Abstract
This study describes and evaluates the use of non-contrast enhanced computerized tomography (NCCT) before and after extracorporeal shockwave lithotripsy (SWL). Computer measured stone volume was used as an exact measurement for treatment response. 81 patients received SWL of kidney stones at Herlev Hospital between April 2013 and January 2014 and follow-up was possible in 77 (95 %) patients. NCCT was used before and after treatment. Treatment response was expressed as a reduction of the stone volume. Stone characteristics as the stone volumes, HU, SSD and localization were measured by radiologist using a vendor non-specific computer program. Complications, patient characteristics and additional treatment were registered. On average, 5858 shocks were given each patient. The follow-up NCCT was performed 24 days after treatment. It was possible to calculate the stone volume in 88 % of the patients—the remaining 12 % it was not possible due to stone disintegration. The stone free rate was 22 %. The average relative reduction in stone burden was 62 %. Only 8 % of the patients were radiological non-responders. Steinstrasse was observed in 13 (17 %) and 28 (36 %) patients had additional treatment performed. Irradiation dose per NCCT was 2.6 mSv. Stone volume could be calculated in most patients. The relative reduction in stone burden after treatment was 62 %. The stone volume was redundant when evaluating stone free patients, but in cases of partial response it gave an exact quantification, to be used in the further management and follow-up of the patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The unchallenged accuracy of non-contrast enhanced computerized tomography (NCCT) in the diagnostics of urolithiasis is well known and has been adapted into most clinical settings [1], whereas treatment control often involves less sensitive and specific imaging modalities. NCCT provides information regarding the extension and location of the stone disease and thereby provides a sound basis for selecting treatment modality together with the clinical history and symptoms.
Extracorporeal shockwave lithotripsy (SWL) is an ideal treatment option for radiopaque stones within the renal pelvis and upper or middle calices when stone diameters are 2 cm or less [2, 3]. Poorer response rates have been reported for lower calyx stones [3], Hounsfield units (HU) over 1000 [4] and skin-to-stone distance (SSD) over 10 cm [4]. When evaluating the SWL treatment the preferred examination is often a plain X-ray of kidney, ureter and bladder (KUB) [5]; however, it has been shown that residual stone fragments in the kidney and ureter will be overlooked when using a KUB [6] and complications such as sub-capsular hematoma will remain undetected.
To ensure a more accurate evaluation of stone treatment, the department of Radiology at Herlev Hospital, Denmark, has performed routine follow-up with NCCT since 2010. This was done to confirm the quality of treatment and to provide the optimal follow-up. The post-treatment NCCTs are presented at a weekly multidisciplinary conference to design a plan tailored for each patient. We experienced that residual fragments sometimes could be difficult to evaluate if any clearance had occurred. Since stones are three-dimensional (3D) objects we find that computer calculated stone volume could give an exact measurement for the reduction of the stone burden [7, 8]. In this study, the aim is to describe and evaluate the systematic use of 3D computer calculated stone volume before and after SWL of renal stones.
Materials and methods
After permission from the Danish Data Protection agency was granted, patients who received SWL treatment at Herlev Hospital between April 2013 and January 2014 were retrospectively identified. A total of 99 consecutive patients were selected and 18 patients with ureter stones were excluded. Follow-up was only possible in 77 out of the remaining 81 patients (95 %).
The treatment was done by the same electromagnetic lithotripter, Modulith SLX-MX (Karl Storz, Kreuzlingen, Switzerland) under fluoroscopy. The standard pulse frequency was 60 shockwaves per minute and a maximum of 3000 shocks per treatment session. The first 1000 shockwaves were given with an energy level of 16 kV (0.54 mJ mm−2) and increased to 18 kV (0.82 mJ mm−2) the rest of the treatment session. The last 500 shocks were given with an increased frequency of 90 shockwaves per minute. During the procedure the patients received a mild intravenous sedation with midazolam and alfentanil. A series of two to three sessions were pre-booked for each patient with a minimum of a week’s interval. If the stone(s) no longer could be identified with the fluoroscopy, the session was cancelled and the patient was booked for a NCCT and a renogram 3–4 weeks later. If the patient contacted the department between the treatment sessions with symptoms the NCCT was brought forward. The renograms were carried out before and after treatment. This provided a benchmark for renal function and facilitated the identification of potential reduction in the renal function due to complications that arose due to the treatment.
