very small fragments (≤ 250 μm as recently defined by Keller, Traxer et al. [6]) the stone burden using low/medium levels of energy and Long Pulse Width settings. After a “pure” dusting RIRS, the fragments would be passively “washed” out or dissolved by urine flow. The advantages could consist of a decreased operative time and minor risk of urinary tract injury by repeated passage of ureteroscope or repositioning of ureteral access sheaths. Nevertheless, there are also disadvantages: dust precipitation in the calyces can lead to stone reformation. Furthermore, the lack of a complete stone analysis may be considered a disadvantage too.
These two “pure” approaches can be combined during the same RIRS, adapting the modality of the intervention to patient and stone’s features.
The aim of this study is to evaluate the outcomes of Low Energy (LE)/High Frequency (HF) RIRS using a 120-W Holmium laser in comparison to lithotripsy performed using “standard” settings (utilizing a 30-W Holmium laser) for the treatment of single renal stones sized between 10 and 20 mm.
Materials and methods
Patients and outcomes
Patients who underwent Retrograde IntraRenal Surgery (RIRS) at S. Croce & Carle Hospital (Cuneo, Italy) from January 2016 were included in our database.
The use of high-power or “standard” lasers for each case was decided at the moment of the intervention on the basis of two criteria: the availability of the laser at the moment of the surgery and the choice of the surgeon.
All patients aged more than 18 years old with single renal (calyces or pelvis) stones sized from 10 to 20 mm were eligible for the study.
Exclusion criteria were applied: presence of ureteral stones; multiple renal stones; preoperative urinary tract infections (UTIs), except for asymptomatic positive urine culture (managed with preoperative antibiotic drugs in accordance to antibiogram).
Patients included in this series signed a specific informed consent. All cases were managed according to the principles of the Declaration of Helsinki.
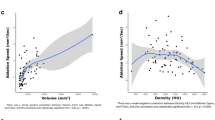
We ensured to collect preoperative data: age, gender, side of kidney affection, mean stone size and density (using Hounsfield classification), stone position, mean pre-intervention values of Creatinine and eGFR, previous placement JJ ureteral stent before RIRS, etc.
Data were retrospectively analysed and patients were divided into two groups according to the laser and the settings used.
Group 1—Case—Technique
All procedures were performed in supine lithotomy position [7].
Initially, the surgeon proceeded to place a 0.035-inch polytetrafluoroethylene-coated guidewire up to the kidney excretory system by cystoscopy. If a JJ stent was previously inserted, it was removed at this time. Then, a semirigid ureteroscopy was performed up to the ureteropelvic junction (UPJ) to explore the ureter in search of stone fragments or ureteral kinking/stenoses. After these propaedeutic steps, in every case a ureteral access sheath (UAS) was positioned (9.5, 10/12 or 12/14 Ch, depending on the ureteral diameter and compliance—35 cm for women, 45 cm for men).
Finally, the surgeon inserted the flexible ureteroscope (Flex X2, Sheath size 7.5 Ch, working channel inner diameter 3.6 Ch, Karl Storz®) exploring all renal calyces and pelvis.
Lithotripsy was performed with a 120-W high-power Ho:YAG laser system (Lumenis® Ltd., Yokneam Industrial Park Hakidma 6, Yokneam 2069204 Israel) and a 200 micron laser fiber.
The technique consists of three phases (Table 1):
-
1.
First phase: Contact Laser Lithotripsy (Low Energy and High Frequency—LE-HF)
A stone dusting technique was applied using a precise setting of Ho-YAG laser, as reported in Table 1: 0.2 J–70 Hz for low and average density stones; 0.5 J–50 Hz for “hard” stones (LE-HF). During this phase, a Long Pulse Width laser setting (LPW—1000 μs) was used and the surgeon ensured to put the laser fiber in direct contact with the stone, to obtain small fragments and dust. Dusting was continued until the size of the residual fragments was liable to extraction.
-
2.