Non-contrast enhanced computerized tomography was used to both diagnose and verify treatment effects. Stone characteristics such as stone volume, maximum stone diameter, peak HU (using 50 % region of interest, ROI), average HU (using 100 % ROI), skin-to-stone distance (SSD) and localization were measured retrospectively by radiologist using a vendor non-specific computer program (Philips Intellispace “CT-viewer”). Stone segmentations were done with fixed HU limit values on “bone window” (Center 800 HU and Width 2000 HU). The radiologist then marked the stone(s) and the software segmented all voxels with HU > 100 and the total stone volume was calculated by adding all the voxels in the region. This process took the radiologist a maximum of 3 min extra for each CT.
The CT planning image (CTI), also called scout, was assessed for radiopaque stones. If no visual stones were identified by visual impression, a localizing scout line was used to help identify radiopaque stones. The patients with no radiopaque stones on CTI had either a KUB or fluoroscopy on the table of the lithotripter to evaluate the possibilities for SWL. The pre-treatment NCCT was performed less than 3 months prior to treatment start. The number of days from the last treatment to the control NCCT was registered together with the irradiation dose per NCCT.
The following data were retrospectively collected from patient files: gender; age; body mass index (BMI); number of treatment session; number of shocks; and complications. The needs for additional stone treatments were registered with respect to both steinstrasse as well as failed treatment response to SWL.
Results
There were 77 patients treated and followed-up; 39 females and 38 males. Mean age was 54.2 years (SD 16.6) ranging from 18 to 88 years. Mean BMI was 25.7 kg m−2 (SD 4.2), ranging from 17.2 to 42.3 kg m−2. Patient characteristics, including stone and treatment features are listed in Table 1. Stone size is presented as the maximum stone diameter measured on the bone window, which is the traditional way to express stone size in clinical practice. The mean stone size was 8.6 mm (SD 2.7) and ranged from 3 to 15 mm.
The mean number of treatment sessions was 2.0 (SD 1.1) and the total number of shocks was 5858 (SD 3037). The post-treatment NCCT was performed on average 24.2 (SD 19.5) days after last SWL session, varying from 1 to 147 days depending on individual patient symptoms and compliance to the given appointments. Nine patients (11.7 %) were pre-stented due to obstructive stones and three patients (3.9 %) were diverted with a percutaneous nephrostomy before treatment due to obstructing stones combined with severe infection.
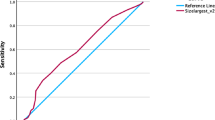
Stone volume accurately describes the stone burden; however, most clinicians have not developed a frame of reference on the stone volume yet. The average stone volume was 608 mm3 (SD 499) before SWL. The variation in stone volume was very large—ranging from 43 to 2131 mm3. To evaluate the SWL treatment effect, both the relative and absolute reduction of the stone volume was calculated. This was possible for 68 patients (88 %) and the results are presented in Fig. 1. The average relative reduction of stone burden was 62 %. In four patients (5 %), there was an increase in stone volume most likely due to micro-fragmentation of a crushed stone. Figure 2 is a magnified 3D picture where the former smooth stone shows clear irregularities due to micro-fragmentation. This phenomenon with an increased stone volume was the same as sometimes observed under fluoroscopy during SWL treatment when a stone changes in size, shape and density.
Disintegration was seen in the remaining nine patients (11.7 %) and stone volume after treatment was not reported due to the well-known inherent CT-error called “volume averaging effect” or “blooming” [9], causing the software to add visible inter-fragmental volumes. In these cases the numerous stone fragments were in very close proximity and the software could not differentiate between each fragment. Figure 3 shows an example of a post treatment CT, where stone volume calculation is erroneous due to fragmentation into gravel.