Extraction of main fragments
The major fragments were extracted using a zero tip 1.9 Ch nitinol basket. All fragments were sent to laboratory for stone analysis.
-
3.
Second stage non-contact Laser lithotripsy (LE-HF Pop-dusting)
All small residual fragments were reduced to dust by means of a 0.5 J–80 Hz Short Pulse Width (300 μs) laser setting (LE-HF-SPW pop-dusting). During this phase, the surgeon maintained the laser fiber in the center of the involved calyx, with a distance of 1–2 mm from the stone fragments (Pop-corning phase). When the calyx was too dilated or difficult to reach, the fragments were displaced to a more easily approachable position.
Group 2—Control—Technique
Patients of Group 2 underwent RIRS with the same steps and phases described for Group 1, except for laser system and settings (Table 2).
We used a Sphinx® Jr 30 W Ho:YAG laser system (LISA laser, 3123 Independence Drive, Livermore CA 94551 USA). During the first phase, a setting 0.5 J/20 Hz LPW (650 μs) was used for dusting, then extraction of main fragments was completed as in Group 1. Finally, for the second stage lithotripsy, a 1 J/15 Hz SPW (300 μs) laser setting was applied for POP-corning, without contact between laser fiber and stones.
Postoperative care
At the end of every intervention, both in Group 1 and in Group 2, a JJ ureteral stent was inserted and a vesical catheter was left until the day after procedure.
In post-operative day 1, all patients were screened for renal function and inflammatory markers: Serum Creatinine, eGFR, complete blood count and C-reactive protein assessment. Blood pressure and oxygenation, temperature and heart rate were monitored twice a day until dismission.
Follow-up
Follow-up was conducted in both Groups with a CT scan performed at 3 months after endoscopy, plus a complete urological examination. Procedure success was defined as stone-free or presence of ≤ 4 mm fragments (Clinical Insignificant Residual Fragments—CIRF).
Complications were registered and classified using Clavien-Dindo Grading Classification (C-D) [8].
Statistical analysis
Qualitative variables were reported as numbers and percentages. Quantitative discrete variables were described as median [interquartile range − IQR] value and quantitative continuous variables as mean [standard deviation − DS] values. Independent Samples T-Student Test was used to compare means, while Chi-Square test was used to compare percentages between the groups.
All tests were conducted using Microsoft Excel 16.22 version for Macintosh; p values < 0.05 were considered as significant.
Results
Patients
From January 2016 to September 2019, a total number of 199 eligible patients with single renal stone sized 10–20 mm underwent RIRS at S. Croce & Carle Hospital (Cuneo, CN, Italy).
86 patients underwent LE/HF RIRS (Group 1), while 113 patients underwent “standard” ureteroscopy (Group 2).
Demographics and baseline characteristics were comparable between the groups (Table 3) except for preoperative eGFR, which was 88 (± 21) ml/min/1.73 m2 in Group 1 vs 80 (± 23) ml/min/1.73 m2 in Group 2 (p = 0.02).
Peri-operative data and outcomes
Mean operative time was 56.6 (± 19.4) min in Group 1 and 65.2 (± 25.2) min in Group 2 (p value 0.01).
In Group 1, 47 (55%) patients underwent RIRS under spinal anesthesia, while in Group 2 spinal puncture was executed successfully in 53 (47%) patients (p > 0.05) [9, 10]. The indication to spinal or general anesthesia depended on anesthetist’s decision and/or surgeon’s preference.
Intraoperative complications were registered: 0 complications in Group 1 and 2 complications in Group 2 (intraoperative bleeding from urinary tract) which have made it necessary to stop the intervention precociously in both cases.
Mean hospitalization time was comparable between the groups (2.5 ± 1.7 days in Group 1 and 2.9 ± 3.2 days in Group 2, p = 0.2). Serum creatinine after intervention was higher in Group 2 (0.9 ± 0.2 in Group 1 vs 1 ± 0.3 in Group 2, p = 0.03), with no statistical difference in terms of eGFR (Group 1 89% ± 21% ml/min/1.73 m2 vs 85% ± 24% ml/min/1.73 m2 in Group 2, p = 0.2).