SWL treatment efficiency has yet to be defined, when controlling treatment response with the high accuracy of NCCT. A 100 % reduction in the stone burden is the optimal result for the patient. The number of patients for whom this occurred was 17 (22 %), however, this information could be acquired by a simple visual evaluation of the NCCT without stone volume measurements. The stone volume data first becomes relevant in the cases with residual fragments. Residual fragments less than 5 mm in maximum diameter have traditionally been considered as clinically insignificant [10, 11], despite that fact that fragments of this size can cause adverse symptoms and regrowth. Figure 1 shows that there has been a response in stone volume in a great number of patients. Responses between ±10 % were considered as non-responders and this group consisted of 6 patients (8 %). The rest of the patients—including the patients with defragmented stones without post-treatment stone volume—had a response to treatment. The response was not satisfactory in 19 (25 %) patients, who subsequently received retrograde intra renal surgery (RIRS) (Table 2). The stone volume in the patients receiving additional renal stone treatment was on the post-SWL NCCT on average 348 mm3 (SD 423), but with a very large range spanning 28–1625 mm3. Stone volume alone was not a suffice indication for surgical treatment. The location of stone fragments together with the patients’ preferences and symptoms were also essential for assessing the necessary additional treatment.
The assessment of visible stones on the CTI before and after treatment is presented in Fig. 4. There were 64 patients (83 %) with and 13 patients without radiopaque stones on the pretreatment CTI. An additional KUB or fluoroscopy identified radiopaque stones in the 13 CTI negative patients. After treatment, 17 patients were stone free and were true CTI negative. The NCCTs showed 47 patients (73 %) with residual fragment. When evaluating these patients’ CTIs there were 22 patients (47 %) with and 25 patients (53 %) without radiopaque residual fragments. Among the patients, the sensitivity of the CTI dropped from 83 % before treatment to 47 % post treatment. This illustrates the possible overestimation of the treatment response when using a less sensitive modality.
Residual fragments in the ureter were not included in the posttreatment stone volume, because these fragments were expected to be cleared either spontaneously or surgically. Steinstrasse was clinically observed in 13 patients (17 %) and 7 (54 %) of these had required semi-rigid ureteroscopy to remove the residual fragments and 1 (8 %) had ureteroscopy combined with RIRS. Two patients with residual fragments in the ureter had semi-rigid ureteroscopy, due to lack of clearance of the fragments, but did not at any time have steinstrasse. The group of patients with steinstrasse had an average stone volume of 726 mm3 (SD 374) before SWL while in the group without steinstrasse the average was 584 mm3 (SD 516). The clearance of fragments in the group with steinstrasse was significantly different from the rest of the patients: 578 mm3 (SD 357) compared to 393 mm3 (SD 443), respectively.
A renogram was performed on all patients before the SWL treatment was initiated. The reference interval for the relative renal function share was 42–58 %. Before treatment 14 patients had a reduced function on the affected side (<42 %)—3 due to obstruction and the rest due to chronical reduced renal function. After treatment 73 of the patients had a new renogram made and 8 patients had a loss of relative renal function of 8 % or more—7 had an obstructing curve. Six patients required surgical intervention due to loss of relative renal function.
The complications are listed in Table 2 and classified according to the Clavien–Dindo classification of surgical complications [12]. No sub-capsular hematoma was observed and 3 patients (4 %) reported hematuria and 3 patients (4 %) were readmitted to the hospital due to infections. 24 patients (31 %) reported pain after treatment, mostly due to stone passage.
Average radiation dose per NCCT was 2.6 mSv (SD 1.2) ranging from 1.0 to 7.8 mSv. Irradiation dose was slightly above the EAU recommendations of 2 mSv for patients with BMI < 30 [13]. 10 % of the patients in the study had a BMI over 30.
Discussion
Success rates for SWL for kidney stones have been reported for many years from around the world. The rates vary from 13.6 to 91.2 % [14–16] and the control modalities were: KUB [4], ultrasound or KUB [17], ultrasound and/or KUB [18] and NCCT [6]. The case for not using NCCT has been irradiation and availability and cost. The risk of overlooking residual fragments has been shown to be 22 % [6], when using KUB compared to NCCT. Ultrasound has been shown to be insufficient in diagnosing residual fragments, especially in ureters [19]. In our perspective KUB is not reliable enough to give patients accurate information about the stone status, because the visibility of radiopaque stone fragments is not only related to stone density, but also to stone size and body mass. When considering patients with residual stones only 47 % could be identified by CTI. CTI is of course not a proxy for KUB, because the negative predictive value of CTI compared to KUB has been shown in another case series to be 67 % [20].