The median period between intervention and JJ stent removal was 7 days (5–28) in Group 1 vs 7 days (2–23) in Group 2 (p = 0.4).
Post-operative complications have been reported: eight complications in Group 1 (two cases of C-D Grade I, three complications C-D Grade II, 2 C-D Grade III and 1 C-D Grade IV) and nine complications in Group 2 (2 C-D Grade I, 4 C-D Grade II, 2 C-D Grade III and 1 C-D Grade IV) (p > 0.05) (Table 4) [11].
At 3-month CT scan, stone-free rate was 69% (59/86 patients) in Group 1 vs 65% (73/113 patients) in Group 2 (p = 0.6). Success rate was 93% (80/86) in Group 1 in comparison to 82% (93/113) in Group 2 (p = 0.03).
Four patients of Group 1 and six patients in Group 2 needed re-intervention because of significant residual fragments (p > 0.05). All these patients underwent second-look RIRS, applying the same technique of the first procedure (the four patients of Group 1 underwent LE/HF second-look RIRS, while the six patients of Group 2 underwent the “control” flexible ureteroscopy). None patient needed a third-look RIRS in both groups.
The results of post-operative physicochemical analysis of the stones are reported in Table 5: no statistically significant difference emerged between the groups in terms of lithiasis composition rates.
Discussion
Nowadays, the presence of innovative medical devices and new technologies on the market has made it necessary to give evidence-based indications to their use. Latest generation high-power Ho-YAG lasers make available a wide range of possibilities of modulation for laser parameters: energy, frequency, potency (as product of the two afore-mentioned physical quantities) and pulse duration. These features can be applied to a stone or an organ with various effects depending on their combination. For example, we can execute the lithotripsy of two renal stones using in both cases a potency of 40 W, obtaining two completely different results: the settings 2 J × 20 Hz SPW and 0.5 J × 80 Hz LPW have the same potency, but not the same effect.
As a consequence, a critical investigation about laser settings and their use seems to be crucial in contemporary endourology.
Aldoukhi et al. [12] already tried to explore the argument. The Authors focused on the effects of different high-power Ho-YAG laser settings and technologies (as “Moses” Technology—Lumenis®) on stone lithotripsy, focusing on clinical and surgical implications. In the paper, they described their own technique for urinary stones treatment: 1) accurate preoperative study of the clinical case, by performing a CT scan completed with stone density measure (Hounsfield scale); 2) first stage contact laser Low Energy/High Frequency lithotripsy; 3) second stage non-contact laser lithotripsy. The first stage contact lithotripsy is aimed to grind stones to dust and smaller fragments, while second stage non-contact lithotripsy to complete dusting and producing fine stone residue for spontaneous elimination. The Authors stated that low energy results in smaller fragments and minor stone retropulsion, with less frequent necessity of stone active removal: it implies shorter operative times.
Tracey et al. [13] confirmed the efficacy of LE/HF RIRS executed on 71 patients (82 “renal units”). In this retrospective study, the Authors described their technique: they utilized a 120 W Ho-YAG laser, performing laser lithotripsy by 0.3 J–70 Hz setting for “hard” stones (> 1000 HU), 0.2 J-80 Hz for lower densities (< 1000 HU).
The results demonstrated the feasibility and safety of Ho-YAG dusting approach, with a total operative time of 53 min (range 22–115). Exclusive LE-HF RIRS was executed in 60/71 patients, with an overall SFR of 67.4%. Complications occurred in 11 cases (13%), all classified as Clavien-Dindo ≤ 2.
Pietropaolo et al. in 2018 [14] published their experience about > 15 mm stones lithotripsy using a 100 W Holmium laser (by a 272 μm laser fiber). The settings applied were an energy level of 0.3–0.6 J and a frequency of 20–50 Hz with a long pulse width. The 50 patients’ results reported were a mean operative time of 51 min (similar to other studies), a SFR equal to 93% for first look RIRS and 98% considering second looks. Complication rates were very low. The lack of a clear definition of “stone-free rate” in the text and the lack of a control group could be considered limitations of the study, but this is a further attempt to give solidity to high frequency lithotripsy and to exploit high potency lasers.