Recent developments have resulted in the necessary irradiation dose given during a NCCT decreasing considerably. The current dose was 2.6 mSv and it is possible to reduce the dose further—approaching a KUB-level—with new CT-scanners and software [21]. In our study we used the bone window to calculate the stone volume. There is an easier way to calculate the stone volume, but it requires that the NCCTs were carried out with a CT-scanner from the same manufacturer. In 17 patients (22 %) the pre-treatment NCCT was performed in another hospital or on a CT-scanner from another manufacturer, which hindered the use of the software program. In these cases, a radiologist calculated stone volumes based on the bone window, which was more time consuming compared to the software-based calculation. We found that the stone volume estimated from both approaches was the same.
Stone volume becomes important in patients that are not stone free after treatment. The partial response can be calculated and presented to the patient as a relative reduction, facilitating patient comprehension of treatment process. Even when a patient decides for a conservative treatment of residual stone fragments it is possible to follow the patient with control NCCT and associated stone volume calculations to evaluate the progression or regression of the stone burden.
Stone volume can be used to calculate the absolute reduction of the stone burden. The patients with steinstrasse had both larger initial stone volume compared to the patients not having steinstrasse, however the differences were not statically significant. The patients with steinstrasse had significantly larger absolute reduction of stone volume compared with the rest of the patients. Using stone volume opens new ways of following treatment success. Stone volumes can easily be adapted into the follow up for other stone treating modalities such as RIRS and percutaneous nephrolithotomy (PCNL). The down side of using stone volume as measures of treatment success can be that patients may become focused on the data generated and demand further treatment, despite not being necessary. To circumnavigate this it will be necessary to identify and inform about clear thresholds for determining treatment in future.
The question that remains is when is the ideal timing for making the follow-up NCCT? In our study the number of days from last treatment was 24. The local guidelines recommends 3–4 weeks, but patients contacting our department with symptoms, mainly painful stone passages or infection, the NCCT was done earlier than the 3–4 weeks. The clearance of both of stone fragments from the kidney and the ureter has been shown to be greater over time [22]. Many studies of SWL with follow up KUB have been done 2–6 weeks after treatment [4, 23]. However, in pre-stented patients it is important not to exceed 3 months of total stenting period due to encrustations of the stent and the risk of infection combined with having a reduced quality of life due to side effects from a jj-stent or a nephrostomy [24]. The reason for not allowing patients wait longer than 3–4 weeks was to shorten waiting time and sick leave, especially if further stone treatment was required.
In 2008 Bandi et al. concluded that “stone volume is an easily obtainable variable and should be routinely reported as a measure of stone burden for all patients with stones” [25]. However; stone volume reduction has not been reported in the recent published results for stone treatment and it is still possible to publish results without performing a follow up NCCT and only evaluating the results with a KUB [23]. Using systematic NCCT and stone volume determination in the follow-up [26] will provide new perspectives on how to report treatment results and define success criteria.
The stone volume in this study was measured retrospectively and has not been used in the clinical decision-making for this group of patients. So whether the potential impact of decisions made based on stone volume reduction cannot be assessed. We can however show the distribution of stone volume reduction after a consecutive group of patients have been treated with SWL of kidney stone. The radiological response rate of 92 % was surprisingly high and very different from the clinical response rate when taking into consideration the need of 28 (36 %) patients for ancillary procedures (semi-rigid ureteroscopy and RIRS). In 46 of the 48 patients (96 %) not having further stone treatment it was possible to calculate the post-treatment stone volume and the average residual stone burden was 145 mm3 (SD 265) ranging from 0 to 1618 mm3. The large spread of the residual stone burden emphasizes that the aim of treatment is not to create perfect radiological result, but to design the treatment and follow up appropriately. In the future, stone volume will be a tool clinicians can use to understand and to describe the exact treatment response of any stone treating modality.