Our study represents a further attempt to explore LE-HF RIRS performed using a high power laser, making some changes to previous studies.
The technique that we applied in Group 1 is directly derived from Aldoukhi’s technique [12] with some modifications. We introduced a new step, the second—major fragments removal through retrieval baskets. This phase could give an advantage in those patients with metabolic dysregulation, allowing a complete diagnosis by stone analysis and giving to urologist the chance to prescribe appropriate pharmacologic therapies for prevention of stone genesis. Furthermore, in some cases the shape, the composition and the hardness of the lithiasis make it difficult to complete an effective dusting. The stone retrieval should always be an available choice for endourologist.
As reported in other previous studies [12, 13], the elevation of the frequency of laser pulses is likely to reduce operative time, because frequency could be considered the accelerator of the entire procedure. Some other Authors do not agree with this concept: the raise of frequency can lead to a reduction of visibility during lithotripsy, forcing the surgeon to stop the lithotripsy frequently. Furthermore, fragmentation with higher pulse energy has been associated with faster stone material ablation per unit time [15].
Nevertheless, endo-vision during RIRS is influenced by a number of factors: the model, the quality and the usage of the instrument, the limpidity of the urines, the anatomy and the compliance of the upper urinary tract, the monitor screen resolution, the status of the camera and the presence or not of bleeding from urothelium.
Some further considerations must be discussed about the cost factor of these two energy sources. Except for the laser used, there is not any substantial difference between the techniques in terms of disposable and non-disposable instrumentation. As a consequence, the cost-effectiveness in the two groups depends on the cost of the laser and of the fibers: high-power Ho-YAG lasers are more expensive than low-power devices for sure. On the other hand, also the usage time of all the equipment in operative room, the overall operating time (which means also the number of retreatments) and obviously the complication rate and severity (need for assistance, drugs and surgery) are factors influencing the final cost of the intervention. Therefore, a conclusive assessment on the cost-effectiveness of low- and high-power lasers is far from being actual.
Our results confirmed that LE HF RIRS leads to a statistically significant reduction in terms of operative time, as put in evidence by the comparison between Group 1 and Group 2 (p < 0.05), without any difference in efficacy. The SFRs and the success rates were comparable between the groups, with a better trend in the LE HF group (p = 0.086). We think that this trend could easily become significant by increasing the casuistry of the groups.
The complication rates are comparable between groups and to literature, attesting that high frequency laser impulses do not represent a risk for patients. In Group 1, a light better trend is recognizable respect to “standard” RIRS in terms of severity of complications, although this result cannot be generalized in a rule because of the limitations of our study.
The major limitations that must be declared are the retrospective design and the moderate sample size: both these observations could reduce the weight of evidence of our study.
The distribution of the patients into the groups was decided by the surgeons at the moment of the intervention, without randomization or blinding. Moreover, we must highlight that also the timing of the procedures included in the two groups is not perfectly contemporary: the RIRS of Group 2 (the “control” Group) were performed from January 2016 to September 2020, while the procedures of Group 1 were executed from July 2016 to September 2020. This discrepancy could represent a limitation, because the surgeons’ learning curve could be different in the groups, so the comparison could be not standardized. However, we must declare that the endo-urologists that performed the procedures were already full experienced in January 2016, with a personal RIRS casuistry of at least 150 procedures, and consequently the influence of this bias on the final results could be less important.
Finally, a more precise evaluation of cost-effectiveness in the groups is lacking: it could represent a further element for the surgeon to decide the best approach during preoperative planning.
Conclusions
As shown by results, LE/HF RIRS is a feasible and effective technique, with stone-free and success rates that are at least not inferior to “standard” RIRS; on the contrary success rate seems to have a superiority trend in Group 1, reaching statistical significance. Operative time is significantly reduced in LE/HF Group of treatment and complications seem to be similar in terms of incidence and severity.