Conclusion
The use of NCCT before and after SWL made it possible to calculate stone volume and calculate the relative and absolute reduction of the stone burden. However, it was not possible to measure the stone volume in all the post-treatment NCCTs due to 9 (12 %) patients having disintegrated stones, so the computer could not differentiate each stone fragment from each other. The stone free rate in this population was 22 %. The average relative reduction of the stone burden was 62 %. A total of 28 (36 %) patients had additional stone treatment performed.
We recommend NCCT as a control measure after SWL to evaluate the treatment results with great precision and using the NCCT after treatment as a baseline for further follow-up. Stone volume is a tool that can be applied in a large number of patients with partial treatment response. The relative and absolute reductions of the stone burden are primarily instruments provided by the radiologist to the urologist to make ideal follow up for the patients.
References
Niemann T, Kollmann T, Bongartz G (2008) Diagnostic performance of low-dose CT for the detection of urolithiasis: a meta-analysis. AJR Am J Roentgenol 191(2):396–401
Srisubat A, Potisat S, Lojanapiwat B, Setthawong V, Laopaiboon M (2014) Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev 11:CD007044. doi:10.1002/14651858.CD007044.pub3
Ozturk U, Sener NC, Goktug HN, Nalbant I, Gucuk A, Imamoglu MA (2013) Comparison of percutaneous nephrolithotomy, shock wave lithotripsy, and retrograde intrarenal surgery for lower pole renal calculi 10–20 mm. Urol Int. 91(3):345–349. doi:10.1159/000351136 [Epub 2013 Jun 28]
Lee HY, Yang YH, Lee YL, Shen JT, Jang MY, Shih PM, Wu WJ, Chou YH, Juan YS (2015) Noncontrast computed tomography factors that predict the renal stone outcome after shock wave lithotripsy. Clin Imaging. doi:10.1016/j.clinimag.2015.04.010 [Epub ahead of print]
Deters LA, Jumper CM, Steinberg PL, Pais VM Jr (2011) Evaluating the definition of “stone free status” in contemporary urologic literature. Clin Nephrol 76(5):354–357
Küpeli B, Gürocak S, Tunç L, Senocak C, Karaoğlan U, Bozkirli I (2005) Value of ultrasonography and helical computed tomography in the diagnosis of stone-free patients after extracorporeal shock wave lithotripsy (USG and helical CT after SWL). Int Urol Nephrol 37(2):225–230
Patel SR, Wells S, Ruma J, King S, Lubner MG, Nakada SY, Pickhardt PJ (2012) Automated volumetric assessment by noncontrast computed tomography in the surveillance of nephrolithiasis. Urology 80(1):27–31. doi:10.1016/j.urology.2012.03.009 [Epub 2012 May 10]
Finch W, Johnston R, Shaida N, Winterbottom A, Wiseman O (2014) Measuring stone volume—three-dimensional software reconstruction or an ellipsoid algebra formula? BJU Int. 113(4):610–614 [Epub 2014 Jan 15]
Kroft LJ, de Roos A, Geleijns J (2007) Artifacts in ECG-synchronized MDCT coronary angiography. AJR Am J Roentgenol 189(3):581–591
Cicerello E, Merlo F, Maccatrozzo L (2012) Management of clinically insignificant residual fragments following shock wave lithotripsy. Adv Urol 2012:320104. doi:10.1155/2012/320104. PMCID: PMC3371344
Osman Y, Harraz AM, El-Nahas AR, Awad B, El-Tabey N, Shebel H, Shoma AM, Eraky I, El-Kenawy M (2013) Clinically insignificant residual fragments: an acceptable term in the computed tomography era? Urology 81(4):723–726. doi:10.1016/j.urology.2013.01.011 [Epub 2013 Mar 7]
Clavien PA et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Türk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, Seitz C (2015) Guidelines on urolithiasis. european association of urology. http://uroweb.org/guideline/urolithiasis/. Accessed 12 June 2015
Obek C, Onal B, Kantay K et al (2001) The efficacy of extracorporeal shock wave lithotripsy for isolated lower pole calculi compared with isolated middle and upper caliceal calculi. J Urol 166(6):2081–2085
Turna B, Ekren F, Nazli O et al (2007) Comparative results of shockwave lithotripsy for renal calculi in upper, middle, and lower calices. J Endourol 21(9):951–956
Sozen S, Kupeli B, Acar C, Gurocak S, Karaoglan U, Bozkirli I (2008) Significance of lower-pole pelvicaliceal anatomy on stone clearance after shockwave lithotripsy in nonobstructive isolated renal pelvic stones. J Endourol 22(5):877–881
Geraghty R, Burr J, Simmonds N, Somani BK (2015) Shock wave lithotripsy outcomes for lower pole and non-lower pole stones from a university teaching hospital: parallel group comparison during the same time period. Urol Ann 7(1):46–48. doi:10.4103/0974-7796.148601
Khalil MM (2012) Which is more important in predicting the outcome of extracorporeal shockwave lithotripsy of solitary renal stones: stone location or stone burden? J Endourol 26(5):535–539. doi:10.1089/end.2011.0314 [Epub 2011 Nov 21]
Viprakasit DP, Sawyer MD, Herrell SD, Miller NL (2012) Limitations of ultrasonography in the evaluation of urolithiasis: a correlation with computed tomography. J Endourol 26(3):209–213. doi:10.1089/end.2011.0177 [Epub 2011 Oct 19]
Graumann O, Osther SS, Spasojevic D, Osther PJ (2012) Can the CT planning image determine whether a kidney stone is radiopaque on a plain KUB? Urol Res 40(4):333–337. doi:10.1007/s00240-011-0411-9 [Epub 2011 Aug 18]
Hur J, Park SB, Lee JB, Park HJ, Chang IH, Kwon JK, Kim YS (2015) CT for evaluation of urolithiasis: image quality of ultralow-dose (Sub mSv) CT with knowledge-based iterative reconstruction and diagnostic performance of low-dose CT with statistical iterative reconstruction. Abdom Imaging 40(7):2432–2440. doi:10.1007/s00261-015-0411-2
Sahin C, Kafkasli A, Cetinel CA, Narter F, Saglam E, Sarica K (2015) How do the residual fragments after SWL affect the health-related quality of life? A critical analysis in a size-based manner. Urolithiasis 43(2):163–170. doi:10.1007/s00240-014-0727-3 [Epub 2014 Oct 2]
Bhojani N, Mandeville JA, Hameed TA, Soergel TM, McAteer JA, Williams JC Jr, Krambeck AE, Lingeman JE (2015) Lithotripter outcomes in a community practice setting: comparison of an electromagnetic and an electrohydraulic lithotripter. J Urol 193(3):875–879. doi:10.1016/j.juro.2014.09.117 [Epub 2014 Oct 8]
Bigum LH, Spielmann ME, Juhl G, Rasmussen A (2015) A qualitative study exploring male cancer patients’ experiences with percutaneous nephrostomy. Scand J Urol 49(2):162–168. doi:10.3109/21681805.2014.938694 [Epub 2014 Dec 1]
Bandi G, Meiners RJ, Pickhardt PJ, Nakada SY (2009) Stone measurement by volumetric three-dimensional computed tomography for predicting the outcome after extracorporeal shock wave lithotripsy. BJU Int. 103(4):524–528. doi:10.1111/j.1464-410X.2008.08069.x [Epub 2008 Oct 31]
Selby MG, Vrtiska TJ, Krambeck AE, McCollough CH, Elsherbiny HE, Bergstralh EJ, Lieske JC, Rule AD (2015) Quantification of asymptomatic kidney stone burden by computed tomography for predicting future symptomatic stone events. Urology 85(1):45–50. doi:10.1016/j.urology.2014.08.031 [Epub 2014 Oct 22]
Acknowledgments
Thanks to Colin A. Stedmon for final language revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Bigum, L.H., Ulriksen, P.S. & Omar, O.S. Using a three-dimensional computer assisted stone volume estimates to evaluate extracorporeal shockwave lithotripsy treatment of kidney stones. Urolithiasis 44, 451–457 (2016). https://doi.org/10.1007/s00240-016-0864-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-016-0864-y