Further studies and larger casuistry are needed to confirm the results and to reach indisputable indications on the topic.
Availability of data and material
Available if necessary.
References
Türk C, Skolarikos A, Neisius A, Petrik A, Seitz C, Thomas K, et al (2019) EAU Guidelines. Edn. presented at the EAU Annual Congress Barcelona 2019. ISBN 978-94-92671-04-2
Fiori C, Autorino R (2018) Flexible ureteroscopy for kidney stones in the third millennium: lights and shadows. Minerva Urol e Nefrol 70:543–545. https://doi.org/10.23736/S0393-2249.18.03354-4
Ulker V, Cakmak O, Yucel C et al (2019) The efficacy and safety of bilateral same-session ureteroscopy with holmium laser lithotripsy in the treatment of bilateral ureteral stones. Minerva Urol Nefrol 71(2):174–180
Ahmed I, Mostafa ME, Nader F, Serge C, Sero A (2018) Double-blinded prospective randomized clinical trial comparing regular and moses modes of holmium laser lithotripsy: Preliminary results. Eur Urol Suppl. https://doi.org/10.1016/S1569-9056(18)31815-3
Kronenberg P, Traxer O (2019) The laser of the future: reality and expectations about the new thulium fiber laser-a systematic review. Transl Androl Urol 8:S398-417. https://doi.org/10.21037/tau.2019.08.01
Keller EX, De Coninck V, Doizi S, Daudon M, Traxer O (2019) What is the exact definition of stone dust? An in vitro evaluation. Eur Urol Suppl 18:e484. https://doi.org/10.1016/s1569-9056(19)30363-x
Peng G, Song L, Xie D, Huang J, Zhong Y, Tan W et al (2018) Suctioning flexible ureteroscopic lithotripsy in the oblique supine lithotomy position and supine lithotomy position: a comparative retrospective study. Minerva Urol e Nefrol 70:612–616. https://doi.org/10.23736/S0393-2249.18.03144-2
Dindo D, Demartines N, Claiven PA (2004) Classification of surgical complications. Ann Surg 2:205–213
Bosio A, Dalmasso E, Alessandria E, Agosti S, Pizzuto G, Peretti D et al (2018) Retrograde intra-renal surgery under spinal anesthesia: the first large series. Minerva Urol e Nefrol 70:333–339. https://doi.org/10.23736/S0393-2249.18.02926-0
Çakici Ç, Özok HU et al (2019) Comparison of general anesthesia and combined spinal-epidural anesthesia for retrograde intrarenal surgery. Minerva Urol Nefrol 71(6):636–643
Carobbio F, Zamboni S et al (2020) Role of cultural analysis in patients with indwelling ureteral stent submitted to ureteroscopy for stones. Minerva Urol Nefrol 72(6):755–762
Aldoukhi AH, Roberts WW, Hall TL, Ghani KR (2017) Holmium laser lithotripsy in the new stone age: dust or bust? Front Surg 4:57. https://doi.org/10.3389/fsurg.2017.00057
Tracey J, Gagin G, Morhardt D, Hollingsworth J, Ghani KR (2018) Ureteroscopic high-frequency dusting utilizing a 120-W holmium laser. J Endourol 32:290–295. https://doi.org/10.1089/end.2017.0220
Pietropaolo A, Jones P et al (2019) Role of ‘dusting and pop-dusting’ using a high-powered (100 W) laser machine in the treatment of large stones (≥ 15 mm): prospective outcomes over 16 months. Urolithiasis 47:391–394
Kronenberg P, Somani B (2018) Advances in lasers for the treatment of stones—a systematic review. Curr Urol Rep 19:45
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peretti, D., Dalmasso, E., Pecoraro, A. et al. Low-energy high-frequency Ho-YAG lithotripsy: is RIRS going forward? A case–control study. Urolithiasis 50, 79–85 (2022). https://doi.org/10.1007/s00240-021-01282-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-021-01282-2